Fig. 18.1
Map of New York State displays the distribution of patients that we serve
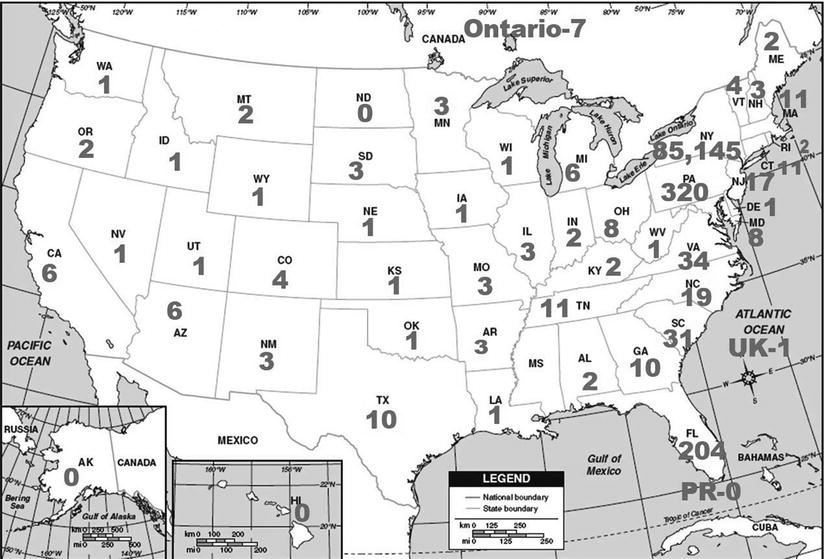
Fig. 18.2
Map of the United States and Canada showing the distribution of patients that travel to our facility
Our practice has expanded over the years and currently includes a main office which is approximately 33,500 square feet (Fig. 18.3) and three satellite offices: 1,200 square feet (a rural location southeast of the main office), 2,000 square feet (northwest of the main office), and 2,300 square feet (east of the main office). Combined, we serve approximately 420 patients daily: 340 screening, 60 diagnostic, 20 screening ultrasound, eight magnetic resonance imaging (MRI) examinations, and six genetic appointments.


Fig. 18.3
Elizabeth Wende Breast Care, LLC, located in Rochester, New York
The first floor of the main office is designated for patient care, and the second floor is designated for medical record storage, administrative offices, and the genetics department. The main office, on a bus line and with ample free parking, sees an average of 265 screening appointments and an average of 60 diagnostic appointments daily. The office includes six radiologists, four full-time and two part-time, in addition to a staff of 134 employees, 97 full-time and 37 part-time. The majority of our work is done online (patients have the option to wait for results) from 6:45 a.m. to 5:00 p.m., which can make for a long day for staff and radiologists.
Screening services available include digital mammography, digital breast tomosynthesis, ultrasound, and breast MRI. All examinations are interpreted at the main office, as the satellite office studies are transferred via our extended network circuits to the main office. Each screening mammography examination is read with the use of computer-aided detection (CAD), and same-day results are offered to those patients who choose to wait. For those who do wait for results (approximately 62 % of our population), additional views, ultrasound, and needle biopsy can all be performed during the same visit, if necessary. Whether our patients travel a distance for their appointment, make special transportation arrangements, or are anxious for their results, the option to have the mammogram and additional work-up, if necessary, during the same visit is very important. For those fitting the appointment into a busy life schedule, the option to not wait for results is appreciated.
In addition to the screening services mentioned previously, we also offer diagnostic services which include diagnostic ultrasound, breast MRI, ductography, fine-needle aspiration cytology (FNAC), and needle core biopsy for all imaging modalities (stereotactic, ultrasound, and MRI).
Breast MRI was a modality that was added to our practice in 2003. We began with MRI 1 day per week with a mobile lease and eventually, due to the high patient demand, built an addition to house a permanent unit to be utilized daily. Having access to an extensive range of diagnostic services has allowed our facility to provide care to a wide array of patients, whether recently diagnosed with breast cancer or those considered at high lifetime breast cancer risk.
As of 2010, we implemented a risk assessment/genetics program and have had a certified genetic counselor on staff since 2011. The process began when we realized patients with multiple risk factors for breast or ovarian cancer had many questions and needed counseling at a level that our current staff could not provide. This program has allowed us to reach out to our high-risk population and ultimately provide additional and potentially lifesaving services, such as screening MRI.
Design of a Dedicated Breast Center
When opening a breast imaging center, there are several factors that need to be considered. From the beginning, it is important to know and understand the state and local laws that may apply in your area.
When picking a location, it is important to keep in mind the population of patients you hope to reach. A city location will allow access to patients in many surrounding areas, as the city is often a central location. A rural location will help to reach those patients who may not have access to urban areas. Another aspect to consider is where the imaging center will be located in relation to a bus line. Allowing access for patients without their own mode of transportation is important.
It is optimal that from the very beginning stages, you plan out what services will be offered to patients, but even with the best plans in place, a practice may grow and require additional space to include services not initially anticipated.
When designing the layout of the breast center, it will be helpful to include an architect in the discussion on the services that will be offered and the desired flow of the practice. This will help to design an efficient layout for a seamless daily workflow. Parking availability should also be considered and directly related to the capacity of the building, for staff and patients alike. Additionally, protecting patient privacy and ensuring that practices are conducted in accordance with Health Insurance Privacy and Accountability Act (HIPAA) will need to be considered when designing the center. This needs to be considered from the time the patient checks in and continued throughout the office visit. Most of the health and human services (hhs.gov) [3] sites are an excellent resource to assure proper protection for patient privacy.
The following subsections will discuss the layout of our facility, from patient check-in and visitor waiting room to the mammography and radiologists’ suites.
Patient Check-In and Visitor Waiting Room
When a patient first enters the facility, she approaches the front desk staff in the main waiting room. The outside waiting room should include varying-sized chairs or benches to accommodate patients and visitors of all sizes. Armchairs are important for patients with limited mobility who may need assistance when getting to a standing position, while bench-style seating (armless) is important as it provides comfort for the overweight patient who may require slightly more room than the standard chair. A waiting room bathroom should be incorporated, as family members tend to accompany and wait for the patient’s visit to be complete. Building codes and specifications will need to be adhered to, to ensure requirements for handicap accessibility are met, for example, a large doorway for wheelchairs, scooters, walkers, or those requiring extra assistance.
Our front reception area went through remodeling to be designed in accordance with HIPAA. It is essential that the check-in process is as private as possible to protect the patients’ protected health information (PHI). Figures 18.4 and 18.5 show the transition of the reception area as the facility adapted to HIPAA regulations. Each receptionist has her own computer and desk, separated from the next receptionist by a glass partition. The partition provides the privacy needed for review of PHI that takes place at check-in (Fig. 18.6).




Fig. 18.4
The original reception area was an open design which did not allow for much privacy while a patient checked in with reception staff

Fig. 18.5
Remodeling of the reception area was performed to ensure adequate privacy for the patient while checking in at the front desk

Fig. 18.6
Glass partitions divide the reception desk to protect the patients’ health information
Aside from the physical design of the outside waiting area, we offer a wide selection of reading materials, as well as herbal teas and decaffeinated coffee, television, and wireless internet for both patients and those who may be accompanying them for the appointment.
Patient Waiting Room Design
Due to the volume of patients we service and the fact that some patients may experience a lengthy visit, the office was designed with two inside patient waiting areas. The asymptomatic screening patients, whether waiting for results or not, have a shorter appointment time, approximately 1 h from check-in to checkout. However, the symptomatic diagnostic patient may be with us for several hours for a complete work-up. The decision of designing two separate waiting areas came from past experience; when all patients shared one waiting area, regardless of appointment type, we found that patients were noticing others would arrive after them and leave before them, and this added additional anxiety to an already stressful appointment. At the earliest opportunity (when further space became available), the decision was made to separate the diagnostic patients and the screening patients. Incorporating the two waiting rooms has turned out to be an excellent decision, as the dynamics of each scenario fit the respective waiting room.
The screening changing area contains 10 changing booths and 72 lockers; the screening waiting room allows seating for 51. A smaller waiting room is adjacent to the large screening waiting room; this room is utilized if a patient requires a smaller setting. The diagnostic changing area has five changing booths and 36 lockers; the diagnostic waiting room is smaller allowing for seating for 34. Both waiting rooms have a fireplace and fish tank to promote a tranquil environment. Decaffeinated coffee and herbal teas are offered for patients, along with reading material (Figs. 18.7 and 18.8).



Fig. 18.7
The waiting room for patients attending screening mammography contains aquariums and a fireplace as it was designed to be a tranquil and serene environment

Fig. 18.8
The waiting room for patients presenting for a diagnostic appointment is a smaller version of the screening waiting room, also housing a fireplace as well as a flat-screen television
As with the visitor waiting room, it is important to have comfortable chairs for patients of all sizes. It has been reported that patients with weight issues often do not adhere to screening tests, but if the environment is accommodating, these patients may be more inclined to keep their appointments [4]. Research has shown that obese women have higher mortality rates for breast and cervical cancer [5], and one bad experience may turn a patient away from a lifesaving screening exam.
Mammography Suites
The main office has ten mammography suites that are centrally located from the two patient waiting rooms. Each room is equipped with a direct ray full field digital mammography (FFDM) unit with attachments and all supplies necessary for the study (Fig. 18.9).


Fig. 18.9
A typical mammography room at our facility
The largest mammography suite has been designated for localization procedures and is also equipped with an examination table used for ductography cannulation (Fig. 18.10).


Fig. 18.10
The largest mammography room is utilized for procedures such as ductography and contains a bed to aid with the procedure so that the patient does not need to be transferred to another room for imaging
Utilizing this larger room for interventional procedures is a benefit, as added staff may be needed during the procedure, such as a nurse, in cases where the patient needs extra assistance. Additionally, in each room, a thin client computer is provided for access to the radiology information system (RIS) and picture archiving and communication system (PACS) (Fig. 18.11). The technologist has the ability to review prior reports and images as well as update electronic health information that may be provided during the patient interview portion of the examination.
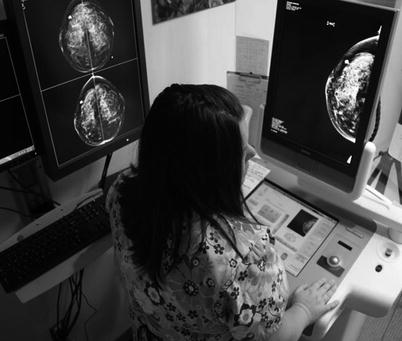
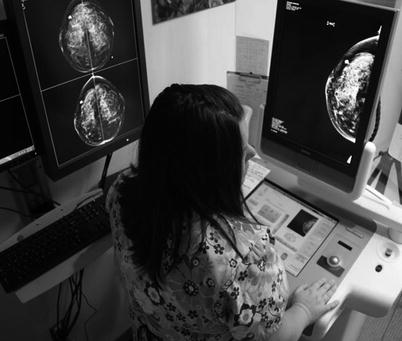
Fig. 18.11
The technologists have access to prior imaging while preparing for the patient in the mammography suite
Radiologist Suite
Each radiologist at our facility has a two-room suite consisting of a reading room and an attached examination and ultrasound room (Fig. 18.12). There is hallway access to both rooms, as well as an inside doorway connecting the two rooms. This allows the patient to be escorted in from the outer hallway and allows the radiologist to enter the examination room from their reading room (Fig. 18.13). Daily, each radiologist has a medical assistant scheduled with them to assist with patient flow.



Fig. 18.12
The radiologists’ reading room and examination room can both be accessed from the hallway, as well as by a doorway between the two rooms

Fig. 18.13
A view into the examination room from the reading room demonstrates the convenience for the radiologist when preparing to examine a patient
The radiologist reading room reflects the current modern, ergonomic design for the digital era. Due to the sedentary nature of the digital reading room, it is crucial that ergonomics be addressed to minimize eyestrain, lower back strain, carpel tunnel syndrome, and fatigue [6]. Each radiologist’s office is equipped with a lumbar-supportive chair and a height adjustable desk that can be used for seated or standing reading (Figs. 18.14 and 18.15).

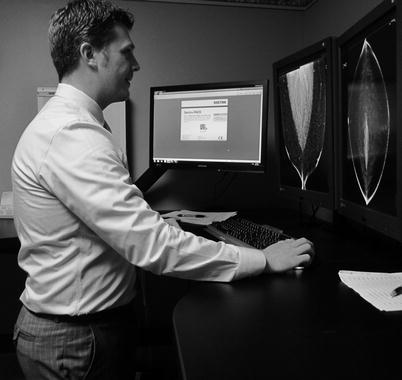

Fig. 18.14
With the new ergonomically designed workstations, the radiologists can read while remaining seated in a lumbar-supportive chair
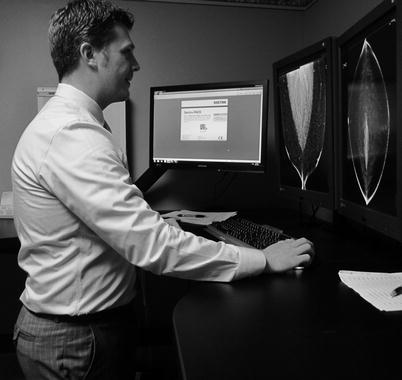
Fig. 18.15
The ergonomically designed workstations can also be adjusted to allow the radiologist to stand while interpreting examinations
Two 5 megapixel monitors can be height adjusted and tilted for optimal viewing to minimize neck strain. Each room has overhead fluorescent lighting, but when interpreting digital mammograms, it is not used due to the reflective glare on the monitors. Instead, ambient lighting (with a low-wattage bulb) that is located behind the monitors is used. Each radiologist has an ergonomic keyboard and mouse allowing for their hand and wrist to be neutrally positioned. A programmable gaming mouse is used and programmed so that with slight hand movement, the reading protocol can be advanced and CAD can be applied.
The ultrasound room attached to the reading room allows for an efficient workflow for the radiologist. This room is used for clinical breast examination, handheld ultrasound, and clinically guided procedures such as cyst aspirations, antegrade ductography injection, FNAC, and core biopsy. In addition to this attached room, there is an overflow ultrasound/examination room that is shared amongst the radiologists if needed on a busy day. This allows the radiologist to see their next patient without waiting for the turnover and cleaning of the room just used. The combination of having an individual suite and a medical assistant assigned to help maintain adequate patient flow is an important aspect in the design of our facility.
Running the Office
This section will review how our systems are integrated to provide a seamless daily clinical workflow.
RIS and PACS
In 2008, our facility became 100 % digital and since then has been converting to a paperless, chartless environment. Our facility uses an electronic proprietary RIS (Avairis). This system is closely integrated with our PACS system (Sectra). The two systems, using bidirectional Health Level 7 (HL7) messaging, have allowed us to follow and manage all aspects of our patients’ visits electronically, as well as maintain an electronic chart for each patient.
Our operation has gone through many changes over the years, and it is important to describe the progression that has brought us to the present functionality. Originally, during the time of film-screen mammography, PACS was solely used to view the new digital images as we began to implement FFDM. As the years progressed, our Information Technology (IT) department and PACS administrators have integrated PACS closely with the RIS. Prior patient information has been added into the patients’ record on PACS to ensure that all information on a patient is directly available to the radiologist. In the transition from film screen to digital, film images have been digitized into PACS. Additionally, all radiology reports have been tied into the exams in PACS and can be viewed directly alongside the images. Personal and family history and prior needle or surgical biopsy information are also now included in PACS and can easily be viewed by the radiologist while reviewing a case. Changes such as these have allowed the radiologists to read all examinations from their own workstations within their own offices.
Today, when a patient schedules an appointment, a message (made possible with HL7) containing appointment information is sent to PACS. PACS performs an automatic “pre-fetch” of prior images from archive the night before the appointment. All prior images will be available for the radiologist to review and compare with the current examination.
During the appointment, PACS will send an HL7 message to the RIS when the radiologist has completed reading the examination. Immediately after screening examinations are interpreted and marked by the radiologists as normal, a message is sent to the RIS, the patient result letter is automatically printed, and the date of the next appointment is set for the patient. Once the letter is printed, the medical assistant knows that the patient’s visit is complete and can then give the patient her results. At the same time, the report is also automatically sent to the patient’s referring physicians, and the name of the reading radiologist is sent to the billing program in the RIS and charges are posted.
When a radiologist needs additional imaging, they will mark either “finding” or “assessment” on the exam in PACS. If “assessment” is marked, this is a request for extra mammographic images to be performed. A message is automatically sent to the RIS where an extra view/exam is created on the “dashboard” (which will be explained in the next section) and is available for the technologist. The process will repeat itself until the patient is marked as normal. If “finding” is marked, which means the additional mammographic views are obtained and the radiologist is still concerned about the area of investigation, a message is automatically sent to the RIS to create a new exam for an ultrasound, and the patient will present on the ultrasound “dashboard” for the sonographers or the radiologist, converting the exam to a diagnostic appointment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree