Keywords
chemotherapy, fertility preservation, gonadotoxicity, gonadotropin-releasing hormone (GnRH) agonist, ovarian protection
8.1
Introduction
Cancer is not uncommon and no longer considered as an incurable disease among reproductive-age women. Indeed, cancer is estimated to occur in approximately 2% of women under the age 40. Over the past decades, there has been a remarkable improvement in the survival rates due to the marked progress in detecting cancer at earlier stages and the improvement in treatment modalities. With improvements in treatment outcomes, 83% of women younger than 45 years diagnosed with cancer in the USA survived between 2002 and 2012. As a consequence of the increase in the number of patients surviving cancer, greater attention has been focused on the delayed effects of cancer treatments on the quality of future life of the survivor.
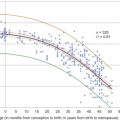
The treatment for most of the cancer types in reproductive-age women involves either removal of the reproductive organs or cytotoxic treatment (chemotherapy and/or radiotherapy) that may partially or definitively affect reproductive function. The irreversible gonadotoxic effects of chemotherapeutic agents on the ovary are well documented, especially for anthracyclines and alkylating agents (e.g., cyclophosphamide, busulfan and ifosfamide), which are the backbone of chemotherapy for breast cancer, lymphomas, leukaemia and sarcomas (see also Chapter 4 ). Pelvic radiation therapy also causes follicular destruction and less than 2 Gy of radiation can deplete at least 50% of the follicles. In addition, exposure to 5–10 Gy of pelvic radiation results in premature ovarian insufficiency (POI) in many women. The risk of ovarian failure following chemotherapy is highly correlated with the woman’s age and ovarian reserve at the time of treatment, type and dosage of drug administered, and the duration of drug exposure. After chemotherapy, the long-term incidence of amenorrhoea is at least 25% at age 30 years and is 50% in women aged 35–40 years, whereas most women over 40 years of age become amenorrhoeic, and their chances of restoring ovarian function is dismal. In addition, temporary amenorrhoea post-chemotherapy, but not duration of amenorrhoea, predicted a trend toward increased rates of infertility.
Currently, the most widely used and effective strategies for fertility preservation in cancer patients are oocyte and embryo cryopreservation, which require the patient to undergo controlled ovarian stimulation in preparation for oocyte retrieval. Historically, this treatment option was often associated with significant delays in starting cancer treatment, which led to anxiety on the part of both the patient and medical team. However, with a random start ovarian stimulation, there are now minimal delays, but it is potentially costly and invasive.
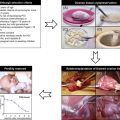
Another option, which has resulted in live births but is still considered experimental according to the American Society for Reproductive Medicine, is the cryopreservation of ovarian tissue. With this procedure, ovarian tissue is surgically removed and cryopreserved. The tissue can then be re-transplanted into the patient at a later time. Although pregnancies have been achieved, the efficiency of this method is controversial : this is discussed further in Chapter 7 .
Another option for fertility preservation that does not require cryopreservation of reproductive cells/tissues involves medical treatments that may protect the ovary. The most widely used agents are gonadotropin-releasing hormone (GnRH) agonists. Multiple clinical studies suggest a potential protective effect in patients receiving gonadotoxic chemotherapy, while others demonstrate no benefit. However, there are no data to support the use of GnRH agonists to protect the ovary from radiotherapy. In this chapter, we review the physiology of GnRH and the role of GnRH agonist co-treatment with chemotherapy for the protection of the ovary.
8.2
Distribution and Roles of the GnRH/GnRH Receptor System
8.2.1
GnRH
GnRH is a decapeptide synthesized by specific neurons located in the arcuate nucleus and in the preoptic area of the hypothalamus, and is released into the portal blood in a pulsatile fashion. GnRH binds with high affinity to specific G protein-coupled receptors on the surface of gonadotrope cells in the anterior pituitary, and induces biosynthesis and secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones act directly on the ovary, stimulating steroidogenesis and gametogenesis.
Twenty-three different isoforms of GnRH have been identified in various vertebrate species. All of these peptides consist of 10 amino acids and have a similar structure, with at least 50% sequence identity ; they have been named according to the species from which they were initially isolated. In mammals, the hypophysiotropic GnRH that stimulates the hypophysiotropic gonadotropin release was first isolated in pigs and is designated as GnRH-I (mammalian GnRH), while an early evolved and highly conserved new isoform that was discovered in the chicken is designated as GnRH-II (chicken GnRH). In addition, in mammals, a third isoform, the salmon GnRH, named GnRH-III, has been reported. In the human genome, only the GnRH-I and GnRH-II have been found. In humans, the expression of both GnRH-I and -II messenger RNA (mRNA) has been demonstrated in somatic and gonadal tissues such as the placenta, ovary, endometrium, trophoblast and the fallopian tubes in addition to in the hypothalamus.
8.2.2
GnRH Receptor
The GnRH receptor (GnRHR) is a member of the G protein-coupled serpent-like membrane receptors, which consist of seven hydrophobic transmembrane chains, connected to each other with extracellular and intracellular loops. Transmembrane chains participate in receptor activation and the transmission of signals, and intracellular loops are involved in the interaction with G proteins and also other proteins participating in the intracellular signal transmission. Upon GnRH binding, the GnRHR undergoes a conformational change and stimulates G proteins, which in turn produces downstream activation of several signalling cascades, mainly inositol 1,4,5-triphosphate (IP3) and diacylglycerol (DAG), MAPK and adenylyl cyclase pathways. Two homologous GnRHR have been identified: type I and type II. The absence of the carboxyl terminal tail results in slow internalization of type I GnRHR, and prevents rapid desensitization of the receptor. In humans, the conventional type I GnRHR is mainly expressed in gonadotropes in the anterior pituitary. However, it is also expressed in numerous extrapituitary tissues including placenta, breast, ovary, uterus, prostate and the corresponding cancer cells. The type II GnRHR has been cloned in marmoset as well as in non-human primates. This receptor does have the characteristic carboxyl terminal tail, which allows its rapid desensitization. However, a full-length type II GnRHR mRNA is absent in humans, as the open reading frame from the putative human type II GnRHR gene is disrupted by a frame shift, resulting in a premature stop codon.
8.2.3
GnRH and GnRHR Expression in the Ovary
In human ovaries, GnRHR mRNA expression was initially demonstrated in granulosa-luteal cells aspirated from preovulatory follicles of women undergoing infertility treatment with in vitro fertilization (IVF). Later, other researchers confirmed the presence of mRNA encoding for GnRHR in human granulosa-luteal cells and corpus luteum. However, it is noteworthy that the levels of GnRHR mRNA in the ovary are almost 200-fold lower than in the pituitary.
GnRH-I, GnRH-II and GnRHR protein expressions were not detected by immunostaining in the follicles from the primordial to the early antral stage. However, in preovulatory follicles, both forms of GnRH and their common receptor were immunolocalized, predominantly to the granulosa cell layer, whereas the theca interna layer was weakly positive. In the corpus luteum, significant levels of GnRH-I, GnRH-II and GnRHR were observed in granulosa-luteal cells but not in theca-luteal cells. Both GnRH isoforms and the type I GnRHR were also immunolocalized to the ovarian surface epithelium.
8.2.4
Direct Effect of GnRH in the Ovary
Consistent with its expression in the ovary, where its receptor is also detected, a direct effect of GnRH on ovarian cells has been demonstrated in animal models and humans. GnRH-I was found to inhibit DNA synthesis in vitro and to induce apoptosis in rat granulosa cells. In humans, GnRH-I has been reported to exert an inhibitory action on ovarian steroidogenesis, decreasing progesterone production. However, others have reported either a stimulatory effect or an absence of any effect. GnRH-II, similar to GnRH-I, inhibits progesterone secretion in human granulosa-luteal cells. GnRH-II also downregulates the receptors of FSH and LH. Apart from its effects on ovarian steroidogenesis, GnRH is also implicated in downregulation of cell proliferation and induction of apoptosis. GnRH-I has been suggested as a luteolytic factor, increasing the number of apoptotic luteinized granulosa cells. GnRH-I increased the number of apoptotic human granulosa cells obtained during oocyte retrieval for IVF. Both GnRH-I and GnRH-II act as negative autocrine/paracrine regulators of cell proliferation in ovarian epithelial cells. Therefore, in addition to its essential function of stimulating gonadotropin synthesis and secretion, GnRH seems to act as an autocrine and/or paracrine factor in the ovary, where it downregulates steroidogenesis and cell proliferation, and promotes apoptosis.
8.3
GnRH Agonists
GnRH agonists (e.g., goserelin, triptorelin, buserelin and leuprolide) are decapeptides, with similar structure to native GnRH and a great affinity to the GnRH receptors. After their binding to the receptors on gonadotropes, they initially cause gonadotropin release (flare-up effect). After several days of continuous administration, this is followed by a dramatic drop in the circulating concentrations of FSH and LH, through a desensitization mechanism. GnRH agonists have greater affinity for the GnRHR than native GnRH; they also have greater resistance to enzymatic breakdown and a prolonged half-life compared to native GnRH (i.e., native GnRH has a half-life of about 2 to 4 minutes compared to 3 h for the GnRH agonist leuprolide). The internalization of receptors and the slow dissociation of the agonist–receptor complex decrease the total number of functional GnRHR, leading to a prolonged desensitization. During treatment with GnRH agonists, high concentrations of GnRH agonists circulate and bind all the available GnRHR, both in central and peripheral tissues.
However, studies on the effects of GnRH agonists on ovarian steroidogenesis have come to contradictory conclusions. Some have shown a lack of direct effect, while others have reported either inhibition or stimulation of the production of oestrogen, progesterone, or both. An interesting finding reported recently was that the treatment of mouse granulosa cells with GnRH agonists failed to increase in cAMP, phosphorylated ERK or phosphorylated ERK p38, which are downstream effectors of all G-coupled protein signalling cascades that GnRH is known to stimulate. This controversial result can be explained by the presence of a different, yet unknown signalling pathway activated in the ovary by GnRH agonists.
8.4
GnRH Agonist Co-treatment with Chemotherapy for the Protection of the Ovary
8.4.1
Animal Studies
Based on the debated role of gonadal suppression in men in preserving testicular function against chemotherapy, and the belief that prepubertal girls are more resistant to gonadotoxic cancer treatment, the effect of GnRH agonists in preserving fertility by creating a prepubertal hormonal milieu has been investigated.
Animal studies have demonstrated a protective role of GnRH agonist treatment against chemotherapy-induced gonadal damage. Primordial follicle loss associated with cyclophosphamide treatment was significantly lower in rhesus monkeys receiving GnRH agonist treatment compared with untreated animals (65% vs. 29%, respectively). Interestingly, using the same model, a protective effect of GnRH agonist treatment was not observed after radiation therapy. Oocytes are extremely sensitive to irradiation, and it seems unlikely that radiotherapy-induced gonadal damage can be prevented by gonadal suppression.
In contrast to the protective effects of GnRH agonists, GnRH antagonists did not protect the ovary from chemotherapeutic damage. In a murine model, administration of GnRH antagonists not only did not prevent chemotherapeutic destruction of primordial follicles but also depleted primordial follicles, possibly through a direct effect on the ovary. However, in another murine model, pretreatment with a GnRH antagonist significantly decreased the extent of primordial follicle damage induced by chemotherapy. The discrepancy between these two studies may be due to the different treatment regimens or different strains of mice that were used.
8.4.2
Early Non-Randomized Studies in Human
Following encouraging findings in animal models, non-randomized studies with short term follow-up suggested a protective role for GnRH agonist co-treatment in women undergoing gonadotoxic chemotherapy. These studies were criticized for their lack of randomization, lack of proper controls, possible recall bias, different follow-up periods for treatment and control groups, and not controlling for confounders. In addition, these studies most often had ovarian failure as an end-point, which may not reflect the decrease in primordial follicle count (partial injury), the most common impact in response to chemotherapy in young women.
One of the largest studies, including 111 patients with Hodgkin lymphoma, was published by Blumenfeld et al. In that study, a monthly depot injection of GnRH analogue was administered starting before chemotherapy for up to 6 months, in parallel to, and until the end of, chemotherapeutic treatment. The main significant difference was the rate of POI, which was 3% (2/65) in the GnRH agonist co-treatment group versus 37% (17/46) in the control group. In the GnRH agonist-treated group, 48 pregnancies occurred in 34 patients, who were 18–33 years old at chemotherapy administration, compared with 22 pregnancies in 16 patients in the control group who were 16–26 years old at chemotherapy administration.
Both Huser et al. and Castelo-Branco et al. have reported similar results in patients with Hodgkin lymphoma in small case-control studies. Significantly lower rates of POI were found in women using GnRH agonist with chemotherapy (10.0–20.8%) compared to those in control groups (71.1–76.9%). These data suggest that the co-treatment of GnRH agonists in women undergoing chemotherapy for Hodgkin lymphoma may protect long-term ovarian function.
There are limited case-control studies evaluating the protective effect of GnRH agonists for other disease states. Recchia et al. investigated the protective effects on ovarian function and the efficacy and tolerability of goserelin, a GnRH analogue, added to adjuvant chemotherapy for early breast cancer. After a median follow-up of 55 months, with 94% survival, 86% of the patients had resumed normal menses, and 84% were disease-free. The 1-, 3- and 5-year projected recurrence-free survival rates were 100%, 81% and 75%, respectively. Five years after treatment, one patient had a pregnancy that ended with a normal birth. In another study, Recchia et al. retrospectively evaluated 100 consecutive premenopausal women with high-risk early breast carcinoma who received a GnRH agonist as ovarian protection during adjuvant chemotherapy. After a median follow-up of 75 months, normal menses were resumed in all patients younger than age 40 years and by 56% of patients older than age 40 years. Three pregnancies were observed that resulted in two normal deliveries and one elective termination of pregnancy. These data show that the addition of GnRH agonists to adjuvant therapy of premenopausal patients with early breast cancer is well tolerated and may protect long-term ovarian function.
GnRH agonist co-treatment may also be beneficial for young women receiving cytotoxic chemotherapy for benign diseases. Somers et al. demonstrated that the treatment with GnRH agonist in parallel to cyclophosphamide therapy was associated with a significant reduction of POI in young women with severe systemic lupus erythematosus. In their study, POI developed in one of 20 women treated with GnRH agonist (5%) compared with that in six of 20 controls (30%) matched by age and cumulative cyclophosphamide dose.
8.4.3
Randomized Clinical Trials in Women
The protective effect seen in small observational studies of GnRH agonists and chemotherapy on future ovarian function triggered multiple larger and prospective randomized studies in recent years ( Table 8.1 ). Most randomized trials to date have focused on whether GnRH agonists are protective in patients treated for breast cancer.
| Trial | No. of Patients | Type of Cancer | Median/Mean Age (GnRH Agonist vs. Control) | Study Arms | Follow-up (Month) | Definition of POI | POI Incidence in GnRH-Treated Women (%) | POI Incidence in Controls (%) | Significant? |
|---|---|---|---|---|---|---|---|---|---|
| Badawy et al. | 78 | Breast | 30 vs. 29.2 | CT+goserelin vs. CT | 3 to 8 | No resumption of spontaneous ovulation | 11% | 67% | Yes |
| Sverrisdottir et al. | 123 | Breast | 45 vs. 45 | CT±tamoxifen+goserelin vs. CT±tamoxifen | 36 | Absence of menses | 64% in gaserolin only, 93% in goserelin+tamoxifen | 90% in CMF only, 87% in CMF+tamoxifen | Yes only for gaserolin only group |
| Del Mastro et al. | 281 | Breast | 39 vs. 39 | CT+triptorelin vs. CT | 12 | No resumption of menstrual activity and postmenopausal levels of FSH and oestradiol | 9% | 26% | Yes |
| Song et al. | 183 | Breast | 40.3 vs. 42.1 | CT+leuprolide vs. CT | 12 | No resumption of menses | 40% | 59% | Yes |
| Gerber et al. | 56 | Breast | 35 vs. 38.5 | CT+goserelin vs. CT | 24 | No reappearance of two consecutive menstrual periods within 21–35 days | 30% | 43% | No |
| Munster et al. | 47 | Breast | 39 vs. 38 | CT+triptorelin vs. CT | 24 | No resumption of menses | 12% | 10% | No |
| Elgindy et al. | 100 | Breast | 32 vs. 33 | CT+triptorelin±GnRH antagonist vs. CT alone | 12 | No resumption of menses | 20% in “early CT” group, 16% % in “late CT” group | 20% in both “early and late CT” groups | No |
| Moore et al. | 135 | Breast | Not provided | CT+goserelin vs. CT | 24 | Amenorrhoea for the prior 6 months and post-menopausal FSH | 8% | 22% | Yes |
| Demeestere et al. | 84 | Lymphoma | 25.6 vs. 27.3 | CT+oral contraceptives+triptorelin vs. CT+oral contraceptives | 12 | FSH level≥40 IU/L | 20% | 19% | No |
In a clinical trial undertaken by Badawy et al. , 78 premenopausal breast cancer patients were randomly assigned to receive adjuvant chemotherapy (5-fluorouracil, doxorubicin (Adriamycin) and cyclophosphamide) with or without goserelin. The primary end-point of POI at 3–8 months post completion of chemotherapy demonstrated a significant benefit for patients receiving goserelin. Menstruation resumption was reported in 35 (90%) patients in goserelin/chemotherapy group versus 13 (33%) patients treated with chemotherapy alone (p<0.001). However, in this study the rate of POI (67%) in the chemotherapy-alone group was higher than expected and the follow-up period was short. These may negatively affect the reliability and generalizability of the results. In addition, the pregnancy rate after treatment was not reported. Importantly, no information was given on either breast cancer hormonal status or tamoxifen use.
The ZIPP (Zoladex In Premenopausal Patients) randomized study was designed to compare the survival rate of different endocrine therapy regimens in premenopausal breast cancer patients treated with or without adjuvant chemotherapy and/or radiotherapy. A subset of patients was also enrolled in a prospectively planned sub-study assessing ovarian function. Patients were randomized to one of four treatment arms: 1) control (no endocrine therapy); 2) goserelin; 3) tamoxifen; and 4) goserelin plus tamoxifen. All patients received endocrine therapy for 2 years, commenced concurrently with chemotherapy, regardless of oestrogen receptor status. In addition to endocrine therapy randomization, patients with node-positive disease received chemotherapy (cyclophosphamide, methotrexate and 5-fluorouracil), plus radiotherapy if four or more nodes were involved. From 260 assessable patients, 123 received six cycles of chemotherapy. At completion of endocrine therapy, amenorrhoea rates of 85% (control), 95% (tamoxifen), 97% (goserelin), and 92% (goserelin plus tamoxifen) were reported. Twelve months after completion of all therapy (36 months follow-up), there was a significant decrease in the amenorrhoea rate in patients treated with goserelin alone (64%) compared with persisting high rates for the other groups: 90% (control), 87% (tamoxifen), and 93% (goserelin+tamoxifen) (p=0.006). Interestingly, no decrease in amenorrhoea was seen in the combined goserelin plus tamoxifen group. This contradictory finding was not explained in the study. In this study, the definition of premenopausal status (i.e., the last menstrual period within the preceding 6 months, including regular or irregular menstruation, without a specific age cut-off) allowed inclusion of perimenopausal patients. This likely contributed to the very high amenorrhoea rates reported across all groups. Pregnancy rates after treatment were not reported.
A phase III trial from Del Mastro et al. assessed the efficacy of triptorelin in preventing chemotherapy-induced amenorrhoea when added to chemotherapy (cyclophosphamide, methotrexate and 5-fluorouracil, or anthracycline-based adjuvant or neoadjuvant chemotherapy) for breast cancer. With 281 enrolled patients, at a median follow-up of 12 months post-chemotherapy, the chemotherapy-induced amenorrhoea rate was significantly higher with chemotherapy alone (26%) compared with triptorelin/chemotherapy (9%) (p<0.001). In this study, contradictory to the previously reported risk factors for POI, only triptorelin treatment, but not age or chemotherapy type, was associated with the rate of chemotherapy-induced amenorrhoea rate. There were limited pregnancy outcomes following treatment. Twenty-four months after all patients had completed chemotherapy, one successful pregnancy in the control arm, and three pregnancies in the triptorelin group (resulting in two live births and one voluntary termination) were reported.
In a more recent phase II randomized trial, Song et al. examined the efficacy of leuprolide acetate on preserving ovarian function in patients with breast cancer. A total of 183 patients were included in this prospective clinical trial and were assigned randomly to receive cyclophosphamide–doxorubicin-based chemotherapy only or chemotherapy plus leuprolide acetate. At the end of the 12 month follow-up, a significantly higher percentage of patients resumed menses in the chemotherapy plus leuprolide acetate group (53 out of 89) compared to patients in the chemotherapy-only group (39 out of 94) (p<0.05).
At the time of writing, the OPTION (Ovarian Protection Trial In premenopausal breast cancer patients) randomized phase III trial has only been reported in abstract form. This trial was designed to assess the ovarian protective effect of goserelin compared with no goserelin in patients with oestrogen receptor-negative early breast cancer treated with anthracycline- and/or cyclophosphamide-based adjuvant chemotherapy, with the primary end-point being amenorrhoea rate at 12 months after completion of chemotherapy. At the time of reporting, 173 patients had adequate follow-up data and 140 had adequate information about menstrual bleeding. No difference between treatment arms was reportedly found; however, data on actual amenorrhoea rates between arms have not yet been published.
The phase II ZORO (ZOledex Rescue of Ovarian function) trial included 56 premenopausal patients (28 patients in each arm) with oestrogen receptor-negative breast cancer randomly assigned to receive neoadjuvant anthracycline/cyclophosphamide-based chemotherapy with or without goserelin. For the primary end-point of normal ovarian function, regular menstruation was reported in 70% versus 57% of patients treated with goserelin/chemotherapy versus chemotherapy alone, though this difference did not reach statistical significance. Similarly, there was no significant difference in the median time to resumption of menstruation: 6.1 versus 6.8 months for goserelin versus control group, respectively. There were limited pregnancy data available, with one pregnancy being reported in each treatment arm.
A randomized trial from Munster et al. compared ovarian function in breast cancer patients treated with adjuvant anthracycline-based±taxane chemotherapy with or without triptorelin. Ovarian function was defined as resumption of normal menstruation during follow-up of at least 2 years post-chemotherapy. Follow-up had been planned to extend to 5 years; however, the trial was terminated at interim analysis due to lack of effectiveness. Of the 49 patients enrolled, 27 patients received triptorelin/chemotherapy and 22 received chemotherapy alone. Most patients had oestrogen receptor-positive disease (73% and 74% for triptorelin and control groups, respectively). After a median follow-up of 18 months (range 5–43 months), resumption of menstruation was seen in 88% versus 90% for triptorelin versus control groups, respectively. Similarly, there was no significant difference in time to resumption of menstruation (5.8 vs. 5.0 months for triptorelin vs. control groups, respectively). Two pregnancies were reported, both in the control group. The number of patients attempting pregnancy was not given.
A phase II randomized trial from Elgindy et al. was designed to assess the potential benefit of triptorelin in two different groups of premenopausal oestrogen receptor-negative early breast cancer patients. The “delayed chemotherapy” group (i.e., patients not requiring immediate cytotoxic treatment) were randomly assigned to chemotherapy plus triptorelin or chemotherapy alone. Patients requiring immediate commencement of chemotherapy were allocated to the “early chemotherapy” group, and randomly assigned to receive chemotherapy with or without triptorelin plus cetrorelix, a GnRH antagonist. The primary end-point of the rate of resumption of menstruation 12 months after chemotherapy was similar across the treatment groups (80% [triptorelin] vs. 84% [control] for the “delayed chemotherapy” group; and 80% [triptorelin+cetrorelix] vs. 80% [control] for the “early chemotherapy” group).
The POEMS trial (Prevention of Early Menopause Study) included 214 women with hormone receptor-negative breast cancer under the age of 50 who were randomized to receive cyclophosphamide-containing treatment with or without monthly goserelin starting 1 week prior to the first chemotherapy dose. The primary study objective was to assess the rate of POI 2 years after chemotherapy, with POI defined as amenorrhoea during the previous 6 months along with postmenopausal concentrations of FSH. Only 135 patients had complete primary end-point data. The rate of POI was lower with goserelin (8%) compared to control group (22%) (OR, 0.3; 95% CI, 0.1–0.87; p=0.03). The birth rate and number of pregnancies were significantly higher in goserelin group (18%) compared to control (9%) (OR, 2.22; 95% CI, 1.00–4.92; p=0.05). During the follow-up, the patients treated with GnRH agonist also had improved disease-free and overall survival. The main strengths of the POEMS trial are the duration of follow-up with the demonstration of ovarian function resumption after 2 years and being the only study showing an increased pregnancy rate after using a GnRH agonist. The main limitation of the study is small sample size due to (a) early termination of the study due to lack of recruitment and financial support (the study had originally planned to randomize 400 patients), and (b) high drop-out rate (38%) due to death or lack of FSH data.
There is only one randomized trial reported on whether GnRH agonists are protective in patients undergoing chemotherapy for lymphoma. In the study by Demeestere et al. 84 patients were randomly assigned to receive either triptorelin plus norethisterone (GnRH agonist group) or norethisterone alone (control group) concomitantly with alkylating agent-based chemotherapy. After 1 year of follow-up, similar percentages of patients experienced POI in the GnRH agonist (20%) and control (19%) groups. More than half of patients in each group completely restored their ovarian function, but the anti-Müllerian hormone values were higher in the GnRH agonist group than in the control group (1.4±0.35 vs. 0.5±0.15 ng/mL, respectively; p=0.04).
In summary, although animal and observational studies suggest that GnRH agonists may have protective effect in the ovary against chemotherapy, randomized trial outcomes are limited and inconsistent for breast cancer patients. Thus, the outcomes cannot be generalized to other cancer types. Despite a number of studies focused on one cancer type, these inconsistent results may stem from heterogeneity of study designs including cancer diagnosis, hormone receptor status in breast cancer, type and duration of the applied chemotherapeutic agents and GnRH agonists, the age of the patient population, definition of POI and follow-up period. The major issues in these clinical trials are small sample size, lack of long-term follow up and fertility/pregnancy information (except POEMS study). Also of concern is that, in most studies, there is lack of control for the confounding effects of tamoxifen, with tamoxifen being a known independent risk factor for amenorrhoea. This tamoxifen effect was excluded in the ZORO, OPTION and POEMS studies by exclusive inclusion of patients with hormone receptor-negative tumours. It was hypothesized that in order for GnRH agonist to prevent ovarian damage, treatment should commence at least a week before chemotherapy. However, in several studies, some patients received GnRH agonist at the commencement of chemotherapy, by which point potential efficacy might be diminished.
8.4.4
Meta-Analysis
Four recent meta-analyses have examined the efficacy of GnRH agonists on the resumption of menses after chemotherapy treatment for cancer, and again reported conflicting results due to inclusion of different studies in each meta-analysis. The first meta-analysis consisted of six trials that examined the reproductive outcomes among women with Hodgkin disease, ovarian cancer and breast cancer. It suggested a potential benefit of GnRH agonist in premenopausal women undergoing chemotherapy for cancer, with significantly higher rates of spontaneous resumption of menses (OR, 3.46; 95% CI, 1.13–10.57) and ovulation (OR, 5.70; 95% CI, 2.29–14.20) in the GnRH agonist cohort compared with in the controls. There was no statistically significant difference in the occurrence of spontaneous pregnancy (OR, 0.26; 95% CI 0.03–2.52). A recent meta-analysis consisting of nine trials that examined the efficacy of GnRH agonist, given before and during chemotherapy, for the prevention of POI in premenopausal women with Hodgkin disease, ovarian cancer and breast cancer also reported a significant reduction in the risk of POI (OR, 0.43; 95% CI, 0.22–0.84) in patients receiving GnRH agonist. Another meta-analysis assessed the efficacy of GnRH agonist on the prevention of chemotherapy-related POI among breast cancer patients in the first year after treatment. It included five randomized trials and found significantly fewer women treated with GnRH agonist to have POI compared with the placebo group (RR, 0.40; 95% CI, 0.21–0.75) but similar rates of menses resumption (RR, 1.31; 95% CI, 0.93–1.85) and spontaneous pregnancy (RR, 0.96; 95% CI, 0.20–4.56). The most recent meta-analysis, evaluating the effect of concurrent use of GnRH agonists with chemotherapy on ovarian function in women with breast cancer who did not use tamoxifen, included four randomized trials. This meta-analysis failed to demonstrate any significant effect of GnRH agonists on the rate of resumption of spontaneous menses (OR, 1.47; 95% CI, 0.60–3.62).
In these meta-analyses, the obvious lack of uniform chemotherapy regimens, follow-up duration, and POI definition negatively impacted accurate analyses. In addition, there was a major heterogeneity of the primary trials with regard to inclusion or exclusion of oestrogen receptor-positive breast cancer patients and treatment with tamoxifen. Treatment with tamoxifen is a significant potential source of bias in individual studies. The inconsistent age of patients included in the clinical trials may also have led to bias in these meta-analyses. Overall, even after these meta-analyses, the assessment of ovarian protection of GnRH agonists against chemotherapeutic agents is still inconclusive.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree