DISORDERS OF THYROID-STIMULATING HORMONE CONTROL
DISORDERS CAUSING HYPOTHYROIDISM
CENTRAL HYPOTHYROIDISM
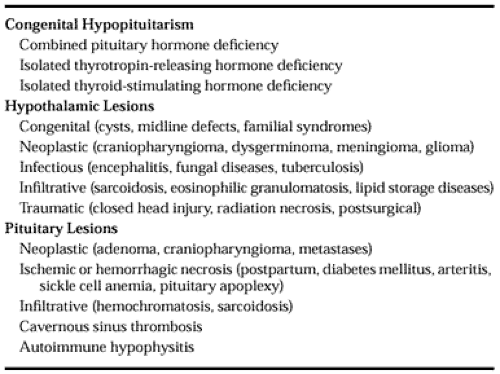
Central hypothyroidism results from failure of the pituitary to secrete biologically active TSH. Central hypothyroidism should be considered in patients who have clinical features of hypothyroidism or hypothalamic-pituitary dysfunction, low serum T4 concentrations, and serum TSH levels that are not elevated. In patients with no clinical manifestations of myxedema and no other evidence of hypopituitarism, other causes of low serum T4 without elevated serum TSH also should be considered, such as decreased thyroid hormone–binding proteins or severe illness. Patients with central hypothyroidism constitute several groups (Table 15-4), as described below.
Combined Pituitary Hormone Deficiency (Idiopathic Hypopituitarism).
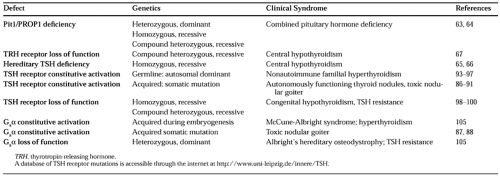
Patients with combined pituitary hormone deficiency (CPHD) have no antecedent histories of disease or injury that could cause hypopituitarism. Clinical features vary. Cases may be sporadic or familial in occurrence. Hypothyroidism alone is rare; patients generally present in childhood with growth hormone deficiency. Patients then go on to develop varying degrees of TSH, prolactin, and gonadotropin deficiencies. However, the patients do not have diabetes insipidus or neurologic deficits. In some families with CPHD, mutations in pituitary-specific transcriptional factors (Pit-1, Prop-1) have been identified (Table 15-5).62,63 and 64
Isolated Thyroid-Stimulating Hormone Deficiency.
In patients with isolated thyroid-stimulating hormone deficiency, basal serum TSH values may be low, normal, or slightly elevated; TRH stimulation generally causes a rise in serum TSH levels. The chronic administration of TRH can restore thyroid
hormones to normal levels. Hence, the hypothyroidism is thought to result from impaired release of TRH from the hypothalamus. Rarely, familial cases with mutations in the β-TSH gene (see Table 15-5) have been described. Mutations have included a truncated β-TSH transcript as a result of a premature stop codon; a single amino-acid substitution resulted in a β-TSH that was unable to heterodimerize, and a frame-shift mutation resulted in reduced amounts of TSH with decreased bioactivity.65,66 In another patient, loss-of-function mutations of the TRH receptor were reported (see Table 15-5).67
hormones to normal levels. Hence, the hypothyroidism is thought to result from impaired release of TRH from the hypothalamus. Rarely, familial cases with mutations in the β-TSH gene (see Table 15-5) have been described. Mutations have included a truncated β-TSH transcript as a result of a premature stop codon; a single amino-acid substitution resulted in a β-TSH that was unable to heterodimerize, and a frame-shift mutation resulted in reduced amounts of TSH with decreased bioactivity.65,66 In another patient, loss-of-function mutations of the TRH receptor were reported (see Table 15-5).67
Hypothalamic Lesions.
Destructive lesions of the hypothalamus may result in central hypothyroidism. Generally, multiple pituitary hormones are involved, and patients often have diabetes insipidus. Serum prolactin levels may be mildly elevated because of interruption of the tonic dopaminergic lactotrope inhibitory pathway. In addition to hormone deficiencies, patients may have neurologic abnormalities and other manifestations of hypothalamic disease, such as disturbances of autonomic function, temperature regulation, food and water intake, and sleep cycle, as well as emotional lability.
TSH with reduced bioactivity has been found in the serum of patients with hypothalamic hypothyroidism; long-term treatment with TRH increases the bioactivity of their TSH.68 These findings might explain why some patients with hypothalamic disorders have hypothyroidism despite showing normal or slightly increased levels of immunoreactive TSH.
Pituitary Lesions.
Pituitary lesions also cause hypothyroidism. Hypothalamic disturbances, visual field cuts, and parasellar abnormalities may be observed if an extrasellar extension of the lesion is present. Pituitary adenomas rarely cause hypothyroidism if they have not grown large enough to cause distortion and enlargement of the margins of the sella turcica.69
THYROID-STIMULATING HORMONE AND THYROTROPIN-RELEASING HORMONE TESTING IN HYPOTHALAMIC-PITUITARY DISEASE
Basal TSH levels may be normal, low, or slightly elevated in patients with central hypothyroidism. Basal TSH values do not correlate with free T4 levels, and TRH-stimulated TSH values are not proportional to basal TSH values.55 Therefore, clinical evaluation and measurement of free T4 should be used in confirming the diagnosis of suspected central hypothyroidism and in titrating thyroid hormone replacement therapy in patients with central hypothyroidism.
Initially, the proposal was made that TRH testing should differentiate pituitary from hypothalamic causes of central hypothyroidism, with pituitary dysfunction causing a blunted or absent TSH response and hypothalamic disease resulting in a normal or exaggerated TSH rise that is delayed or prolonged. Although such classic patterns are found in many patients, the responses often overlap. Normal or “hypothalamic” patterns have been observed in patients with pituitary lesions, and the serum TSH response has been flat in some patients with suprasellar disease.70 Thus, the anatomic site of the central lesion may not always correlate with the expected functional consequences on TRH responsiveness. Abnormal serum TSH responses to TRH (i.e., blunted or delayed peaks) also are noted frequently in patients with pituitary or hypothalamic diseases even when the patients appear clinically euthyroid and their serum thyroid hormone levels are normal.71
DISORDERS CAUSING HYPERTHYROIDISM
THYROID-STIMULATING HORMONE–INDUCED HYPERTHYROIDISM
Hyperthyroidism induced by TSH has been described in a small group of thyrotoxic patients in whom serum TSH levels are normal or increased (see Chap. 42). If signs and symptoms of thyrotoxicosis are absent in a patient with elevated thyroid
hormone concentrations and normal serum TSH levels, other causes of hyperthyroxinemia with nonsuppressed TSH also should be considered (Table 15-6). Patients with TSH-induced hyperthyroidism have clinical evidence of a stimulated thyroid gland, including diffuse goiter and elevated radioactive iodine uptake. Extrathyroidal manifestations of Graves disease are lacking, and the assay of TSI is negative.72 Two groups of abnormalities have been described.
hormone concentrations and normal serum TSH levels, other causes of hyperthyroxinemia with nonsuppressed TSH also should be considered (Table 15-6). Patients with TSH-induced hyperthyroidism have clinical evidence of a stimulated thyroid gland, including diffuse goiter and elevated radioactive iodine uptake. Extrathyroidal manifestations of Graves disease are lacking, and the assay of TSI is negative.72 Two groups of abnormalities have been described.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree