Chondrosarcoma
R. Lor Randall
Kenneth J. Hunt
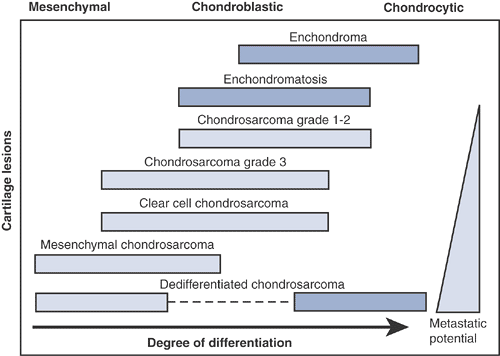
Chondrosarcomas of bone can be found in any bone in the human body and include a spectrum of lesions that range from low grade to dangerously aggressive. Although cartilage bone lesions in general have a characteristic radiographic appearance, differentiating between benign and low-grade malignant cartilage lesions often presents a diagnostic challenge (Table 6.3-1). Since treatment and outcome are based in large part upon an accurate diagnosis, this distinction is important (Fig. 6.3-1).
Pathogenesis
Etiology
Unknown
Current speculation: may arise from monoclonal expansion of single chondrocyte
Epidemiology
Peak age: third to sixth decades (Fig. 6.3-2)
Frequency of chondrosarcomas in the United States
∼10% to 25% of primary bone tumors are chondrosarcomas.
Approximately 250 to 625 cases/year in United States
Second to osteosarcoma among bone sarcomas
Table 6.3-1 Differentiation Between Benign and Low-Grade Malignant Cartilage Lesions | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Pathophysiology
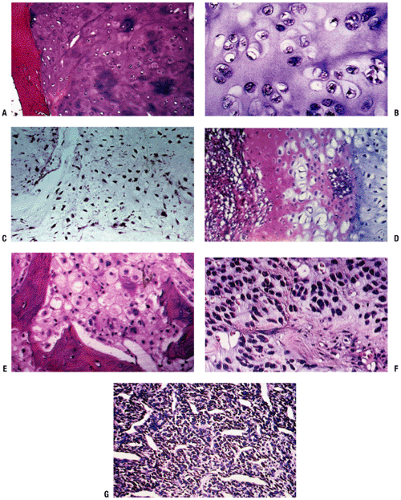
Histopathology (Fig. 6.3-3)
Macroscopic appearance
Heterogeneous gross properties, including lobulated areas of chalky calcific admixture
Regions of firm translucent unmineralized gray cartilage with relatively low vascularity
Intermixed areas of necrosis and degeneration
Low-grade chondrosarcomas
Relatively acellular, heavily calcified areas
Regions of increased activity exhibiting immature cartilage cells with multiple nucleated lacunae
Permeation pattern of cartilage surrounding pre- existing bony trabeculae
High-grade chondrosarcomas
Densely packed, hyperchromatic, malignant-looking cells
May be difficult to determine that these cells are truly of cartilaginous origin
Myxomatous changes and highly degenerative areas common
Classification
Several classification schemes
Histologic grade (I, II, III, dedifferentiated)
The most important factor in the malignant potential of a chondrosarcoma is its histologic grade. Most (∼85%) chondrosarcomas are low-grade lesions.
Location within the bone and body
Peripheral (periosteal or juxtacortical chondrosarcoma and secondary chondrosarcoma arising from osteochondroma) versus central (intramedullary)
Axial versus appendicular skeleton
Primary versus secondary
Primary: arises de novo
Secondary central: arises from enchondroma
Secondary peripheral: arises from osteochondroma
Specific histologic subtype
Conventional
Clear cell chondrosarcoma
Mesenchymal chondrosarcoma
Dedifferentiated chondrosarcoma
Histologic grades of conventional chondrosarcomas (Table 6.3-2)
Grade I (“low-grade”) tumors
Slow-growing and locally aggressive
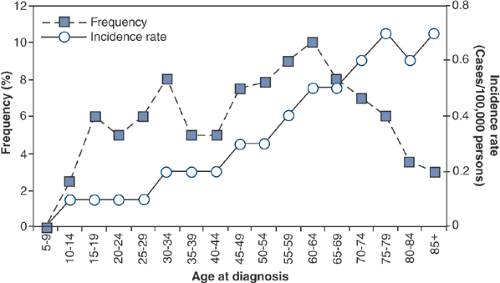
Figure 6.3-2 Age-specific frequency and distribution of chondrosarcoma, based on SEER 1973–1987 data. (After Dorfman HD, Czerniak B. Bone cancers. Cancer 1995;75:223–227.)
Table 6.3-2 Clinicopathologic Features of Cartilaginous Tumors
Lesion
Clinical
Radiology
Histopathology
Treatment
Enchondroma
Mostly asymptomatic and incidentally recognized
9% have endosteal scalloping
Enchondroma encasement pattern
Surveillance, intralesional excision if symptomatic
Chondrosarcoma
Grade I
60% are painful
Endosteal scalloping, calcifications in rings or spicules, uniform calcifications, eccentric lobular growth
Chondrosarcomatous permeative pattern
Controversial: Extended intralesional excision versus wide resection
Grade II
Up to 80% painful
Endosteal scalloping, potentially more aggressive and adaptive changes
Mixture of grade I and grade III characteristics
Wide resection
Grade III
Up to 80% painful
Endosteal scalloping, faint amorphous calcifications, large lucent areas, growing soft tissue mass
Densely packed hyperchromatic malignant-looking cells, cells of questionable cartilaginous origin, myxomatous changes, highly degenerative areas
Wide resection
Possible adjunct radiation therapy and chemotherapy in selected cases
Recurrence common, but very low metastatic potential
Histologically resemble normal hyaline cartilage, may surround or permeate through areas of lamellar bone (a feature not seen in benign lesions, which are more typically encased by bone)
Radiographically may show bone expansion, cortical thinning, endosteal scalloping, periosteal reaction, lytic areas
Grade II (“intermediate-grade”) tumors
Locally aggressive with higher potential for recurrence
∼10% to 15% metastasize (lung > bone)
Histologically show increased cellularity and cytological atypia (enlarged nuclei and often multinucleated cells) with foci of myxoid changes
Radiographically, grade II lesions show endosteal scalloping.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree