Cytopathology is a specialized branch of pathology related to the study of cells derived from either fine-needle aspiration biopsy (FNAB) or exfoliation including effusions, washings, brushings, or body fluids. FNAB is performed using a 23- or 25-gauge hypodermic needle attached to a 10-mL plastic syringe. FNAB can be performed blindly for palpable masses or under radiologic guidance including ultrasound (US), computed tomography (CT), or magnetic resonance imaging (MRI) for nonpalpable lesions. Specimens obtained from any of these sources can be prepared in several ways for conventional cytopathologic evaluation and ancillary studies. Smears can be made directly or from the cell pellet obtained after centrifugation of the specimen following admixture with a liquid base such as RPMI or Cytolyt solution. Monolayer preparation of the specimen can also be made using different techniques such as Thin Prep and Sure Path. Smears prepared by any of the techniques are usually fixed in alcohol for Papanicalaou staining, or air-dried for Diff-Quik staining. In addition, aspirated material from FNA or exfoliative specimens can be rinsed in RPMI or Cytolyt solution to prepare tissue blocks that are fixed in formalin, processed routinely similar to surgical tissues, embedded in paraffin, and subsequently cut at 5 μm and finally stained by the hematoxylin and eosin (H&E) method.
The popularity of core needle biopsy (CNB) has to a large extent reduced the performance of FNAB in many centers. CNB produces cores of breast tissue that are generated by introduction of automated spring-loaded devices that activate a 14- to 18-gauge cutting needle into the localized site. Unlike FNAB, CNB not only provides tissue architecture that facilitates interpretation but also adequate tissue for performing ancillary studies. In contrast to CNB, FNAB is however better tolerated, less invasive, and allows more effective sampling of small-sized lesions. Moreover, the possibility of sampling multiple sites in a large-sized lesion is an added advantage. FNAB is also the preferred technique for investigating breast lesions close to the chest wall because of fear of causing pneumothorax with a CNB or for investigating lesions occurring in breast with any type of tissue expander because of the risk of puncturing the latter. FNAB, however, may yield very minimal material insufficient for diagnosis particularly in sclerotic lesions necessitating the performance of CNB. For primary breast masses, the inability of FNAB to distinguish in situ from invasive carcinomas is a major disadvantage, which has essentially led CNB to replace FNAB for initial investigation of index breast lesions that are deemed to be very suspicious for malignancy on clinical examination and imaging findings. It should be noted, however, that FNAB and CNB are complementary techniques and can be used alone interchangeably or in conjunction based on the requirement of individual cases for preoperative diagnosis. The golden rule for the interpretation of breast FNAB is to always correlate the cytologic findings with clinical and imaging findings, commonly referred to as the triple test. Any discrepancy between the 3 components of the triple test should lead to obtaining a CNB or surgical excision for definite diagnosis of the abnormality. The results of FNAB should be categorized into 1 of 5 categories: benign, atypical/indeterminate, suspicious, malignant, or nondiagnostic/unsatisfactory.1 The overall sensitivity and specificity of FNAB in comparison to CNB and surgical excision is high and ranges from 85% to 100% in different reports.2-8 The role of cytology including FNAB of primary breast masses and metastatic tumors and exfoliative specimens such as nipple aspirate fluid, ductal lavage, and effusions is discussed in the following sections.
Most breast cysts are encountered in premenopausal women. They can be single or multiple, of variable size, and may mimic solid masses on imaging. FNAB of breast cysts yields foamy histiocytes, few benign ductal epithelial cells, and cells with abundant granular cytoplasm referred to as apocrine cells in a background of proteinaceous material.9-10 Cytologic examination of breast cysts may be optional if the cyst yields clear yellow fluid and collapses following aspiration. However, cysts that yield brownish or reddish fluid, do not collapse following aspiration, or are associated with a residual mass should be aspirated again or subjected to further investigation to exclude cancer.
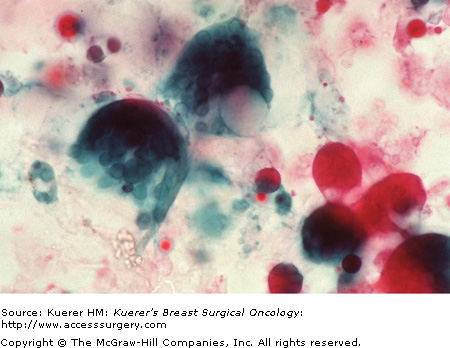
FNAB is useful for confirming lesions highly suspicious for fat necrosis on imaging or for those cases of fat necrosis that may closely mimic malignant lesions clinically and on imaging.11 It is to be noted however that fat necrosis and malignancy can coexist, and therefore proper sampling of the lesion, careful cytologic examination, recognition of the pitfalls, and strict adherence to the triple test can avoid the occurrence of a false-positive or false-negative diagnosis. Fat necrosis yields fragments of degenerated adipose tissue, foamy histiocytes including multinucleated giant cells, conglomeration of red blood cells resulting in structures resembling a bag of grapes referred to as myospherulosis, hemosiderin pigment deposition, and variable degrees of acute and chronic inflammation, granulation tissue, and fibrosis. Figure 24-1 illustrates multinucleated giant cells and myospherules on direct smears of FNAB from a case of fat necrosis of the breast. Reactive atypia may be encountered in the macrophages, myofibroblasts, and epithelial cells, which can lead to an erroneous diagnosis of malignancy.
FNAB can be utilized not only for making a diagnosis but also for obtaining material for microbiologic culture studies from breast abscesses. Breast abscesses are commonly encountered in lactating women. The aspirated material is yellow, purulent, and shows abundant neutrophils, granulation tissue, and cellular debris.12 Epithelial and mesenchymal cells may exhibit reactive atypia, which should not be mistaken for malignancy.
Subareolar abscess is a distinct type of breast abscess that occurs over a wide age range, is not related to lactation, and results from squamous metaplasia of lactiferous ducts resulting in keratin plugging and rupture of the duct.13 The resultant squamous material in the stroma elicits acute inflammation and eventually may lead to fistula formation. FNAB shows abundant squames, acute inflammation. and the characteristic finding of multinucleated giant cells with ingested squames.
Granulomatous mastitis, caused by organisms such as mycobacterium tubercolosis, fungus, actinomyces, cat scratch disease, and foreign bodies such as sutures following surgery or silicon leakage from breast implants, can result in a breast mass that may be suspicious for malignancy on clinical examination and on imaging. FNAB shows clusters of epithelioid macrophages and multinucleated giant cells with or without associated necrosis. Silicone may be dissolved during processing resulting in empty spaces or it may be noted as homogenous refractile droplets on the smears.
Women in the reproductive age group show variable degrees of epithelial proliferation, stromal fibrosis, and cystic change resulting in ill-defined thickening and/or masses that are often investigated by FNAB to exclude malignancy. FNAB in these cases yields few fragments of benign ductal epithelial cells with or without evidence of proliferation, apocrine cells, scattered individual nuclei derived from myoepithelial cells, foamy histiocytes, and stromal fragments of fibrosis. Proliferative changes involving ductal epithelial cells result in moderate- and large-sized fragments comprised of sheets of epithelial cells including both ductal and myoepithelial types. There may be mild pleomorphism of the nucleus, presence of small nucleoli, and mild nuclear enlargement. There is evidence of cellular streaming with nuclear overlap, crowding, and presence of irregular slit-like spaces within the fragments. Presence of punched-out spaces with focal cribriforming and evidence of monotony in the epithelial cells are worrisome features for presence of atypical ductal hyperplasia. Further investigation of lesions demonstrating findings of atypia on FNAB is warranted to exclude the presence of low-grade carcinoma in situ.
Fibroadenoma is a benign fibroepithelial tumor, characterized by the proliferation of benign epithelial and stromal elements. These lesions are noted as a moveable well-defined mass in women in their 20s and 30s, which may be either easily palpable or nonpalpable and detected on imaging alone. Direct smears of classical cases of FNAB of fibroadenoma show clusters and sheets of benign ductal epithelial cells with associated myoepithelial cells that often form antler hornlike clusters, few fibromyxoid fragments of low cellularity, and many individual naked nuclei in the background.14Figure 24-2 illustrates the presence of many individually distributed naked nuclei, associated with a cluster of benign ductal cells obtained from FNAB of a case of fibroadenoma. The majority of the latter are myoepithelial in origin. Fibroadenomas are one of the most common causes of a false-positive diagnosis on FNAB of breast. High cellularity of the epithelial elements, nuclear atypia, presence of dispersed epithelial cells, and myxoid/mucoid background can all lead to misdiagnosis of fibroadenoma as a malignant lesion. Definite diagnosis of fibroadenoma should only be made on FNAB if the lesion exhibits all the three characteristic cytologic features and correlates with imaging findings of a well-defined mass with no irregularity or lobulations of the edges, absence of increased vascular flow, and no history of increased growth. Lesions not fulfilling the criteria or any discordance between cytologic imaging and clinical findings should be investigated further with either a CNB or preferably with surgical excision.
Figure 24-2
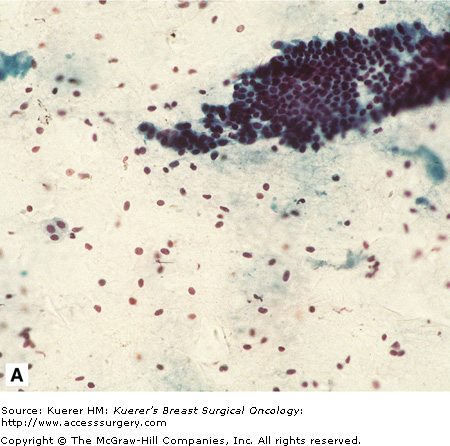
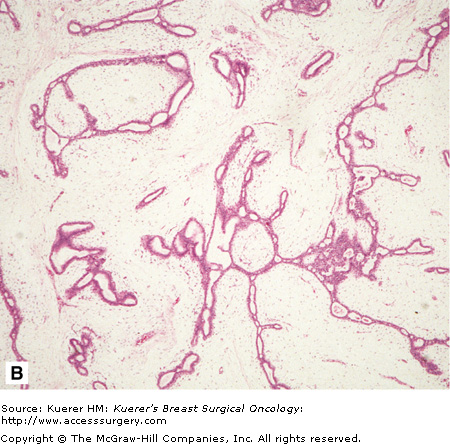
Illustration of a case of fibroadenoma on FNAB (A) and CNB (B). Note the cluster of benign ductal cells with associated myoepithelial cells and presence of many naked nuclei in the background of the smear. The corresponding CNB (B) shows classic features of a fibroadenoma including the proliferation of benign ductal and stromal elements.
Phyllodes tumors are fibroepithelial tumors that by definition are associated with a benign epithelial component and a cellular stromal component that exhibits variable degrees of atypia. At the lower end of the spectrum, the stromal fragments exhibit a mild increase in cellularity without any evidence of atypia or presence of mitotic figures and no evidence of stromal overgrowth or necrosis. Because of overlapping features between low-grade phyllodes tumors and cellular fibroadema, FNAB of these lesions is categorized as indeterminate and surgical excision is recommended for a definite diagnosis.15,16 FNAB, however, can clearly establish the diagnosis of malignant phyllodes tumor. Stromal fragments on FNAB of malignant Phyllodes tumor clearly exhibit not only increased cellularity but also stromal atypia, pleomorphism, and mitotic figures. In addition, atypical stromal cells are also distributed in the background of the smears. There may be necrosis. The epithelial fragments in all cases of Phyllodes tumors is essentially benign with the presence of both epithelial and myoepithelial cells.
Papillary neoplasms by definition exhibit a fibrovascular core with proliferation of epithelial cells around them. Papillary neoplasms can be benign or malignant. When they occur in the lactiferous ducts, they are usually associated with a bloody nipple discharge. Intraductal papillomas are benign tumors that demonstrate proliferation of benign ductal epithelial cells including myoepithelial cells around the fibrovascular cores.17 Three-dimensional papillary clusters of the same cells, foamy and hemosiderin-laden macrophages, and a proteinaceous material in the background are usually noted. In some cases, the fragments may be bordered by tall columnar cells and similar cells may be distributed in the background. Papillary carcinomas, on the other hand, demonstrate atypical epithelial cells around the fibrovascular cores and in the background without the presence of myoepithelial cells.17-19 While the distinction between benign and malignant papillary tumors may be possible in many cases, it is recommended to designate these lesions as papillary neoplasms and categorize them as indeterminate on cytology.
Mucinous carcinoma exhibits abundant extracellular mucin in direct smears. These tumors must be distinguished from mucocele-like lesions on FNAB, which range from benign to atypical in morphology. Unlike mucinous carcinomas, mucocele-like lesions are generally associated with reduced cellularity and show few sheets of benign ductal epithelial cells including myoepithelial cells. On the other hand, mucinous carcinoma demonstrate increased cellularity with 3-dimensional epithelial cell clusters and individually distributed atypical epithelial cells of varying degrees of atypia.19,20 Most importantly, the clusters do not contain myoepithelial cells. Therefore, while a distinction of mucocele-like lesions from mucinous carcinomas is possible on FNAB majority of times, lack of typical features and inability to definitely distinguish these lesions on FNAB with confidence should lead to surgical excision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree