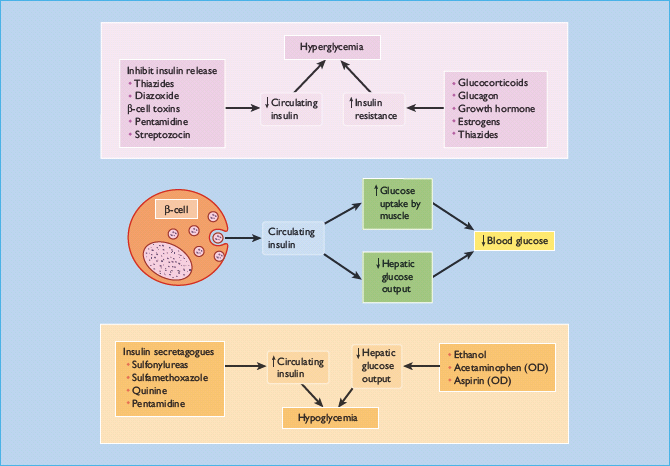
- Many drugs interfere with glucose homeostasis or interact with antidiabetic agents and thus can disturb glycemic control in people with diabetes. Specific diabetic complications, such as nephropathy and neuropathy, may require particular drugs to be used with care.
- Hyperglycemia can be caused or worsened by numerous drugs. Those that induce insulin resistance include glucocorticoids, certain oral contraceptives, antipsychotic drugs, HIV protease inhibitors, the fluoroquinolone gatifloxacin and β-adrenoceptor antagonists. Diabetogenic drugs that damage the β-cell include pentamidine and cyclosporine (ciclosporin).
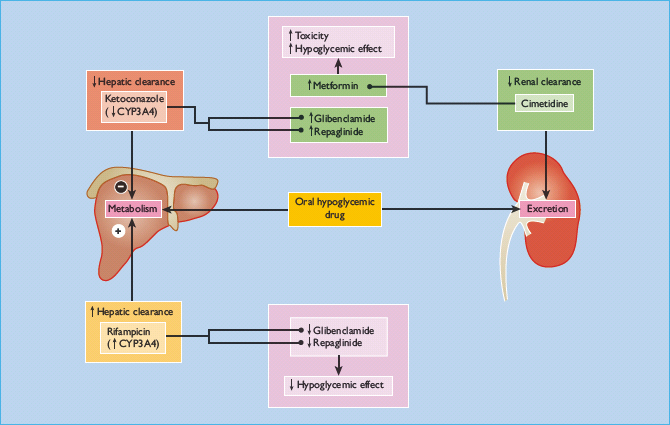
- Sulfonylureas and related agents commonly cause hypoglycemia by interacting with other drugs that block their metabolism in the liver, e.g. ciprofloxacin inhibits CYP2C9, which degrades glyburide (glibenclamide), or that impair renal function and decrease their elimination (e.g. non-steroidal anti-inflammatory agents).
- Hypoglycemia can be induced by drugs that stimulate insulin secretion (e.g. quinine, especially in children with cerebral malaria); and sulfamethoxazole, which binds to the sulfonylurea receptor. Pentamidine can induce transient hypoglycemia, by causing passive loss of insulin from the β-cell, as a prelude to permanent diabetes.
- Hypoglycemia can complicate overdosage with acetaminophen (paracetamol), following hepatic necrosis; or aspirin, which blocks hepatic glucose output and stimulates peripheral glucose uptake. Alcohol inhibits hepatic gluconeogenesis and can provoke, prolong or exacerbate hypoglycemia.
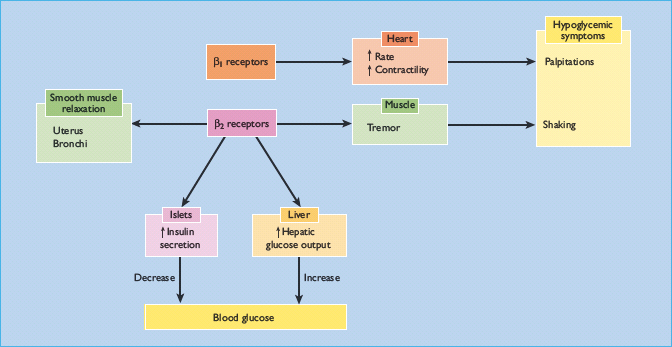
- Non-selective β-adrenoceptor antagonists inhibit insulin secretion and can impair glucose tolerance. They also decrease certain catecholamine-mediated symptomatic and metabolic responses to hypoglycemia; awareness of hypoglycemia may therefore be reduced, and recovery of normoglycemia delayed. These adverse effects are much less pronounced with cardioselective β1-adrenoceptor antagonists.
- Thiazide diuretics used at low dosages (e.g. 2.5mg/day bendroflumethiazide) lower blood pressure effectively and are suitable for use in patients with diabetes.
- Certain drugs require special consideration in patients with diabetic complications. Metformin and several sulfonylureas are cleared through the kidney; they are therefore contraindicated in advanced nephropathy and should not be co-administered with nephrotoxic drugs. Vasodilators and ganglion-blocking agents exacerbate postural hypotension.
This chapter discusses the problems posed by drug therapy in the management of people with diabetes. Numerous drugs can affect diabetic control, causing hyperglycemia or hypoglycemia, by interfering with insulin secretion or action or both, or by interacting with antidiabetic agents. Some important examples are illustrated in Figure 26.1. The special considerations that apply when using other drugs in patients with diabetes and in the presence of specific diabetic complications are also discussed.
Drugs that raise blood glucose concentrations
Drug-induced diabetes is now recognized as a distinct etiologic category, and diabetogenic drugs are discussed in detail in Chapter 16. The main culprits are shown in Table 26.1. Most of these drugs – notably glucocorticoids (a common and important cause of iatrogenic diabetes), contraceptive steroids and β-adrenoceptor antagonists – act by inhibiting insulin action. By contrast, insulin secretion is inhibited by diazoxide, while pentamidine can cause permanent β-cell damage. In recent years, antipsychotic drugs, HIV protease inhibitors and the fluoroquinolone antibiotic gatifloxacin have emerged as important causes of hyperglycemia.
Table 26.1 Drugs that may cause or exacerbate hyperglycemia.
| Potentially potent effects | Minor or no effects |
| Glucocorticoids | Oral contraceptives |
| Oral contraceptives | Progestogen-only pills |
| High-dose oestrogen | Levonorgestrel in combination pills |
| Thiazide diuretics (especially high dosages)* | Loop diuretics |
| Non-selective β-adrenoceptor antagonists | Calcium-channel blockers |
| β2-Adrenoceptor agonists | α1-Adrenoceptor agonists |
| Salbutamol | Growth hormone (physiologic doses) |
| Ritodrine | Somatostatin analogst |
| Antipsychotics | Androgen deprivation therapy for prostate cancer |
| HIV protease inhibitors | Selective serotonin reuptake inhibitors |
| Indinavir, nelfinavir, ritonavir and others | Nicotinic acid |
| Others | Lamivudine |
| Pentamidine | Isoniazid |
| Gatifloxacin | |
| Streptozotocin | |
| Diazoxide | |
| Cyclosporine (ciclosporin) | |
| Tacrolimus | |
| Temsirolimus | |
| Interferon-α | |
| L-Asparaginase |
* “High” dosages of thiazides correspond to >5mg/day bendrofl umethazide.
† Somatostatin analogs may induce hyperglycemia in type 2 but not type 1 diabetes.
Drugs that lower blood glucose concentration
Many drugs can cause hypoglycemia (Table 26.2) [1–10]. These include some that interact with and enhance the action of glucose-lowering drugs. Others act in their own right as insulin secretagogues, or to enhance or mimic the effect of insulin in suppressing glucose production by the liver and stimulating glucose uptake into peripheral tissues. Some drugs (e.g. nonselective β-adrenoceptor antagonists) specifically block the warning symptoms or the neuroendocrine counter-regulatory responses that are normally triggered by hypoglycemia, and so can prolong and intensify hypoglycemic episodes.
Table 26.2 Drugs that may cause or exacerbate hyperglycemia.
Antidiabetic drugs Insulins Sulfonylureas, e.g. glimepiride Repaglinide Drugs that interact to enhance the actions of sulfonylureas (Table 26.4) Quinolone antibacterials: Levofloxacin, gatifloxacin [4] Corticosteroids, including inhaled corticosteroids (when withdrawn may lead to adrenal insufficiency) [5,6] Other drugs Aspirin (in overdosage) Cibenzoline Disopyramide Doxycycline [7,8] Etanercept Ethanol Hydroxychloroquine Imatinib Mefloquine Non-selective β-adrenoceptor antagonists Paracetamol (in overdosage) Pentamidine Quinidine Quinine Sulfamethoxazole (in co-trimoxazole) Valproate (in neonates exposed in utero) [9] Venlafaxine (in overdosage) [10] |
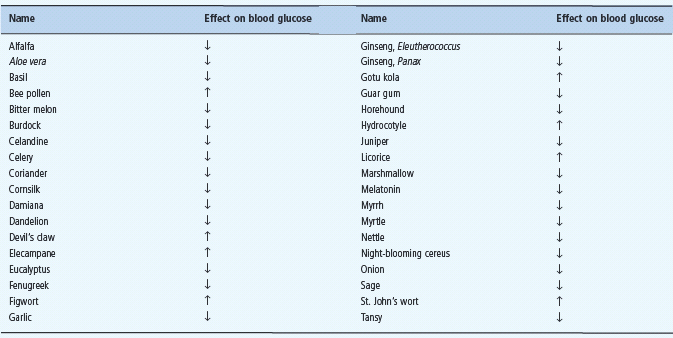
Drugs should always be suspected whenever patients with previously well-controlled diabetes experience unexplained hypoglycemic episodes, or if dosages of insulin or oral hypoglycemic agents decline. As well as prescription drugs, patients should be asked about herbal, traditional and other alternative medicines. These are now widely used by people with diabetes – up to one-third of patients in one study [11] –and some products may contain naturally occurring or synthetic glucose-lowering agents (Table 26.3).
Table 26.3 ome herbal medicinal products and food supplements that can potentially interact with antidiabetic drugs to affect blood glucose concentrations. Data from Ernst E. The Desktop Guide to Complementary and Alternative Medicine.An Evidence-Based Approach. Edinburgh: Mosby, 2001.
Sulfonylureas
Sulfonylureas are an important and sometimes unrecognized cause of symptomatic hypoglycemia (see Chapter 33). They are also affected by numerous interactions with other drugs (Figure 26.2).
The long-acting sulfonylureas glibenclamide and chlorpropa-mide are especially troublesome. In one outpatient survey, 20% of patients treated with glibenclamide reported symptoms of hypoglycemia within the previous six months [12]. while other surveys suggest that tolbutamide is much less likely to cause severe hypoglycemia (i.e. requiring hospital admission) than either glibenclamide or chlorpropamide [13,14]. A Swiss study [15] defined the risk of severe hypoglycemia as two episodes per 1000 persons per year in those given glibenclamide, over twice as high as in those taking shorter-acting sulfonylureas such as tolb-utamide, gliclazide or glipizide. The novel sulfonylurea, glimepiride, is said to carry a relatively low risk of hypoglycemia because it binds to a different site on the sulfonylurea receptor from classic sulfonylureas and also has distinct pharmacokinetic properties. None the less, the rate of hypoglycemia is still substantial, with 10–20% of patients experiencing at least one mild episode each year [16].
Several factors other than the individual drug per se can increase the risk of hypoglycemia from sulfonylureas, notably increasing age and renal impairment [13,14,16–18]. Reduced food intake during intercurrent illness can also contribute [17,18]. Drug interactions that enhance the action of sulfonylureas are considered below.
Not all those who have sulfonylurea-induced hypoglycemia are patients with type 2 diabetes (T2DM): “bystanders” have included toddlers who ate a grandparent’s tablet [19], nursing-home residents given the treatment of other patients [20] and people whose prescriptions for other drugs have been misread [21].
Sulfonylurea-induced hypoglycemia can be profound and prolonged, and difficult to manage. Patients with sulfonylurea-induced hypoglycemia may require admission and treatment with glucose until the effect of the sulfonylurea has worn off although caution is needed as indicated in the case report below. Insulin hypersecretion induced by sulfonylureas can be suppressed effectively with either diazoxide (which opens the β-cell KATP channel that is closed by sulfonylureas) [22,23] or by the somatostatin analog octreotide [24].
A 62-year-old woman was admitted with acute confusion and became unresponsive 2 hours after admission. She had type 2 diabetes with impaired renal function (serum creatinine 176u.mol/L) and had been taking 40mg gliclazide twice a day. Her blood glucose concentration was 1.8 mmol/L. The hypoglycemia was reversed with an intravenous bolus of 50 mL 50% glucose but subsequently she had repeated episodes of hypoglycemia and required continuous intravenous glucose infusion for 3 days. A blood sample taken when she was hypoglycemic showed raised serum insulin and C peptide concentrations, indicating increased insulin secretion. This patient had impaired renal function. It is likely that this caused gliclazide to accumulate, leading to hypoglycemia. Intravenous glucose restored consciousness, but also stimulated further insulin secretion, leading to further episodes of hypoglycemia.
Adapted from Langford et al. Postgrad Med J 2003; 79:120.
Other a ntidiabetic a gents
These are described in Chapter 29.
- Metformin used alone is not expected to cause hypoglycemia in therapeutic use; but instances of “hypoglycemia” were reported by the UK Prospective Diabetes Study (UKPDS) during metformin treatment [25]. They were not generally confirmed by blood glucose measurements.
- Thiazolidinediones (e.g. rosiglitazone and pioglitazone) potentiate the peripheral actions of insulin. They do not induce hypoglycemia in their own right, but can enhance hypoglycemia caused by sulfonylureas or insulin when used in combination with them.
- Repaglinide stimulates insulin release by a mechanism distinct from that of the sulfonylureas and so causes hyperinsulinemic hypoglycemia. A case of factitious hypoglycemia from repaglinide has been reported [26].
- Acarbose inhibits intestinal disaccharidase, and so reduces the hydrolysis of sucrose and thus glucose absorption. It does not cause hypoglycemia when used as monotherapy. Acarbosetreated patients who develop hypoglycemia from other glucose-lowering drugs should be warned that oral glucose, not sucrose, is needed to treat the episode.
- Exenatide and liraglutide are incretins, that is, peptide hormones that enhance the pancreatic insulin response to glucose in the gut. They are agonists of the glucagon-like peptide-1 (GLP-1) receptor. They slow down stomach emptying and stimulate insulin secretion. Unlike insulin, they do not tend to cause hypoglycemia. They also increase pancreatic p-cell mass and promote weight loss. The major disadvantages are nausea, the need for subcutaneous injections, and the high cost relative to sulfonylureas.
- Gliptins increase the circulating levels of incretins by inhibiting dipeptidyl peptidase 4 (DPP-4), the enzyme that breaks down incretins and other peptides. The oral route of administration is an advantage, but the long-term effects of DPP-4 inhibition remain unknown. Exenatide and gliptins are indicated for glycemic control as alternatives to thiazolidinediones or acarbose in patients with T2DM on metformin therapy in whom a sulfonylurea is not tolerated or inappropriate.
- Inhaled insulin preparations deliver insulin by the pulmonary route, and have a value in patients who have a phobia of needles. Because of poor sales and safety concerns, the first inhaled insulin marketed has been withdrawn. There could be a revival of interest in inhaled insulin if long-acting formulations become available.
Other drugs
Antimicrobials
- Quinine and quinine derivatives. Patients with falciparum malaria are often extremely ill, and may have hypoglycemia because of the effects of cytokines and malnutrition, both of which diminish hepatic gluconeogenesis. In this context, it is easy to overlook quinine-tnduced hypoglycemia, which can be profound, especially in children [27,28]. It is caused by insulin hypersecretion, as quinine has insulin secretagogue activity [29]. Octreotide (a long-acting somatostatin analogue) has been used successfully to inhibit insulin release and raise blood glucose concentrations under these conditions [30]. Quinidine and mefloquine may occasionally cause hypoglycemia, while chloroquine does not [28].
- Sulfamethoxazole, which is combined with trimethoprim in co-trimoxazole, has a sulfonylurea-like action and can stimulate insulin secretion; several cases of severe hypoglycemia have been described [31]. This tends to be long-t asting, perhaps because excessive amounts of glucose solution are infused; this may paradoxically worsen hypoglycemia by further stimulating insulin secretion. Elderly patients receiving high dosage, and patients in renal failure (which causes the drug to accumulate) are at particular risk [32], as are patients infected with HIV who receive high doses of co-trimoxazole to treat Pneumocystis jirovecii pneumonia (formerly known as Pneumocystis carinii) [33].
- Pentamidine, a drug used to treat and prevent P. jirovecii pneumonia, can also damage pancreatic β-cells. This initially leads to the passive leakage of insulin out of secretory vesicles, causing hypoglycemia, but diabetes may develop subsequently [34]. In two series of patients with HIV treated with pentamidine, 25% [35] and 14% [36] developed symptomatic hypoglycemia; they invariably developed renal damage from the drug as well. Even inhaled pentamidine can cause hypoglycemia [37].
- Doxycycline has been suggested to cause hypoglycemia, but the reaction is infrequent and no mechanism has been identified [38].
- Quinolones. particularly gatifloxacin, can cause hypoglycemia (and also hyperglycemia). A case-control study defined an adjusted odds ratio for hypoglycemia with gratifloxacin treatment of 4.3 (95% confidence interval [CI] 2.9-6.3) compared with macrolide treatment [4]. There was a small increase in risk with levofloxacin.
Miscellaneous drugs
- Disopyramide and cibenzoline (cifenline), class Ia antiarrhyth-mic agents, can rarely cause symptomatic hypoglycemia; this can occur either with or without hyperinsulinemia [39], suggesting that peripheral effects contribute. In normal subjects, disopyramide produces a small but statistically significant fall in fasting glucose concentration [40]. In a Japanese case–control study, cibenzoline treatment was associated with an eightfold increase in the risk of hypoglycemia; disopyramide did not significantly increase the overall risk, but the confidence intervals were wide [41]. The effect of disopyramide appears to be dose-dependent. In one case, a man developed severe hypoglycemia while taking disopyramide only after starting treatment with clarithromycin for an intercurrent infection [42]; clarithromycin inhibits the hepatic microsomal enzymes that metabolize disopyramide and so greatly increases serum disopyramide concentrations.
- Antidepressants, including monoamine oxidase inhibitors, selective serotonin reuptake inhibitors and nefazodone, have been reported to reduce blood glucose concentrations [43].
Drugs in overdose
- Acetaminophen (paracetamol), in overdose, can cause hypogly-cemia as a complication of acute hepatic necrosis. Overdosage of aspirin and other salicylates inhibits hepatic glucose production and also increases peripheral glucose utilization, leading to hypoglycemia, especially in children. Paradoxically, and for unknown reasons, hyperglycemia can be encountered in adults.
- Ethanol inhibits gluconeogenesis; consequently, it can cause hypoglycemia in children or fasting adults and exacerbate hypoglycemia from another cause even when consumed in relatively modest amounts (see Chapter 24). Results of experimental studies are unclear: modest concentrations of ethanol impaired the growth hormone response to insulin-induced hypoglycemia in volunteers with type 1 diabetes (T1DM), but did not affect glucagon response [44]. The same dose of ethanol impaired glucagon, although not growth hormone (GH), response to the same degree of hypoglycemia in patients with diet-treated T2DM [45]. Rebound hypoglycemia can follow 2–3 hours after drinking alcohol with a glucose load in the form of sweet drinks or foods–so-called “gin-and-tonic hypoglycemia” [46]. Alcohol ingestion also increases the risk of severe brain damage or death in people who take an intentional overdose of insulin [47].
Non-pharmacopoeial drugs
Some “herbal,” “traditional” and “folk” remedies contain compounds with glucose-lowering properties that are generally weak [48]. Some preparations, however, have caused severe hypoglycemia and have been found on analysis to contain an undeclared sulfonylurea [49].
Drug interactions that affect blood glucose concentrations
Several potential mechanisms underlying drug interaction cause hyperglycemia or hypoglycemia. Pharmacokinetic interactions can influence the effective concentrations of a glucose-modifying drug; examples are the increased concentrations of disopyramide following co-administration of clarithromycin, as described above, and the large number of drugs that increase or decrease circulating concentrations of sulfonylureas (see below).
Pharmacodynamic interactions occur when the observed action of one drug is modified by the action of another, without a change in the circulating concentration of either. The drugs can act at the same site (e.g. sulfamethoxazole is a ligand at the SUR-1 sulfonylurea receptor) or at different sites. Examples of the latter include β-adrenoceptor antagonists and other drugs that influence the physiologic response to hypoglycemia, and so alter the duration or severity of hypoglycemia from another cause.
Drugs that interact to enhance the actions of insulin secretagogues
Many drugs have pharmacokinetic or pharmacodynamic interactions with sulfonylureas that can cause clinically important disturbances in glycemic control. Some of the more important examples are shown in Table 26.4 and Figure 26.2. The most common outcome is hypoglycemia, brought about by reduced metabolic or renal clearance. Transient effects from displacement of protein-bound drug may occasionally also be important. Major dangers include the potentiation of the effects of tolbutamide, and possibly of chlorpropamide, glibenclamide and glipiz-ide, by azapropazone (apazone), oral chloramphenicol and fluconazole. Miconazole interacts with glibenclamide and glipiz-ide as well as tolbutamide. All these interactions are secondary to the inhibition of the metabolism of sulfonylurea in the liver. Similarly, ciprofloxacin increases the plasma concentrations and therefore enhances the hypoglycemic action of glibenclamide, apparently by inhibiting the hepatic CYP2C9 enzyme that metabolizes glibenclamide [50].
Table 26.4 Drugs that interact with sulfonylureas.
Drugs that may enhance the hypoglycemic effect of sulfonylureas Azapropazone, phenylbutazone Salicylates Probenecid Sulfonamides Clarithromycin Nicoumalone Fluconazole, ketoconazole, miconazole, voriconazole Drugs that may reduce the hypoglycemic effect of sulfonylureas Rifampicin Chlorpromazine |
By contrast, rifampicin reduces the action of glibenclamide by inducing CYP2C9 and enhancing the hepatic clearance of sulfo-nylurea. Chlorpromazine also decreases the glucose-lowering effect of sulfonylurea, possibly by inhibiting insulin secretion.
Another important interaction with chlorpropamide (and, to a much lesser extent, with other sulfonylureas) is the cutaneous vasodilatation of the face and occasionally the trunk that is induced by ethanol, the chlorpropamide–alcohol flush (see Chapter 29).
Clarithromycin has been reported to interact with glibenclamide and glipizide, leading to hypoglycemia [51].
Some patients may be more susceptible to drug-induced hypoglycemia than others. For example, a Japanese case-control study suggested that patients taking levothyroxine and who also had liver disease were at substantially increased risk of mild hypoglycemia, with an odds ratio of 14.7 (range 1.6–137) [52].
Several oral hypoglycemic agents, including glimepiride, glip-izide, glibenclamide, tolbutamide and nateglinide, are metabolized by CYP2C9, and a study suggests that among other factors, individuals with genetically determined low CYP2C9 activity are at an increased risk of sulfonylurea-associated severe hypoglycemia [53].
A meta-analysis confirms the impression that hypoglycemia is more likely with glibenclamide than other insulin secretagogues (relative risk 1.52 [95% CI 1.21–1.92]) [51].
Surreptitious ingestion of sulfonylureas such as glibenclamide in alternative medicines can cause hypoglycemia [54].
Interactions with metformin
Metformin has a high renal clearance. Cimetidine reduces the renal clearance of metformin, and causes it to accumulate (Figure 26.2). Drugs that impair renal function, such as non-steroidal anti-inflammatory agents and aminoglycosides, should be used with care, as they can also raise metformin concentrations, increasing the risk of lactic acidosis. Metformin should be stopped 24 hours before prolonged fasting (e.g. before surgery) and 48 hours before procedures requiring intravenous radiocontrast media. Patients on metformin are advised to avoid alcohol or to drink in moderation as hepatic damage poses a risk of hypoglycemia and lactic acidosis.
Interactions with other antidiabetic agents
- Rosiglitazone is metabolized by the hepatic microsomal enzyme CYP2C8, raising the theoretical possibility of interaction with other agents metabolized by the same enzyme. These include cerivastatin, now withdrawn in the USA and the UK, and paclitaxel [55], but no clinically significant interactions have yet been reported.
- Repaglinide is metabolized by CYP3A4, which also breaks down glibenclamide and several other important drugs, and is then excreted in the bile. Clarithromycin, an inhibitor of CYP3A4, has been reported to increase repaglinide concentration and the risk of hypoglycemia [56]. Rifampicin, which induces the same enzyme, reduces the effective concentrations of repaglinide by 25% in healthy volunteers, and could potentially worsen glycemic control in patients with T2DM [56]. Repaglinide is also metabolized by CYP2C8, and its plasma concentration is greatly increased by gemfibrozil, an inhibitor of CYP2C8. This interaction can result in hypoglycemia [56].
- Glimepiride is broken down by CYP2C9, and its metabolism is significantly inhibited by fluconazole, thus potentially enhancing its hypoglycemic action [57].
Hazards of general drugs when used in patients with diabetes
The presence of diabetes can influence the choice of agent for treating several important conditions. Drugs to treat cardiovascular diseases–hypertension, angina, arrhythmias and heart failure–and hyperlipidemia are of particular importance, because these conditions are common in people with diabetes.
Drugs with cardiovascular actions
β-Adrenoceptor antagonists
These are useful in the treatment of hypertension, angina, arrhythmias and in some cases of heart failure. There is also evidence that β-adrenoceptor antagonists (beta-blockers) are effective cardioprotective agents that reduce mortality following myocardial infarction in subjects both with and without diabetes [58,59]. β-adrenoceptor antagonists are indicated in patients with chronic heart failure as they improve left ventricular function and reduce mortality [60]. The β-adrenoceptor antagonists should be started in stable patients, at a very low dose which should be escalated gradually.
β-Adrenoceptor antagonists can, theoretically at least, interfere with several aspects of glucose homeostasis (Figure 26.3). In the islets, insulin secretion is enhanced by β2-adrenoceptor stimulation, while the β2-adrenoceptor-mediated response to hypoglycemia in the liver promotes hepatic glycogenolysis and increases hepatic glucose output, a crucial part of the counter-regulatory response that restores blood glucose to normal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree