Fig. 23.1
Arrows show the flow of heat (FH) differences between different materials
In a fast frozen tissue, temperature drops can be visualized as isotherms being at the center of the lesion, the area with the lowest temperature. The cryosurgeon will need to guarantee that the required −50 °C needed to destroy cancer cells is at the bottom of the tumor. The easiest way is to measure it at the periphery of the tumor (Fig. 23.2). The knowledge of the shape of the tumor will be important in determining the required margins. As a general rule, the margins to be frozen are the same than when removing a tumor by surgery.
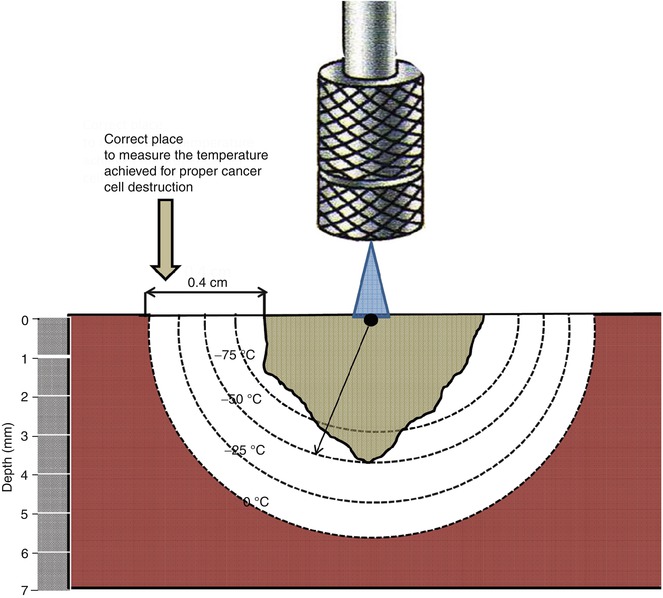
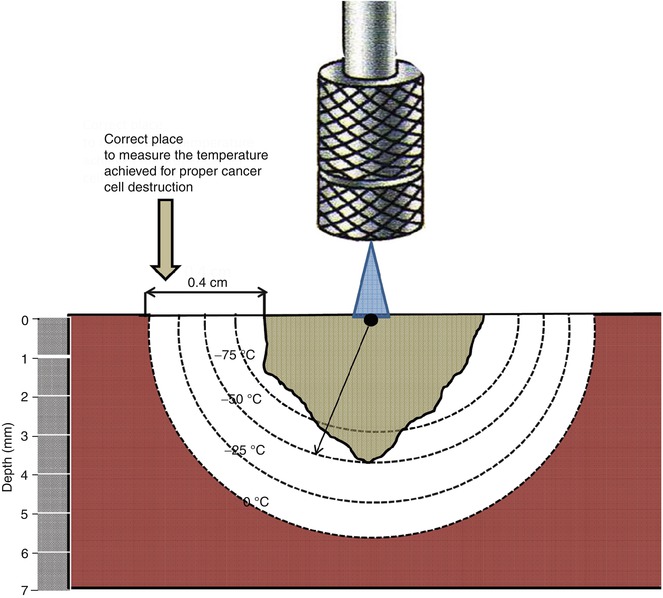
Fig. 23.2
Schematic view of the isotherms. As we move further down from the freezing source, temperatures are higher in depth and laterally
Basic Principles
The molecular basis for destruction with sub-zero temperature can be summarized as follows [2–4] (Table 23.1):
Table 23.1
Molecular basis of cryosurgical injury
Mechanism | Time of cycle | Location | |
|---|---|---|---|
Direct injury | Intracellular ice crystal formation; followed after days by coagulation necrosis | Freezing phase | Center |
Vascular injury | Microcirculatory failure | Thawing phase | Periphery |
By apoptosis | Cell death by apoptosis | Up to 8 h after rewarming | Periphery |
Immunologicala | Dendritic cell mediated | Late event | Periphery |
1.
Direct injury. With initial freezing, water crystals form outside the cells. This generates a hyperosmotic environment and subsequent water movement out of the cell. Internal dehydration initiates membrane and organelle damage. As freezing is maintained, there is water crystal formation inside the cell which results in cell bursting. As the tissue thaws, crystals reorganize forming newer and larger crystals that cause further destruction.
In addition, the mechanical damage generated at the membrane level adds to the metabolic failure caused by ionic changes, pH decrease, and lipid alteration, all leading to further permeability alterations.
Most of the direct damage occurs during the freezing period, causing cell death by necrosis mainly at the center of the lesion.
2.
Vascular injury. Cold generated severe vasoconstriction with subsequent decrease in the blood flow. With thawing, the tissue becomes congested due to vasodilation and vascular damage. Eventually, there is platelet aggregation and microthrombi formation which leads to vascular stasis. Thawing brings about hyperperfusion, free radical formation, and further membrane damage. Blood supply due to microcirculation failure occurs in about 1 h from freezing and causes death by ischemia, evident at the periphery of the cryoinjury.
3.
Apoptosis. Cell death by apoptosis is a phenomenon seen at the periphery of the cryoinjury that occurs as a late event (2–8 h after freezing) [5].
Equipments
The equipment required for office cryosurgery is commercially available through different manufacturers. It consists of a unit to deliver the LN, diverse attachments, tank to store LN, and other accessories (Fig. 23.3).


Fig. 23.3
Dewars, gloves, withdraw device, and Cry-Ac® TrackerCam™
Handheld Unit
These units are used to deliver the cryogen. They have to hold enough LN to allow the cryosurgeon to perform several procedures without filling the tank every time. Large units hold more LN but weigh more and are cumbersome to handle. Excess in weight or in diameter of the units can result in loss of accuracy. This is the reason why the ideal unit size ranges from 300 to 500 cc. The most popular commercially available units are made by Brymill Corporation. Further developments in the unit have produced the Cry-Ac® Tracker (Brymill) which is the only unit that measures the temperature on the skin as LN is delivered to the target lesion and the newest Cry-Ac® TrackerCam™ which measures temperatures, monitors freezing, and records the procedure.
Other manufactures are Erbokryo derm, Wallach (UltraFreeze tm; units available in 300 and 500 cc), or Cortex (Cryopro, in 500 and 350 cc units).
Attachments and Other Delivery Gadgets (Fig. 23.4)


Fig. 23.4
(a) Spray tips. (b) Probes. (c) Chambers. (d) Cones. (e) Tweezers
Tips or apertures are devices that can be screwed at the open end of the unit and allow the output of LN through openings of predetermined size. They are named with letters: A, 0.04 in.; B, 0.03 in.; C, 0.022 in.; and D, 0.016 in. The larger the openings, the larger the release of LN. They are used for cryospray technique.
Probes are metal extensions usually covered by Teflon (to avoid sticking to the surface). They come in different sizes (cylindrical, conical, ball shaped, half-moon, sharp-pointed conical, concave, flat elongated). They have an internal conduit line that freezes the metal from the inside maintaining a continuous low temperature. They are used for close cryosurgery.
Chambers are metal cylinders with one of the endings screwed onto the opening of the unit while the free open end has a rubber ring to protect the skin. Once applied over the target lesion, LN is released and maintained inside the chamber (by applying a discrete pressure on the skin). LN turbulence generates inside the chamber and allows extremely powerful freezing. They are considered a variation of the open technique and its use is limited to the treatment of lesions where destruction in depth is important. They are reserved to advance malignancies like skin metastasis.
Cones are cylinders, open at both ends, used to confine LN as it is delivered to the target lesion through a tip or aperture. They help protect the healthy skin that surrounds the target (not meant to be destroyed). They also constrain and direct the flow of LN to the delimited area, making freezing more effective. They come in different sizes and are made of neoprene (sizes are 6, 11, 16, 25, 30, and 38 mm) or plastic (very useful are the ones used in otoscope). A device called cryoplate that consists of a Lexan plate with four conical openings (4, 7, 9, and 12 mm) is another alternative. These are all variants of the open technique. It is usually used in benign lesions.
Tweezers have been designed for benign lesions. However, they can be used to grasp exophytic tumors. A modified tweezer (with one ending attached at the unit for continuous LN flow) was designed by our team for use in large vascular tumors (Fig. 23.5).


Fig. 23.5
Tweezers used in SK tumors of the leg
Extensions (bend or straight) are meant to attach applicators or probes. They are used to treat hard-to-reach lesions, keeping the unit straight and maintaining precision. Luer lock adapters can be used to hook in needles or other probes. Back vent adapter eliminates intermittent spray (useful for continuous flow over a large tumor).
Dewars. LN needs to be stored in special dewars capable of maintaining the gas restrained within it and at the same time, allow some small amounts to evaporate to avoid pressure build up on the insides. The quality of the cover is very important in determining the duration of stored LN. They come in different sizes: 5, 10, 20, 30, and 50 L capacity. The intermediate sizes (20–30 L) tend to be more practical because they hold enough LN to last for 1–2 months unlike the smaller ones and are more manageable than the 50 L. A 5 L dewar can be used to place the residual LN of a larger dewar while waiting to get it filled again. There is a LN generator (MMR technology® ideal for offices located away from distribution networks.
Gloves, Roller Base for Dewars, Withdrawal Device. These are optional gadgets that can be useful for manipulating LN. Gloves protect from accidental spilling and the roller base helps move the dewar from one side to another (meant for large ones); the withdrawal device comes in two models: one that affixes to dewars and stays there until new refill. LN is released by opening a faucet; the other is meant to be fit every time the unit has to be refilled and offers instant pressurization, and once the unit is filled, it is removed, and the dewar cap is placed back.
Techniques
These are basically:
1.
Spray or open technique
2.
Cone or semi-open technique
3.
Probe or close technique
4.
Chamber or semi-closed technique
5.
Tweezer
6.
Intralesional
In skin cancer, the most commonly used are spray, probe, and chamber.
Spray or Open Technique
The open technique is probably the most common one. It is the technique of choice for benign lesions and in numerous skin cancers. LN is released through tips with apertures of known diameter. The most commonly used is the C tip (0.022 in./0.56 mm). Other apertures are A, 0.04 in./1.02 mm; B, 0.031 in./0.079 mm; D, 0.016 in./0.41 mm; and E, 0.013 in./0.33 mm. Luer lock adapters will be useful to use in different gauge needles, whenever in need of a more delimited freezing.
Extensions can be located between the unit and the tip to allow the operator to reach areas not readily exposed, such as mouth, earlobe, or canal. There are 1″ × 20 g Straight Spray and 3″ × 20 g Bent Spray.
The larger tips will release largest amounts of LN and therefore, freezing will be faster and deeper. Distance from the target tissue and direction of the spray are also elements to take into consideration (Fig. 23.6).
Fig. 23.6




Effects of (a) distance (the closer to the skin, the lower the final temperature in the skin) (b) inclination: the area closer to the freezing tip will have a lower final temperature (c) aperture of the orifice the larger the orifice, more LN will get to skin resulting in a lower final temperature. Aperture (A) is 0.04 in and aperture (D) is 0.016 in
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree