CLINICAL APPLICATIONS OF THYROID-STIMULATING HORMONE MEASUREMENT
THYROID-STIMULATING HORMONE ASSAY
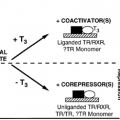
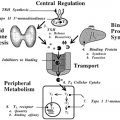
The radioimmunoassays initially used for routine clinical measurement of TSH have been replaced by more sensitive two-site noncompetitive immunometric assays (IMAs). These assays use two antibodies with specificity toward separate epitopes on TSH. One antibody is attached to a solid-phase support and the other antibody is labeled. Enzymes, luminescent or fluorescent compounds, and iodine-125 have been used as antibody labels.28,44 Luminescent labels now are used most commonly. Binding of the two antibodies to TSH results in the formation of a labeled “sandwich” that is separated from the noncomplexed reagents and measured. IMAs are specific for the measurement of TSH and generally free from interference. Rarely, falsely elevated serum TSH levels have been reported because of the presence in serum of heterophilic antibodies that neutralize the reagent anti-TSH antibody.45
With the introduction of the IMAs, a confusing nomenclature has developed based on the claimed sensitivity (e.g., “highly sensitive,” “ultrasensitive,” “supersensitive”). The American Thyroid Association has proposed that assays should be characterized by a functional criterion and that a TSH assay should be designated as “sensitive” only if sera from thyrotoxic persons yield results >3 log standard deviations below the mean of normal euthyroid persons.46 More than 95% of sera from thyrotoxic persons would be expected to have TSH levels below the lower limit of normal in an assay meeting this criterion. Most commercial IMAs appear capable of meeting that standard.47
Clinical chemists have traditionally reported as the analytic sensitivity or detection limit of an assay the lowest TSH level statistically distinguishable from zero concentration by measurement of replicate samples in the same assay run. Such a definition of sensitivity may be clinically misleading, because a single measurement of a specimen containing TSH at the analytic threshold concentration would yield a result of zero 50% of the time. Furthermore, analytic sensitivity is a function of within-assay variance and does not assess the reliability of between-assay comparisons, which are more likely to be clinically useful in the diagnosis and treatment of an individual patient. As an alternative to analytic sensitivity, the proposal has been made that assay sensitivity be characterized by a criterion based on interassay variability. Specifically, the “lower limit of interassay quantitative measurement,”48 or functional sensitivity, of an assay is the TSH concentration for which the interassay coefficient of variation is less than some preestablished threshold (generally 20%) to permit reliable quantitative comparisons between specimens measured in different assay runs.
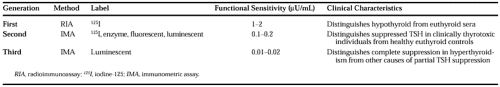
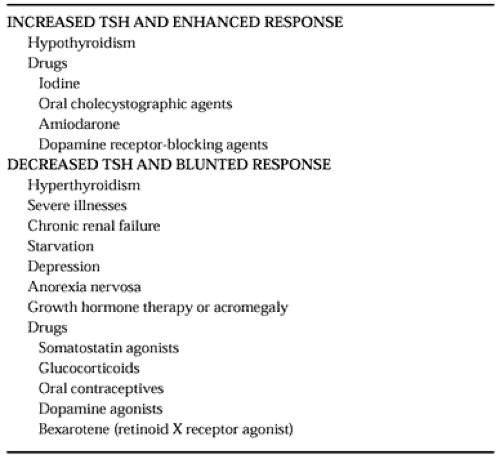
A “generational” classification of TSH assays has been proposed49 (Table 15-2). Each generation is approximately an order of magnitude more sensitive than the previous one. Both second- and third-generation assays distinguish suppressed TSH levels in hyperthyroidism from normal values. However, the third-generation assay further differentiates partial suppression of basal TSH concentrations in some patients with
subclinical hyperthyroidism, nonthyroid illness, glucocorticoid therapy, and other clinical states (Table 15-3) from the more complete suppression of basal TSH concentrations in overt hyperthyroidism.50
subclinical hyperthyroidism, nonthyroid illness, glucocorticoid therapy, and other clinical states (Table 15-3) from the more complete suppression of basal TSH concentrations in overt hyperthyroidism.50
Measurement of TSH is frequently used as the initial, and sometimes sole, thyroid function test.51 This approach is generally sensitive and specific in the ambulatory population, in which the finding of a normal TSH level is strong evidence that a patient is euthyroid, and an abnormal TSH has a high likelihood of being due to thyroid dysfunction. However, abnormally high or low TSH values (compared to those of an ambulatory euthyroid control population) are frequently noted in hospitalized patients as a result of the effects of nonthyroid illness, acute psychiatric illness, or glucocorticoid therapy.52,53 Therefore, diagnoses of hypothyroidism or hyperthyroidism in hospitalized patients should be based on clinical evaluation, measurement of free thyroid hormone levels, and other indices of thyroid function, rather than on TSH measurement alone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree