Endometrial Biopsy versus Curettings versus Cytology
Anna Sienko MD
Greater than 90% of patients with endometrial lesions, either nonneoplastic or neoplastic, present clinically with abnormal uterine bleeding and postmenopausal bleeding. Assessing the cause for the abnormal uterine bleeding or postmenopausal bleeding necessitates endometrial tissue sampling for histopathologic evaluation and appropriate treatment planning. In patients with postmenopausal bleeding, approximately 10% will be diagnosed with endometrial carcinoma upon further investigation.1 Tissue sampling of the endometrium includes invasive and noninvasive methods. Invasive procedures include endometrial curetting (dilatation and curettage [D&C]), endometrial biopsy or hysteroscopy, and directed biopsy.2 Evaluation of the endometrium by noninvasive methods includes procedures performed by transvaginal ultrasound and endometrial cytology (direct sampling). In 5% of asymptomatic women, endometrial cells will be found in Papanicolaou (Pap) tests in routine cervical screening as an incidental finding. Follow-up and additional investigations are recommended in patients with “abnormal endometrial cells” in a Pap test and in all patients 40 years of age and older (see Chapter 11).3,4
DILATATION AND CURETTAGE
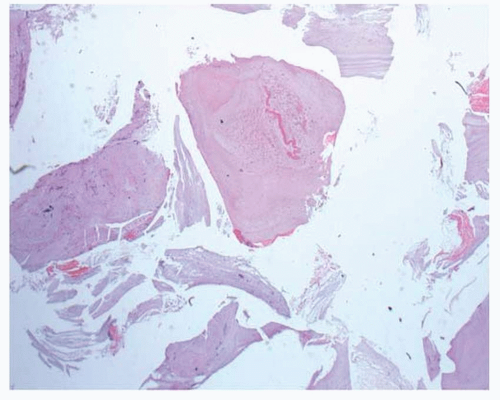
In the past, endometrial tissue sampling was most often performed as a D&C procedure, and D&C is still considered the “gold standard” for investigation of abnormal uterine bleeding, especially in postmenopausal patients and patients with endometrium thickness of 5 mm or more by transvaginal ultrasonography.5,6 D&C is an invasive procedure that requires operating room time with general anesthesia. Although many different types of sampling devices are available, the procedure is similar and entails insertion of a curette into the endometrial cavity through a vaginal speculum and gradual dilatation of the cervix. The curette has a hollow head, which is often “spoon shaped.” Some curetting devices may also have a longitudinal slot through which the endometrial sample is suctioned into the curetting head. The sample is obtained by rotating the curette and scraping the top layer of endometrium (Figs. 13-1 and 13-2).
Sampling Issues with Dilatation and Curettage
D&C sampling is performed “blind,” without direct visualization of the uterine cavity, and is limited, with only 30% to 60% of the endometrial cavity sampled.5 Comparison studies of endometrial tissue sampling obtained by D&C and hysterectomy specimen showed that
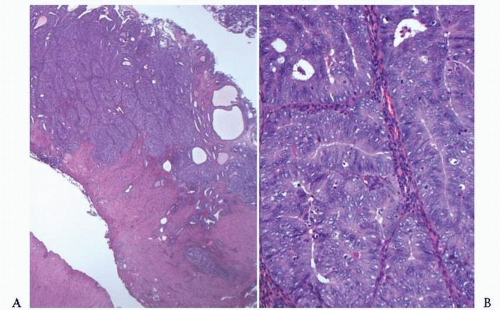
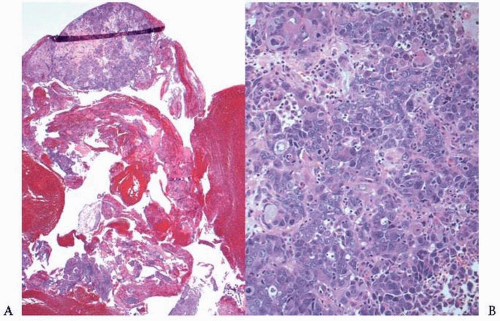
D&C undersampling can occur with lesions that are focal, exophytic, or endophytic.7,8 In endometrial lesions that were diffuse, D&C had a high yield, with a greater than 92% to 94% detection rate of hyperplasia and carcinoma (Fig. 13-3).5 D&C tissue sampling was also found to be limited in patients with endometrial thickness of ≤4 mm by transvaginal ultrasonography (Fig. 13-4).6 Because D&C only “scrapes” the top layer of endometrium for sampling, depth of tumor invasion cannot be ascertained, and accurate staging cannot be performed by this method. Thus, the tissue sample obtained by D&C sampling and the tumor grading of that sample would be the most measurable and heavily used parameter for preoperative
evaluation in surgical planning and staging. However, the tumor grade has been found to be underestimated in tissue sampling by D&C in more than 25% of patients, with a higher grade found on hysterectomy specimen in more than 10% of patients.5,9,10
D&C undersampling can occur with lesions that are focal, exophytic, or endophytic.7,8 In endometrial lesions that were diffuse, D&C had a high yield, with a greater than 92% to 94% detection rate of hyperplasia and carcinoma (Fig. 13-3).5 D&C tissue sampling was also found to be limited in patients with endometrial thickness of ≤4 mm by transvaginal ultrasonography (Fig. 13-4).6 Because D&C only “scrapes” the top layer of endometrium for sampling, depth of tumor invasion cannot be ascertained, and accurate staging cannot be performed by this method. Thus, the tissue sample obtained by D&C sampling and the tumor grading of that sample would be the most measurable and heavily used parameter for preoperative
evaluation in surgical planning and staging. However, the tumor grade has been found to be underestimated in tissue sampling by D&C in more than 25% of patients, with a higher grade found on hysterectomy specimen in more than 10% of patients.5,9,10
ENDOMETRIAL BIOPSY (PIPELLE)
Many different types of instruments for endometrial sampling have been developed as an alternative to inpatient procedures for evaluation of abnormal uterine bleeding. These office outpatient procedures do not require operating room time or general anesthesia and are more cost effective than a D&C procedure. All are based on aspiration sampling of the endometrium. The sample is obtained by introducing into the uterine cavity, through a vaginal speculum, a flexible or rigid hollow sheath (Pipelle; Unimar, Wilton, CT) inserted up to the fundus; suction is generated (via internal piston, vacuum syringe, or vacuum pump), and the sheath is rotated and moved back and forth as it is withdrawn. Tissue is “sucked” into openings at the “head tip” of the sheath and into lumen of the sheath.11,12
Issues with Endometrial Biopsy
The Pipelle is currently the most commonly used and most studied device for office outpatient endometrial sampling.1 The problems and issues with the Pipelle and similar devices are predominately based on sample tissue size. Adequate samples consisting of one or more pieces large enough and intact enough for histopathologic interpretation were obtained in 87% to 99% of patients according to several studies.5,13,14 A diagnosis of endometrial adenocarcinoma was made in 67% to 98% of samples.1,13,14 Inadequate specimens with scant tissue for evaluation were obtained from 12% to 22% of patients who were menopausal or had cervical stenosis, with an overall false-negative rate of up to 15%.1,13,15




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree