DIAGNOSIS OF OSTEOPOROSIS USING BONE DENSITOMETRY: THE WORLD HEALTH ORGANIZATION CRITERIA
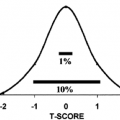
To allow bone densitometry to be used for the identification of asymptomatic individuals at risk for fracture, a paradigm shift in the definition of osteoporosis had to occur. The accepted definition of osteoporosis is “a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture risk”7 (see Chap. 64). Although this accepted definition includes the terms low BMD, systemic disease, microarchitectural deterioration, and increased bone fragility, only BMD can presently be objectively measured in clinical practice. Before this consensus statement defined osteoporosis, a diagnosis was made on the basis of the presence of a fragility fracture, which usually occurs only in the advanced osteoporotic state. Recently, osteoporosis has been defined on the basis of a reduced level of BMD. This new definition was implemented by the World Health Organization (WHO) Consensus Development Conference on Osteoporosis.2 The goal of the WHO Working Group was to establish a relationship between bone mineral content (BMC) per centimeter measured, at that time, predominantly at the radius and hip, and the prevalence of fractures in elderly postmenopausal white women. It was determined that those women in the lowest quintile of BMD had the greatest prevalence of global fractures. The lowest BMD quintile, when corrected for different instrument calibrations, corresponded to 2.5 standard deviations (SD) below the mean of the reference population. Therefore, the new definition of osteoporosis became a bone mass that is at least 2.5 SD below the mean of a young normal reference population. One major clinical justification for changing the diagnostic criteria for osteoporosis from one of prevalent fragility fractures to one of low BMD are data that established a higher risk for a second fracture once a first fracture has occurred.8 In addition, the combination of low bone mass and a vertebral fracture increased the risk of a hip fracture. This risk is far greater than the risk of a first fracture in elderly individuals who have low bone mass alone.8 The logical corollary of these data is the need to identify individuals with low bone mass before the first fracture.
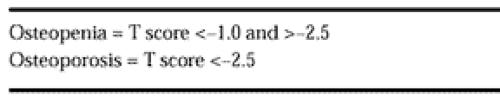
The WHO criteria for the diagnosis of osteopenia and osteoporosis (Table 57-1) are based on a patient’s comparison to peak adult bone mass (PABM) and use standardized scores (T score). The WHO Working Group chose to categorize individuals using the number of SD a patient’s bone mass is below the mean bone mass of a young normal reference population. Because fracture risk is a gradient, increasing with declining levels of bone mass,9 the WHO created a second diagnostic category of osteopenia (low bone mass, T score >-2.5 but <-1.0 SD) to alert the clinician that individuals with smaller reductions in bone mass merit attention, particularly if they are postmenopausal or have secondary conditions associated with bone loss. Data suggest that postmenopausal women who are not receiving hormone-replacement therapy (HRT) will predictably lose bone.10,11 As the emphasis on skeletal health shifts from treatment to prevention, the diagnostic category of osteopenia may become increasingly important. Postmenopausal women not receiving therapy to prevent bone loss may unknowingly continue to lose bone, thereby progressively increasing their fracture risk as they age. Hence, postmenopausal women identified as osteopenic may be targeted for prevention strategies to preserve their skeletal mass. Individuals with osteopenia may also experience fragility fractures, particularly when risk factors for fracture are present.12 Such factors include increased rates of bone turnover, advancing age, increased likelihood of falling, etc. It, therefore, is not surprising that some patients with small
reductions in BMD and the presence of other risk factors may have fragility fractures. For this reason, the National Osteoporosis Foundation (NOF) clinical guidelines recommend treating all postmenopausal women with T scores <-2.0 SD without risk factors and <-1.5 SD with one or more risk factors.13
reductions in BMD and the presence of other risk factors may have fragility fractures. For this reason, the National Osteoporosis Foundation (NOF) clinical guidelines recommend treating all postmenopausal women with T scores <-2.0 SD without risk factors and <-1.5 SD with one or more risk factors.13
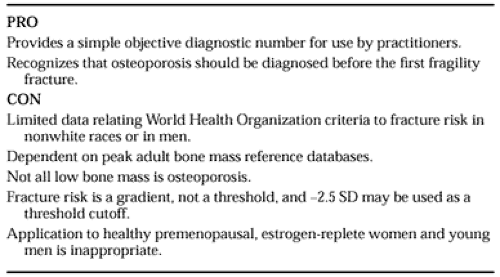
Like all diagnostic criteria, there are strengths and limitations to the WHO criteria for the diagnosis of osteoporosis. These are listed in Table 57-2. The WHO criteria provide a practitioner with objective values to be used for the diagnosis of low bone mass, akin to blood pressure for the diagnosis of hypertension. Practitioners have objective criteria that initiate the cognitive process of assessment of low bone mass, leading to intervention. In addition, the WHO criteria stress the importance of making a diagnosis of low bone mass (osteopenia) or osteoporosis before the first fracture occurs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree