Acute onset dyspnea
80 %
Gradual onset dyspnea
3 %
Orthopnea
0.4 %
Chest pain
49 %
Syncope
24 %
Hemoptysis
6 %
As discussed below, although these symptoms are often due to serious disease, they are non-specific and thereby non-diagnostic. A study comparing symptoms in patients with (n = 1880) and without (n = 528) PE found no relevant differences in symptoms between the groups. The results are seen in Table 2.
Symptom | PE proven (%) | PE not proven (%) |
|---|---|---|
Dyspnea | 50 | 51 |
Pleuritic chest pain | 39 | 28 |
Cough | 23 | 23 |
Substernal chest pain | 15 | 17 |
Fever | 10 | 10 |
Hemoptysis | 8 | 4 |
Syncope | 6 | 6 |
Unilateral leg pain | 6 | 5 |
Signs of deep vein thrombosis | 24 | 18 |
Another study found significant differences in the frequency of sudden onset dyspnea, gradual onset dyspnea, orthopnea, pleuritic and substernal chest pain and fainting when studying 202 patients with, and 298 patients without PE. However, this is not clinically significant, as all symptoms can be present and absent in patients with PE. The results are seen in Table 3.
Symptom | PE proven (%) | PE not proven (%) |
|---|---|---|
Dyspnea (sudden onset) | 78 | 29 |
Dyspnea (gradual onset) | 6 | 20 |
Orthopnea | 9 | 9 |
Chest pain (pleuritic) | 44 | 30 |
Chest pain (substernal) | 16 | 10 |
Fainting | 26 | 13 |
Hemoptysis | 9 | 5 |
Cough | 11 | 15 |
Palpitations | 18 | 15 |
The pathophysiology of dyspnea in PE is probably multifactorial and includes hypoxemia and stimulation of pressure receptors in the right atrium (Manning and Schwartzstein 1995). When present, chest pain in PE is often pleuritic, i.e. worsening during inspiration, and is thought to be caused by lung infarction and pleural irritation (Stein and Henry 1997). This is also the background for alveolar hemorrhage and hemoptysis seen in PE. However, chest pain in PE can also mimic acute myocardial infarction. In these cases the pain probably originates from right ventricular strain with pressure overload and decreased coronary perfusion. Syncope is often a sign of reduced cardiac output and massive PE.
Four main symptoms of PE (acute onset dyspnea, chest pain, syncope, and hemoptysis) are almost always present, either alone or in combination, if the patient is not asymptomatic. In Table 4, this is summarized.
Only one of four symptoms | 42 % |
Any two of four symptoms | 41 % |
Any three of four symptoms | 11 % |
At least one of four symptoms | 94 % |
Other symptoms | 2 % |
Symptoms and signs of deep vein thrombosis only | 3 % |
No symptoms at all | 1 % |
When interviewing the patient suspected of PE, the focus must be on these symptoms and the duration, but in addition the interview must clarify risk factors for PE and possible contraindications to treatment.
2.3 Clinical Findings
In all patients with acute cardiopulmonary symptoms, vital signs like heart rate, blood pressure, arterial oxygen saturation, and respiratory frequency, should be recorded immediately, as these are fundamental during initial resuscitation and in risk stratification if PE is confirmed. However, no clinical important differences in vital signs are found between patients with or with-out PE (Goldhaber 2010).
Likewise, no physical findings are reported to either confirm or rule-out PE, although signs of deep vein thrombosis are found more frequently in patients with PE than patients without PE (Kline et al. 2004; Wells et al. 2000; Perrier et al. 2004; Le Gal et al. 2006). Clinical findings like wheezing and high fever are found more often in patients without PE, and suggest other diagnosis (Miniati et al. 2008; Stein et al. 2000; Kline et al. 2002; Kabrhel et al. 2006). Table 5 presents findings from 202 patients with and 298 patients without PE; differences in the frequency of leg swelling, high fever and wheezing between the two groups were statistically significant, but have limited clinical significance.
Clinical finding | PE proven (%) | PE not proven (%) |
|---|---|---|
Tachycardia > 100/min | 24 | 23 |
Cyanosis | 16 | 15 |
Hypotension < 90 mm Hg | 3 | 2 |
Neck vein distension | 12 | 9 |
Leg swelling (unilateral) | 17 | 9 |
Fever > 38 °C | 7 | 21 |
Crackles | 18 | 26 |
Wheezes | 4 | 13 |
Pleural friction rub | 4 | 4 |
2.4 Differential Diagnosis
In general, patients presenting to the emergency room with respiratory impairment like tachypnea and hypoxemia most commonly suffers from one of the conditions seen in Table 6 (Ray et al. 2006). By nature, the distribution of these conditions will vary in different patient populations, e.g. children or very specialized centers.
Cardiogenic pulmonary edema | 43 % |
Community acquired pneumonia | 35 % |
Acute exacerbation of obstructive pulmonary disease | 32 % |
Pulmonary embolism | 18 % |
Acute asthma | 3 % |
Other, common and uncommon, diseases with symptoms and clinical findings mimicking PE by causing dyspnea are lung malignancies, cardiac or intrapulmonary shunt states, pneumothorax, interstitial lung diseases, pulmonary hypertension and tracheobronchial foreign bodies. In addition, non-cardiopulmonary conditions like severe anemia, obesity and certain neuromuscular diseases can result in dyspnea.
In the patient presenting with chest pain, syncope and hemodynamic instability, acute myocardial infarction, malignant cardiac arrhythmias, aortic dissection, ruptured aortic aneurism, and other forms of shock must be included as possible differential diagnosis (Finfer and Vincent 2013).
2.5 Risk Factors for PE
Even though Virchow’s Triad (consisting of abnormal blood composition, vessel wall abnormalities and stasis) has been used for more than a century to describe risk factors for VTE, the clinical value of this has recently been questioned and additional details and interactions between the three components have been suggested (Wolberg et al. 2012). In some patients, it is not possible to establish any obvious risk or disposing factors for PE (White 2003).
However, if one or more risk factors are demonstrated, it is important if these are temporary (like recovery from surgery) or permanent (like incurable cancer). In other words, it must be decided whether the patient has secondary/provoked or primary/unprovoked/idiopathic PE. The thrombophilias constitutes a separate entity, and are covered in details in another chapter.
Table 7 (modified from (Anderson and Spencer 2003)) shows important relative risk factors for PE.
Strong risk factors (odds ratio >10) | Moderate risk factors (odds ratio 2–9) | Weak risk factors (odds ratio < 2) |
|---|---|---|
Fracture (hip or leg) | Arthroscopic knee surgery | Bed rest > 3 days |
Hip or knee replacement | Central venous lines | Immobility due to sitting (e.g. prolonged car or air travel) |
Major general surgery | Chemotherapy | Increasing age |
Major trauma | Congestive heart or respiratory failure | Laparoscopic surgery (e.g. cholecystectomy) |
Spinal cord injury | Hormone replacement therapy | Obesity |
Malignancy | Pregnancy/antepartum | |
Oral contraceptive therapy | Varicose veins | |
Paralytic stroke | ||
Pregnancy/postpartum | ||
Previous venous thromboembolism | ||
Thrombophilia |
In recent years more focus has been on VTE and arterial thrombosis sharing the same risk factors, and this has to be taken into account when assessing the patient with PE; both during diagnosis, treatment and prophylaxis of PE (Piazza 2015). The traditional risk factors for arterial thrombosis which are also recognized as risk factors for VTE and PE, are seen in Table 8 and are based on a metaanalysis of 63,552 patients (Ageno et al. 2008; Goldhaber 2010) (Table 9).
Table 8
Risk factors for VTE and PE traditionally seen as risk factors for arterial thrombosis (Ageno et al. 2008)
Diabetes mellitus |
Hypercholesterolemia |
Hypertension |
Obesity |
Smoking |
In-patient population | Out-patient population |
|---|---|
Major surgery | Advancing age |
Cancer | Cancer |
Congestive heart failure | Prior VTE |
Chronic obstructive pulmonary disease | Venous insufficiency |
Chronic kidney disease, especially nephrotic syndrome | Pregnancy |
Trauma | |
Frailty and immobility |
2.6 PE in Different Medical Specialties
In 2011, almost 200,000 patients in the United States were admitted with PE (LaMori et al. 2015), and every year 300,000 and 600,000 patients with PE are diagnosed in Europe and United States, respectively (Cohen et al. 2007; Garcia et al. 2005).
However, these numbers are not of direct utility to the individual clinician, as the incidence varies widely across medical specialties. In some fields of practice, PE is very common. For example, some studies suggest that 20 % of patients admitted with exacerbation of chronic obstructive pulmonary disease in fact have PE (Rizkallah et al. 2009; Kim et al. 2014). Also patients with liver cirrhosis and different autoimmune diseases have increased risk of PE (Ng et al. 2015; Tamaki and Khasnis 2015). In the emergency department, up to 1/400 will be diagnosed with PE (Kline and Kabrhel 2015a). Even though PE in pregnancy, and especially in the postpartum period (Meng et al. 2015), is fairly uncommon with 0.1 % of pregnant woman developing PE (Neuberger and Wennike 2013; Simpson et al. 2001), the risk is increased (Heit et al. 2005), and PE is a leading cause of maternal mortality in developed countries (Khan et al. 2006). In addition, the impact of PE in this patient category is often more complex with ethical and legal aspects in addition to the tragic nature of the situation. In surgery, increased risk of PE has to be taken into account in many specialties – e.g., 5 % of patients undergoing urooncological surgery will develop PE (Kukreja et al. 2015), in orthopedic surgery, 1 % of patients undergoing lower extremity surgery developed PE (Park et al. 2015; Wahlsten et al. 2015; Dixon et al. 2015) and the same is the case in patients with severe trauma and spine surgery (Lichte et al. 2015; Hamidi and Riazi 2015). Even in psychiatry, increased risk of PE is found in schizophrenic patients with a twofold risk of PE (Hsu et al. 2015). The examples above are by no means exhaustive, but meant as illustrations that clinicians in every field of medicine must have some knowledge of PE.
3 Basic Work Up
When assessing patients with acute cardiopulmonary symptoms, a range of investigations is indicated. In most patients, arterial gas analysis, chest x-ray, electrocardiogram (ECG) and venous blood samples are performed. In the following, the usefulness of these examinations in suspected PE will be reviewed.
Recently, focused point-of-care ultrasonography of the lungs, heart and deep vein have gained popularity in some centers, and seems utterly applicable in patients with respiratory symptoms and hypoxemia, increasing the number of patients with correct diagnosis at 4 h from admission from 64 to 88 % (Laursen et al. 2014). Ultrasonography of the lungs, heart and deep veins in the primary evaluation of these patients have several advantages in addition to establishing differential diagnoses to PE. Firstly, lung ultrasound has, in a recent meta-analysis, been found to have sensitivity of 87 % and specificity of 82 % for the diagnosis of PE (Squizzato et al. 2013). In addition, ultrasonography of the heart (echocardiography) will aid in risk stratification (as described later) and ultrasound of the deep vein can reveal deep venous thrombosis which will increase the possibility of PE in patients with relevant symptoms. However, while lung ultrasound has obvious benefits, is radiation free and can be used bedside, important limitations, primarily concerning training issues and interobserver variability exists (Touw et al. 2015).
3.1 Arterial Gas Analysis
Arterial blood gas measurements are fundamental when evaluating patients with acute respiratory impairment. Hypoxemia is present in most patients with PE, but is also present in many other conditions. The same is true for hypocapnia and abnormal (A–a) DO2 gradient (Rodger et al. 2000). Thus, the arterial blood gas is generally not helpful in making or excluding the diagnosis, but is important in determining severity and emergency treatment in patients with respiratory distress. However, some papers have demonstrated a lower PaCO2 in patients with COPD and PE, than in patients with COPD exacerbation without PE. Therefore, unsuspected hypocapnia in a patient with COPD exacerbation could be a clue that PE is present (Akpinar et al. 2014).
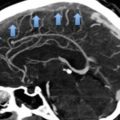
3.2 Chest X-Ray
Most patients with PE present with some abnormalities on the chest x-ray. These are, however, almost always non-specific and classical findings in PE like the Westermark sign (distal oligemia due to PE) are, although with varying frequency, only seen in a minority of patients (Miniati et al. 1999; Elliott et al. 2000; Stein et al. 1991b). Table 10 presents findings from the ICOPER study which studied around 2300 patients with PE.
Chest x-ray finding | % of patient with PE with finding | No. of patient with finding/no. interpreted |
|---|---|---|
Cardiac enlargement | 27 | 622/2315 |
Pleural effusion | 23 | 523/2319 |
Elevated hemidiaphragm | 20 | 457/2316 |
Pulmonary artery enlargement | 19 | 443/2305 |
Atelectasis | 18 | 410/2310 |
Infiltrate | 17 | 400/2317 |
Pulmonary congestion | 14 | 330/2316 |
Oligemia | 8 | 196/2315 |
Pulmonary infarction | 5 | 117/2312 |
Overinflation | 5 | 121/2319 |
When pleural effusion is present, it is present only as blunting of the costodiaphramatic angle in the large majority of patients (Stein et al. 1991a). A large pleural effusion should therefore not be contributed to PE, but investigated further to exclude other diagnosis like e.g. malignancy even though PE has been confirmed.
In general, the chest x-ray is important as an initial investigation in patients with clinical features of PE, as important differential diagnosis, like pneumothorax, can be diagnosed this way and typically leaves other more advanced diagnostic modalities redundant.
3.3 ECG
Multiple ECG changes in PE have been reported, and most patients with PE, depending on severity, have abnormal ECG (Stein et al. 1991b). Although some findings, like signs of right ventricular overload, are significant more frequently present in patients with PE than without (49.5 % vs. 12 %, P < 0.00001) (Miniati et al. 1999) the findings cannot by themselves either rule in or out PE. The ECG therefore serves primarily as an important tool in differential diagnostics. Conditions like acute coronary syndrome and ventricular arrhythmia can clinically mimic PE and can be diagnosed by ECG. Table 11 outlines findings on ECG in documented PE (from Stein et al. 1975).
Table 11
ECG findings in PE
ECG finding | % of patients with massive or submassive PE with finding |
|---|---|
Normal electrocardiogram | 13 |
Rhythm disturbances | |
Premature atrial beats | 2 |
Premature ventricular beats | 3 |
Atrio-ventricular conduction disturbances | |
First degree A-V block | 1 |
P pulmonale | 6 |
QRS abnormalities | |
Right axis deviation | 7 |
Left axis deviation | 7 |
Clockwise rotation (V s) | 7 |
Incomplete right bundle branch block | 6 |
Complete right bundle branch block | 9 |
Right ventricular hypertrophy | 6 |
S1S2S3 Pattern | 7 |
S1Q3T3 Pattern | 12 |
Pseudoinfarction | 11 |
Low voltage (frontal plane) | 6 |
Primary RST segment and T wave abnormalities | |
RST segment depression (not reciprocal) | 26 |
RST segment elevation (not reciprocal) | 16 |
T wave inversion | 42 |
When signs of right heart strain are present on ECG, it is associated with worse prognosis (Hariharan et al. 2015). For example, in one study 29 % of patients with PE and ECG changes died during the admission, whereas this was only the case in 11 % of patients without ECG changes (Geibel et al. 2005).
3.4 Biochemical Analyses
Presently, three biochemical analyses have gained interest in the work-up of pulmonary embolism. These are fibrinogen d-dimer, (N-terminal-pro)-brain-natriuretic peptide (BNP) and the cardiac troponins T and I (TNT and TNI).
Different d-dimer assays are available, with different diagnostic performance. When using a high sensitivity-assay like the the quantitative enzyme-linked immunosorbent assay (ELISA) or ELISA-derived assays, the sensitivity and negative predictive values are very high (Stein et al. 2004). However, many agree that a negative d-dimer should not rule out PE when the clinical probability is high.
No d-dimer assay has sufficient specificity to confirm PE, as increased d-dimer is a non-specific marker of activation of the coagulation system. A recent review have summarized conditions described to cause elevated d-dimer, and of notice is that many of these conditions are also present in patients typically suspected of PE which can render d-dimer testing in these patients useless. The factors that, among others, can cause false-positive d-dimer are increasing age, cocaine use, immobility, hemoptysis, hemodialysis, malignancy, rheumatoid arthritis, systemic lupus erythematosus, sickle cell disease, pregnancy, postpartum state and surgery (Kline and Kabrhel 2015b).
BNP is released in right ventricular pressure overload as seen in more severe PE (Henzler et al. 2012). The test is not useful in the diagnosis or exclusion of PE, but a low value is useful to identify patients with low risk of adverse events and thereby candidates for early discharge and out-patient management (Coutance et al. 2011; Klok et al. 2008; Vuilleumier et al. 2009; Hardeman et al. 2010).
TNI and TNT are released in myocardial infarction. Right ventricular infarction can occur in PE, and is a sign of severe PE. The use of TNI and TNT has been studied in PE, and most reports have shown a connection between the release of TNI and TNT and a worse prognosis and higher risk of adverse events. As an example, a recent study showed that negative high sensitivity TNT has a very high negative predictive value of adverse events like mortality (Lankeit et al. 2011).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree