A monoclonal spike on serum protein electrophoresis is a frequent finding in the general population and pathognomonic of a plasma cell dyscrasia. In otherwise healthy individuals, it is diagnostic of two asymptomatic, premalignant conditions called monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) which carry a lifelong risk of progression to multiple myeloma (MM) or related malignancy. This article discusses the criteria for diagnosis of MGUS, SMM, and MM; current recommendations for follow-up and risk factors for progression to MM of patients with MGUS and SMM; and diagnostic evaluation of suspected MM transformation.
Epidemiology of monoclonal gammopathy of undetermined significance
The nomenclature monoclonal gammopathy of undetermined significance (MGUS) was introduced by Kyle in 1978, and, since then, the fundamental characteristics, natural history, and diagnostic criteria of this condition have been extensively revised. According to the most current International Myeloma Working Group consensus, MGUS is defined by the simultaneous presence of 3 criteria: (1) a monoclonal spike (M spike) of less than 3 g/dL on serum protein electrophoresis (SPEP), (2) bone marrow infiltration by monoclonal malignant plasma cells (PCs) of less than 10%, and (3) the absence of any end-organ damage related to multiple myeloma (MM), the so-called CRAB (hypercalcemia, renal failure, anemia, and bone lesions) criteria ( Table 1 ). Other diseases that can present with an M spike, such as chronic lymphocytic leukemia, B-cell and T-cell lymphomas, chronic myeloid leukemia, and other PC dyscrasias (amyloid light chain [AL] amyloidosis, Waldenström macroglobulinemia [WM], and heavy chain disease) should also be excluded before making a diagnosis of MGUS. Epidemiologic studies in the Olmsted County have estimated that MGUS affects around 3% of individuals aged 50 years or more, with prevalence increasing with age. These data refer to a cohort heavily skewed toward whites, and the 3% figure does not reflect the 2- to 3-fold increased incidence of MGUS in African Americans and blacks from Africa or the decreased incidence in Asians and Mexicans in comparison with the white population. A familial predisposition, with increased risk of MGUS in first-degree relatives of patients with MGUS, has also been observed. MGUS carries a 1%-per-year unremitting, lifelong risk of transformation to hematologic cancer, mainly MM. Clinical research has focused on identifying predictive factors of progression and risk stratification models to provide appropriate patient counseling and guide follow-up.
| Criteria | M Spike | BM | CRAB a | Comments | ||
|---|---|---|---|---|---|---|
| MGUS | <3 g/dL | AND | <10% | AND | Absent | Diagnosis requires exclusion of other lymphoproliferative diseases |
| SMM | ≥3 g/dL | OR | ≥10% | AND | Absent | — |
| MM | Any concentration on SPEP/UPEP or abnormal FLC ratio | AND | Any percentage or presence of plasmacytoma | AND | Present | Truly nonsecretory MM is an exception because an M spike cannot be identified on SPEP, UPEP, or FLC |
| PC Leukemia b | Absent/present | AND | Absent/present | AND | Absent/present | Defined by the presence of peripheral blood circulating clonal PC >2 × 10 9 /L or 20% of leukocytes |
| Solitary Plasmacytoma | Absent c | AND | Absent | AND | Absent | Defined as a single site of abnormal PC proliferation in the bone (osseous) or soft tissue (extraosseous) |
a Hypercalcemia is defined as a total serum calcium level higher than 11.5 mg/dL; renal insufficiency is defined by a serum creatinine level exceeding 2 mg/dL or an estimated glomerular filtration rate less than 40 mL/min; anemia is defined by a hemoglobin level less than 10 g/dL or less than 2 g/dL the normal reference values; bone lesions include lytic lesions, pathologic fractures, or severely osteopenic bone disease. Hyperviscosity, recurrent infections related to hypogammaglobulinemia, and amyloidosis also represent evidence of end-organ damage.
b PC leukemia is further classified as primary, when occurring de novo, or secondary, when it represents the leukemic phase of MM.
Diagnosis and follow-up of patients with monclonal gammopathy of undetermined significance (MGUS)
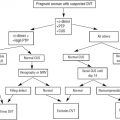
In most instances, MGUS is an incidental diagnosis on blood work performed to investigate a variety of signs and symptoms. The diagnosis is usually made by general practitioners in the ambulatory setting while evaluating complaints that are rather nonspecific, such as fatigue, lack of stamina, or forgetfulness, or symptoms and signs suggestive of MM or amyloidosis, such as back or bone pain, abnormal liver function test results, or neuropathy. The evidence of an M spike on SPEP and/or an abnormal immunofixation (IF) is suggestive of PC dyscrasia, although these findings can occur with other diseases. In the absence of clinical or diagnostic findings suggestive of MM, WM, amyloidosis, or other myeloid or lymphoid neoplasia, an M spike smaller than 3 g/dL on SPEP is pathognomonic of MGUS. The CRAB criteria need to be excluded or, when present, explained by another condition (ie, hypercalcemia secondary to primary hyperparathyroidism, renal failure secondary to diabetic or hypertensive nephropathy, iron deficiency anemia in chronic gastrointestinal [GI] losses). Given its prognostic value, free light chain (FLC) assay is recommended in patients newly diagnosed with MGUS. Bone survey and/or bone marrow aspiration and biopsy are not a mandatory part of the workup of patients with MGUS in the absence of clinical presentations suspicious for active MM or amyloidosis (excruciating or new unremitting bone pain, neurologic symptoms, heart failure) or abnormal laboratory findings. Fat aspiration to exclude amyloidosis should only be performed when clinically indicated (ie, evidence of unexplained liver, heart, peripheral nerve, or GI tract abnormalities).
Although the risk of progression to MM or a related malignancy (WM, amyloidosis) in patients with MGUS is small, it is unremitting and lifelong. In the most updated consensus, the International Myeloma Working Group recommends a repeated SPEP for patients with newly diagnosed MGUS at 6-month follow-up. If the M spike proves stable, complete blood cell counts, kidney function tests, determination of serum calcium levels, and SPEP should be performed yearly in patients with high-risk features (see next section) in an attempt to promptly identify transformation to MM and avoid complications. If clinical conditions are stable, patients with low-risk MGUS could tentatively be assessed with laboratory studies every 2 to 3 years. Patients should be informed to pay special attention to new-onset bone pain, progressive fatigue, or progressive confusion and promptly seek medical attention if such conditions arise. If there is suspicion of interim progression to symptomatic MM, a detailed history taking and complete physical examination should be performed and diagnostic studies, as deemed appropriate, should be recommended to exclude evolution to active disease.
Diagnosis and follow-up of patients with monclonal gammopathy of undetermined significance (MGUS)
In most instances, MGUS is an incidental diagnosis on blood work performed to investigate a variety of signs and symptoms. The diagnosis is usually made by general practitioners in the ambulatory setting while evaluating complaints that are rather nonspecific, such as fatigue, lack of stamina, or forgetfulness, or symptoms and signs suggestive of MM or amyloidosis, such as back or bone pain, abnormal liver function test results, or neuropathy. The evidence of an M spike on SPEP and/or an abnormal immunofixation (IF) is suggestive of PC dyscrasia, although these findings can occur with other diseases. In the absence of clinical or diagnostic findings suggestive of MM, WM, amyloidosis, or other myeloid or lymphoid neoplasia, an M spike smaller than 3 g/dL on SPEP is pathognomonic of MGUS. The CRAB criteria need to be excluded or, when present, explained by another condition (ie, hypercalcemia secondary to primary hyperparathyroidism, renal failure secondary to diabetic or hypertensive nephropathy, iron deficiency anemia in chronic gastrointestinal [GI] losses). Given its prognostic value, free light chain (FLC) assay is recommended in patients newly diagnosed with MGUS. Bone survey and/or bone marrow aspiration and biopsy are not a mandatory part of the workup of patients with MGUS in the absence of clinical presentations suspicious for active MM or amyloidosis (excruciating or new unremitting bone pain, neurologic symptoms, heart failure) or abnormal laboratory findings. Fat aspiration to exclude amyloidosis should only be performed when clinically indicated (ie, evidence of unexplained liver, heart, peripheral nerve, or GI tract abnormalities).
Although the risk of progression to MM or a related malignancy (WM, amyloidosis) in patients with MGUS is small, it is unremitting and lifelong. In the most updated consensus, the International Myeloma Working Group recommends a repeated SPEP for patients with newly diagnosed MGUS at 6-month follow-up. If the M spike proves stable, complete blood cell counts, kidney function tests, determination of serum calcium levels, and SPEP should be performed yearly in patients with high-risk features (see next section) in an attempt to promptly identify transformation to MM and avoid complications. If clinical conditions are stable, patients with low-risk MGUS could tentatively be assessed with laboratory studies every 2 to 3 years. Patients should be informed to pay special attention to new-onset bone pain, progressive fatigue, or progressive confusion and promptly seek medical attention if such conditions arise. If there is suspicion of interim progression to symptomatic MM, a detailed history taking and complete physical examination should be performed and diagnostic studies, as deemed appropriate, should be recommended to exclude evolution to active disease.
Risk factors for progression and stratification models for patients with monclonal gammopathy of undetermined significance (MGUS)
Retrospective epidemiologic studies showed non-IgG immunoglobulin subtypes (IgA, IgD, or IgM), monoclonal component levels of 1.5 g/dL or more, and an abnormal FLC ratio (κ:λ ratio <0.26 or >1.65) to be risk factors for the progression of MGUS to MM.
The Mayo Clinic group has proposed a risk model on the basis of these parameters; patients presenting with all 3 risk factors had a 58% risk of MGUS progression to MM over a period of 20 years. This likelihood was reduced to 37%, 21%, and 5% in patients with MGUS presenting with 2, 1, or no risk factors, respectively.
The Spanish group has proposed a second risk progression model based on the preponderance of aberrant monoclonal PCs in the bone marrow aspirate, evaluated by multiparametric flow cytometry. A percentage of aberrant PCs equal to or exceeding 95% of the total bone marrow PC population and the presence of DNA aneuploidy were established as risk factors for progression to symptomatic MM. Patients with MGUS presenting with both risk factors carried a 46% risk of progression at 5 years versus 10% when only 1 risk factor was present and 2% when both risk factors were absent.
Two recent prospective studies performed by Weiss and colleagues and Landgren and colleagues provided useful information on the natural history of MGUS and outlined the challenges related to predicting progression to MM in the clinical setting. Both studies showed that MM is (almost) inevitably preceded by MGUS. In the study by Landgren and colleagues, only half of the patients whose MGUS progressed to MM presented with a yearly progressive rise in the M spike, whereas the other half had a relatively stable M spike until MM diagnosis, making a rising M spike only a partially reliable marker of disease transformation.
Epidemiology and diagnostic criteria for smoldering multiple myeloma (SMM), multiple myeloma (MM), and plasma cell (PC) dyscrasia variants
MM is further classified as smoldering MM (SMM) and active MM (referred simply as MM from now on). The former is a precancerous condition diagnosed by the presence of an M spike of 3 g/dL or higher and/or a bone marrow invasion by malignant PCs of 10% or more in the absence of end-organ damage (CRAB, see Table 1 ). Unlike MGUS, patients with SMM have a risk of progression to active MM or related PC dyscrasia of 10% per year in the first 5 years, 3% per year in the following 5 years, and 1% per year thereafter, with a cumulative probability of progression of more than 70% at 15 years. Bone marrow involvement by MM cells of 10% or more, M spike equal to or greater than 3 g/dL, and an abnormal FLC ratio (κ:λ ≤0.125 or ≥8) have been identified as risk factors for progression to active disease. Current guidelines recommend close observation and monitoring with no active treatment of patients with SMM. Yet, the paradigm of PC dyscrasia is evolving, with the timing of active therapy for patients with high-risk SMM being recently questioned and early treatment being advocated, in an attempt to slow disease progression and possibly prolong survival.
Three criteria need to be satisfied to diagnose MM: (1) bone marrow invasion by monoclonal PCs or evidence of a plasmacytoma, (2) presence of an M spike on SPEP or urine protein electrophoresis (UPEP) or an abnormal FLC ratio, and (3) evidence of end-organ damage related to the PC clone (any of the CRAB criteria or hyperviscosity, amyloidosis, or recurrent infections) (see Table 1 ). True nonsecretory MM, which represents around 3% of all MM, is an exception to these criteria because an M spike is not identifiable on either SPEP or UPEP with IF. True solitary plasmacytoma is a variant within PC dyscrasia and occurs in around 3% to 5% of cases. It is characterized by a single area of monoclonal PC proliferation either within the bone (osseous plasmacytoma) or in the soft tissues (extraosseous plasmacytoma), tipically of the upper respiratory or GI tract, in the absence of systemic disease and bone marrow involvement. These patients can occasionally present with a small monoclonal component, but generally an M spike cannot be identified on SPEP or UPEP. By definition, in solitary plasmacytoma, CRAB features must not be diagnosed, with the exception of the single plasmacytoma-related lytic lesion for osseous plasmacytoma (see Table 1 ). PC leukemia is defined by the presence of peripheral blood–circulating PCs exceeding 2 × 10 9 per liter or 20% of leukocytes and can be either primary (occurring de novo) or secondary (the leukemic transformation of a preexisting MM) (see Table 1 ). Around 60% of PC leukemia cases are primary.
In the Western world, MM accounts for more than 10% of hematologic malignancies and 2% of annual cancer-related deaths. According to the American Cancer Society, almost 22,000 new cases of MM and 10,700 MM-related deaths are expected for 2012. Although the past decade has witnessed a remarkable improvement in prognosis, mostly related to the introduction of novel chemotherapy agents such as thalidomide, lenalidomide, and bortezomib, MM remains incurable and the current 5-year relative survival rate is estimated to be around 40%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree