, Joong Mo Ahn2 and Yusuhn Kang2
(1)
Department of Radiology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, South Korea
(2)
Department of Radiology, Seoul National University, Bundang Hospital, Seongnam, South Korea
3.1 Osteochondroma
Overview
Osteochondroma is a surface lesion composed of lamellar bone covered by a cartilage cap (Fig. 3.1). Clinically, it presents most commonly as painless swelling and cosmetic deformity. Further clinical presentation may include neurovascular impingement, fracture, overlying bursal or pseudoaneurysm development, and malignant transformation (Fig. 3.2). The younger the patient, the closer the lesion will be to the growth plate. Osteochondroma ceases to grow by the time the physis closes, and the cartilage cap usually involutes after skeletal maturity. This lesion is usually classified as a neoplasm, but it is generally believed that it occurs as a result of physeal cartilage displacement onto the bone surface. If the lesion is asymptomatic, it can be followed radiographically and clinically until cessation of growth.
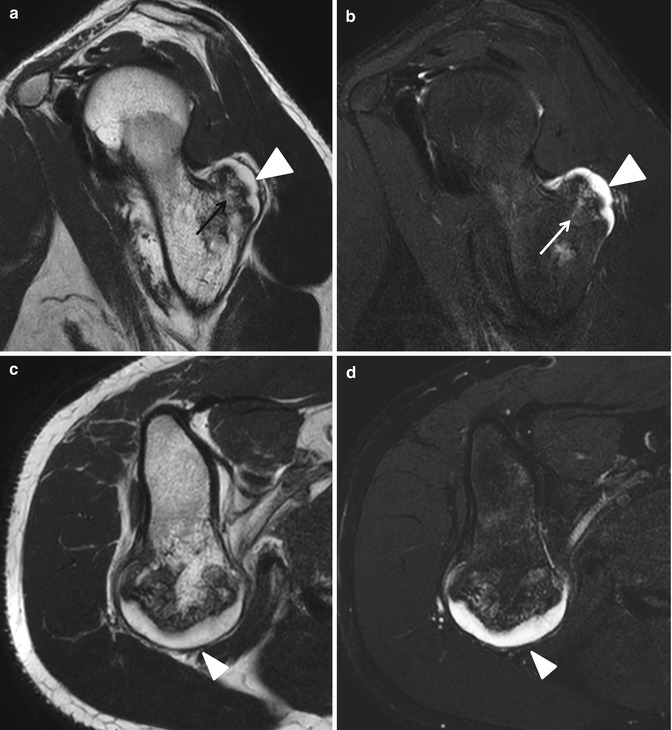
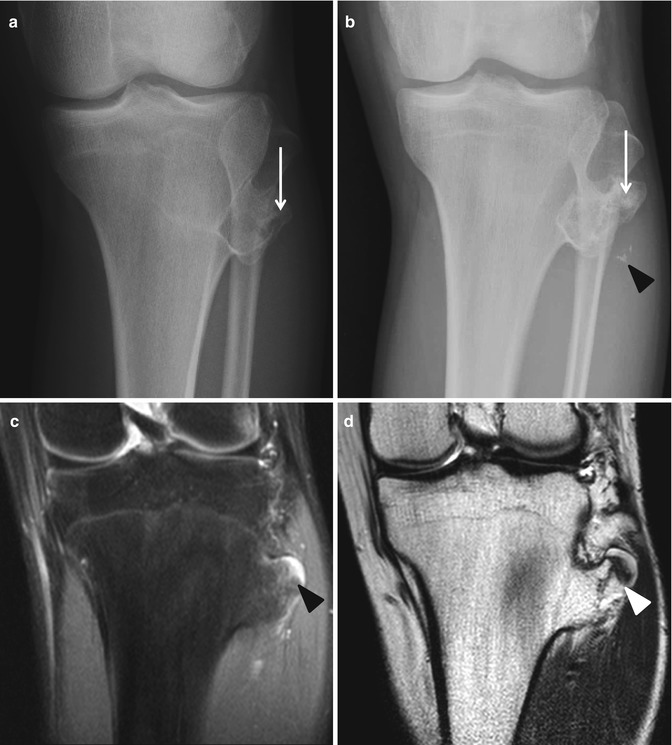
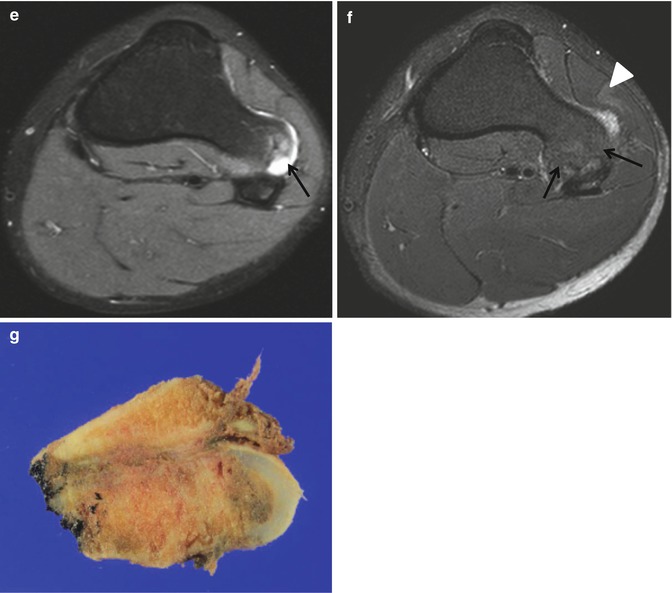
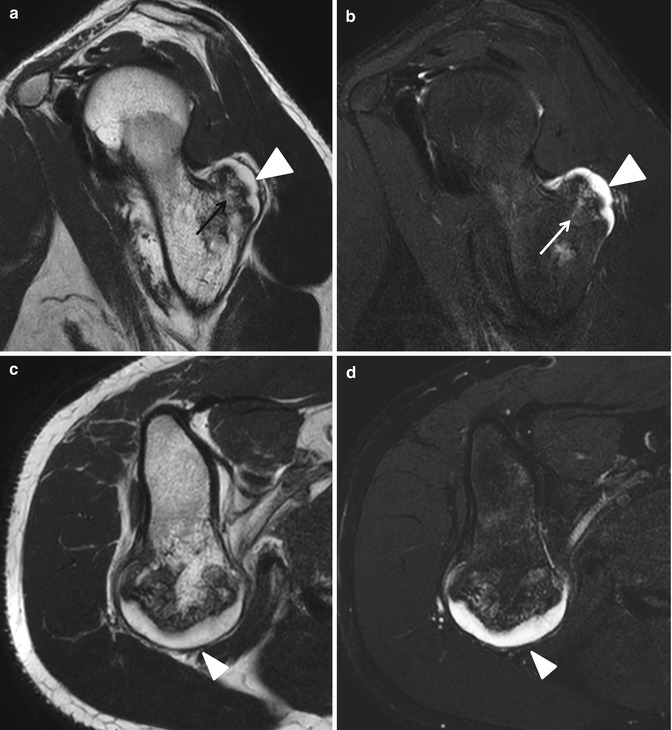
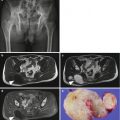
Fig. 3.1
Osteochondroma. (a) Sagittal T2-weighted MR image shows a surface lesion composed of lamellar bone (arrow) covered by a cartilage cap (arrowhead). (b) Sagittal fat-suppressed T2-weighted MR image demonstrates a surface lesion composed of lamellar bone (arrow) covered by a cartilage cap (arrowhead). (c) Axial T2-weighted MR image shows an osteochondroma with hyperintense cartilage cap (arrowhead). (d) Axial fat-suppressed T2-weighted MR image demonstrates an osteochondroma with hyperintense cartilage cap (arrowhead)
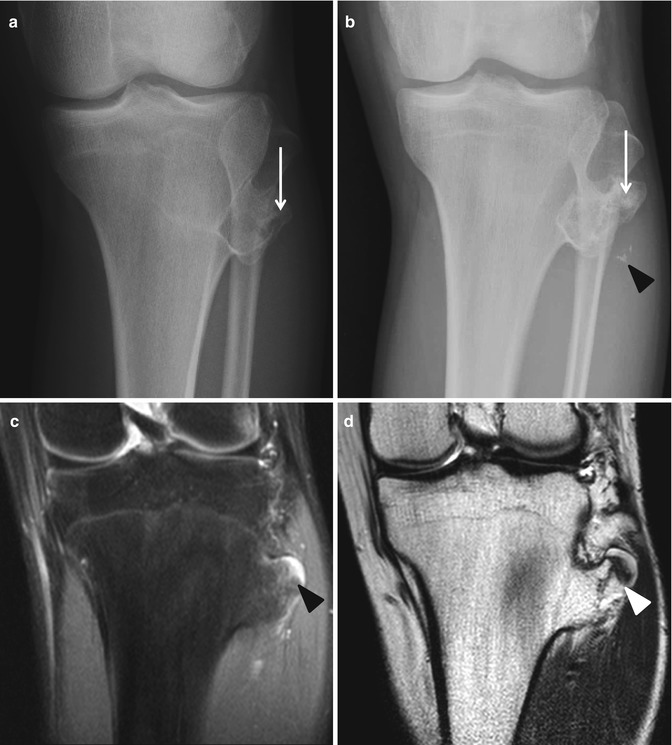
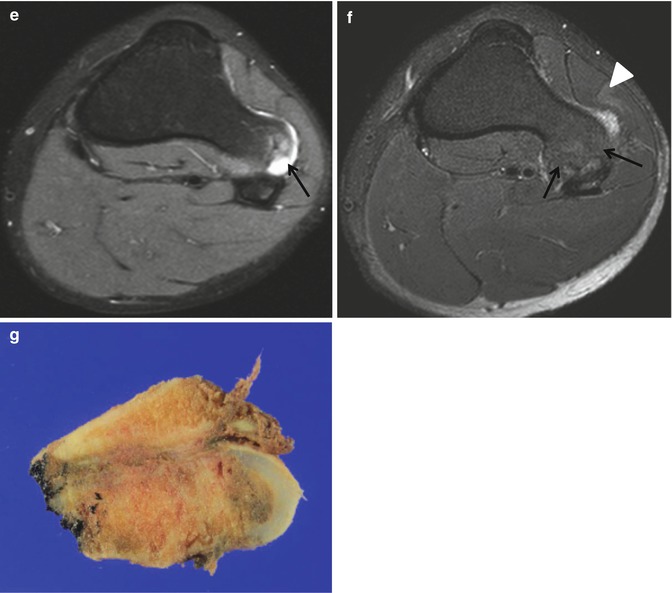
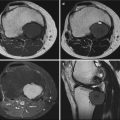
Fig. 3.2
Malignant transformation of osteochondroma. (a) Anteroposterior radiograph of the left knee shows a pedunculated bony protrusion (arrow) arising from the left proximal tibia, representing an osteochondroma. (b) Four-year follow-up anteroposterior radiograph shows slightly increased size of the osseous protrusion (arrow) with adjacent soft tissue mineralization (arrowhead). (c) Coronal fat-suppressed proton density-weighted MR image shows an osseous protrusion with hyperintense cartilage cap (arrowhead). (d) Coronal T2-weighted MR image again demonstrates an osseous protrusion with hyperintense cartilage cap (arrowhead). (e) Axial fat-suppressed proton density-weighted MR image shows an osseous protrusion with hyperintense cartilage cap (arrowhead). (f) Axial T2-weighted fat-suppressed MR image shows an osseous protrusion with hyperintense cartilage cap (arrowhead). (g) Corresponding gross photograph shows an osseous mass with thick cartilage cap. Histopathology showed a chondrosarcoma, grade 1
A benign osteochondroma may become painful for a number of reasons, including fracture through the stalk, development of an overlying bursa, or compression of adjacent neurovascular bundle.
Epidemiology
Osteochondroma is the most common benign bone tumor. There is a male predominance, and 75 % of patients are younger than 20 years of age.
Common Locations
Osteochondroma can arise from any bone undergoing enchondral maturation, but it is most common in tubular bones and in particular around the knee. The ilium and scapula are the two most commonly affected flat bones. In long bones, it is located at the metaphysis and grows away from the joint.
Imaging Features
Radiograph
Osteochondroma is a surface lesion that demonstrates corticomedullary continuity (Fig. 3.3). It may be on a stalk (pedunculated) (Fig. 3.4) or broad based (sessile) (Fig. 3.5). The osteochondroma can usually be diagnosed with radiography alone.
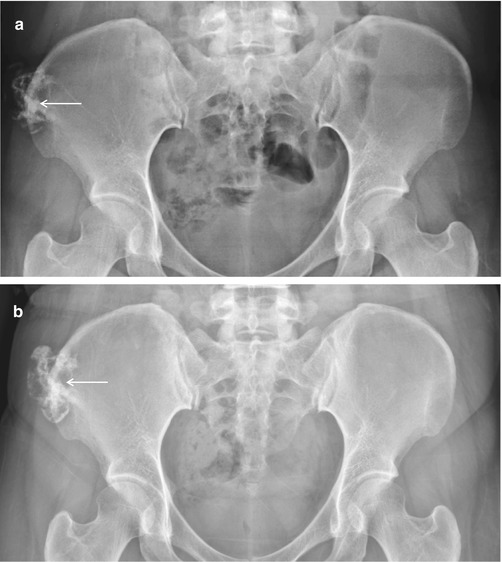
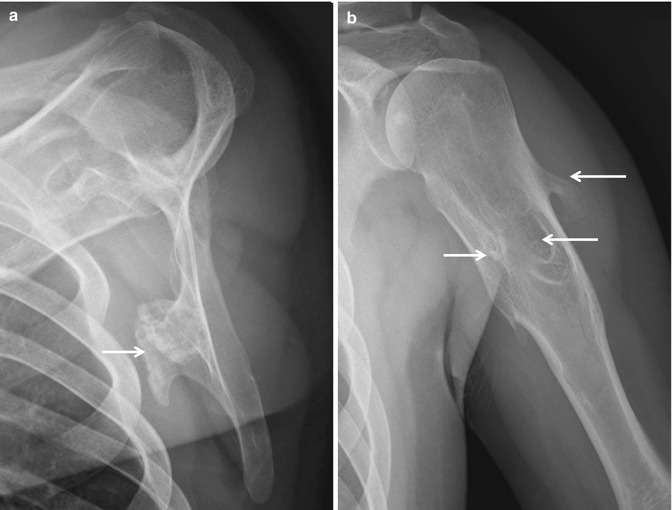
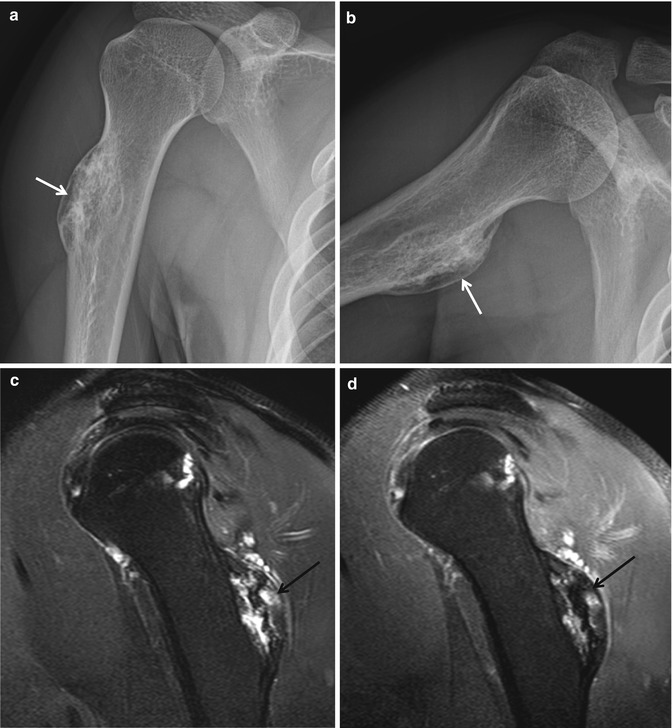
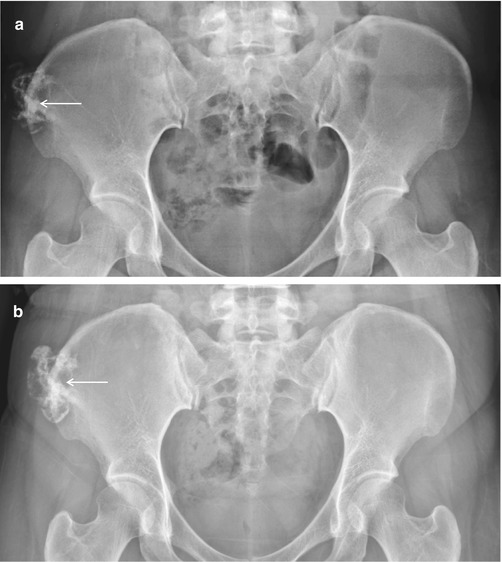
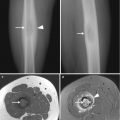
Fig. 3.3
Osteochondroma. (a) Anteroposterior radiograph of the pelvis shows a pedunculated osseous mass (arrow) with corticomedullary continuity, arising from the right ilium. (b) Four-year follow-up anteroposterior radiograph of the pelvis shows slightly increased size of the osteochondroma (arrow). Surgical resection was performed, and histopathology showed features of an osteochondroma without evidence of malignant transformation
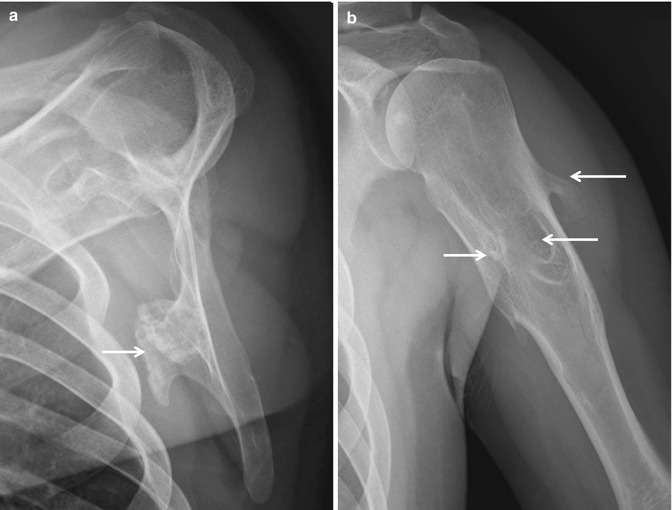
Fig. 3.4
Osteochondroma. (a) Lateral radiograph of the left scapula shows a pedunculated osseous mass (arrow) with corticomedullary continuity, representing osteochondroma. (b) Lateral radiograph of the left humerus demonstrates multiple osteochondromas (arrows). The osteochondromas point toward the diaphysis
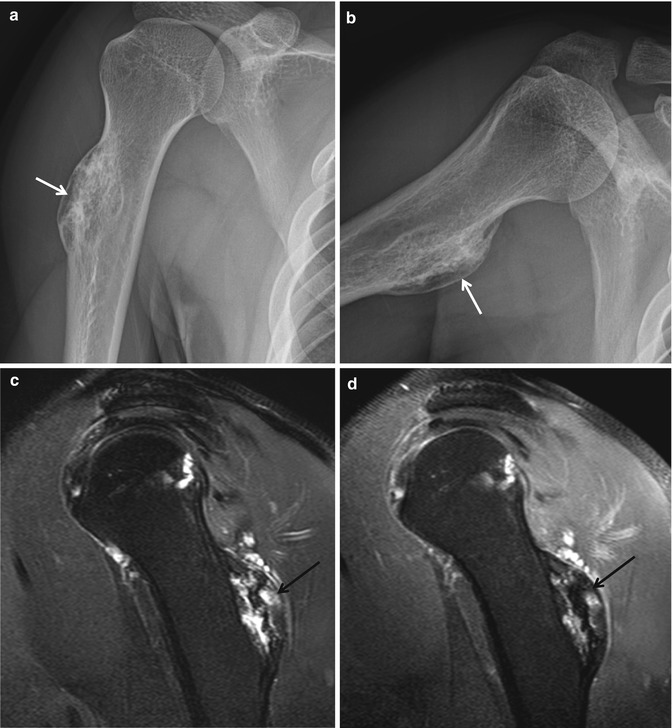
Fig. 3.5
Osteochondroma. (a) Anteroposterior radiograph of the right humerus shows sessile osteochondroma (arrow). (b) Lateral radiograph of the right humerus again shows sessile osteochondroma (arrow). (c) Sagittal T2-weighted fat-suppressed MR image shows a broad-based osseous protrusion (arrow) with hyperintense areas. (d) Sagittal fat-suppressed contrast-enhanced T1-weighted MR image shows a broad-based osseous protrusion (arrow) with areas of nodular enhancement
Magnetic resonance imaging
MR imaging may demonstrate a cartilage cap. After skeletal maturity, the cartilage cap should not be thicker than 2 cm; if it is, then transformation to chondrosarcoma should be considered. MR imaging aids in distinguishing bursa formation over the cap from the actual cap. Cartilage cap growth after skeletal maturity and pain are worrisome for malignant transformation.
Differential Diagnoses
- 1.
Parosteal osteosarcoma
Osteochondromatous lesions in the popliteal fossa should be differentiated from parosteal osteosarcoma. Round-shaped parosteal osteosarcoma may mimic a densely calcified osteochondroma.
- 2.
Osteoma
Osteoma is a small, round, well-defined, homogeneous, bony surface lesion arising from the cortex and does not demonstrate the corticomedullary continuity seen in an osteochondroma.
3.2 Enchondroma
Overview
Enchondroma is a benign cartilaginous tumor and is usually discovered either incidentally in long bones or when a pathological fracture occurs. Histologically, it is characterized by rests of hyaline cartilage within the medullary bone intermixed at times with a myxoid matrix.
Enchondroma may have a variable degree of amorphous matrix mineralization. These lesions may undergo a chondrosarcomatous transformation, presenting with a more destructive lytic lesion with a soft tissue mass. Multiple enchondromas can be seen in various syndromes. Ollier disease refers to multiple enchondromas in the appendicular skeleton, particularly the hands. Multiple hemangiomas and enchondromas are present in Maffucci syndrome. Both of these syndromes are associated with an increased rate of malignant transformation of enchondromas.
Epidemiology
Enchondroma is the second most common benign neoplasm of the bone and comprises 3–5 % of biopsied primary bone lesions. Enchondroma is encountered equally in men and women and has a peak incidence in the third decade.
Common Locations
It is common in the bones of the hand and feet and in long bones. Enchondroma occurs mostly as a central lesion in the metaphysis.
Imaging Features
Radiograph
Enchondroma appears as a well-marginated expansile lucent lesion (Fig. 3.6) arising in the medullary cavity, usually near the epiphysis. Chondroid mineralization (Fig. 3.7), including stippling, rings, and arcs calcification, develops in the matrix. Enchondroma is included in the differential diagnosis of lucent lesions, because it lacks matrix mineralization in the hands, where it most commonly occurs. The hand lesions are usually centrally located and can be expansile with associated cortical thickening and endosteal scalloping. This may lead to pathological fracture with minimal trauma. Enchondromas outside of the hands and feet often have a different, distinctive radiographic appearance because of the calcified chondroid matrix.

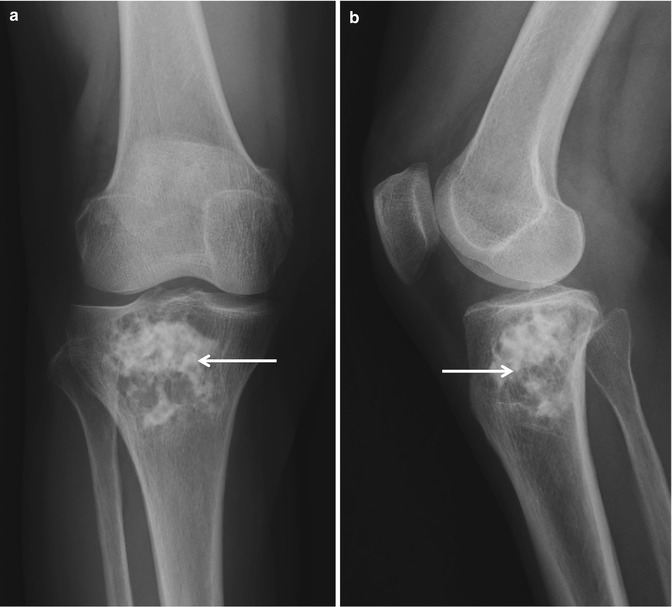
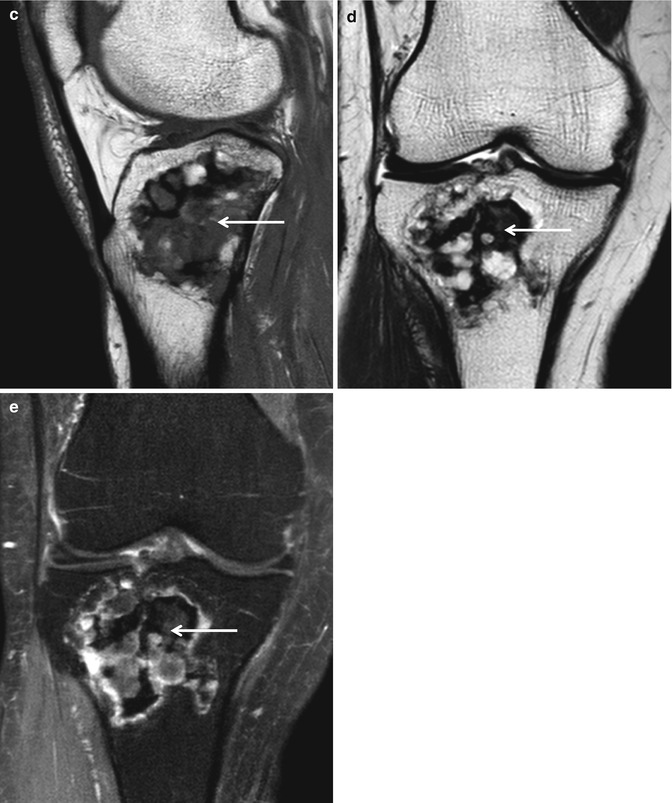

Fig. 3.6
Enchondroma. (a) Posteroanterior radiograph of the right hand shows a lucent lesion with chondroid mineralization (arrow) in the proximal phalanx of the right third finger. (b) Oblique radiograph again demonstrates an intramedullary lesion with chondroid mineralization (arrow)
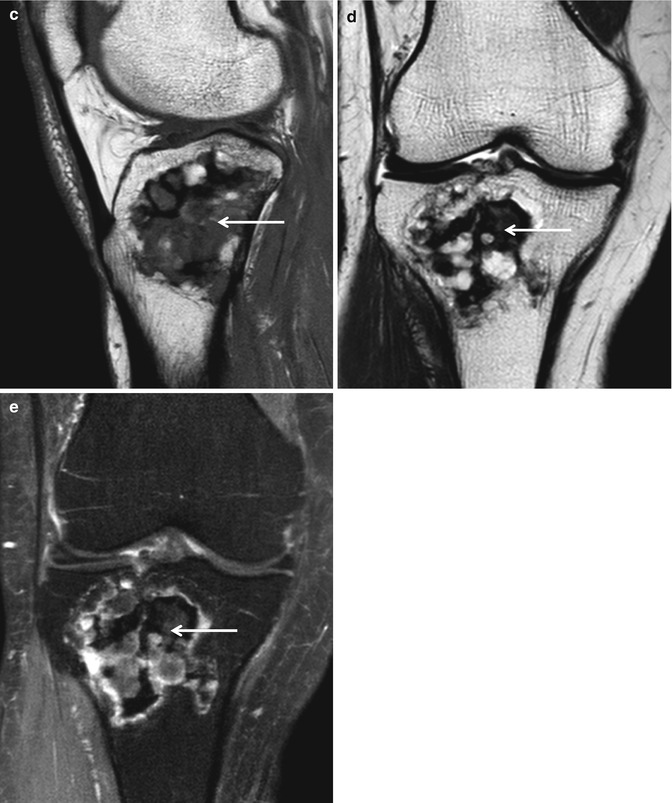
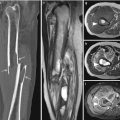
Fig. 3.7
Enchondroma. (a) Anteroposterior radiograph of the right knee shows a lucent lesion with stippled and flocculent mineralization (arrow) in the proximal tibia. (b) Lateral radiograph again demonstrates an intramedullary lesion with chondroid mineralization (arrow). (c) Sagittal T1-weighted MR image shows an intramedullary lesion with hypointense foci (arrow). (d) Coronal T2-weighted MR image again shows an intramedullary lesion with hypointense foci (arrow). (e) Coronal fat-suppressed contrast-enhanced T1-weighted MR image shows peripheral and nodular enhancement and persistent hypointense foci (arrow)
Magnetic resonance imaging
MR imaging can show typical lobular morphology and high signal intensity of the hyaline cartilage within the lesion on the fluid-sensitive sequences and scattered low signal intensity of chondroid mineralization (Fig. 3.7). Rings and arcs pattern of enhancement represents the fibrovascular septae between the cartilage lobules.
Differential Diagnoses
- 1.
Bone infarct
Unlike enchondroma, bone infarct has a well-defined shell-like peripheral sclerosis and does not show endosteal scalloping.
- 2.
Chondrosarcoma
Enchondromas are rare in the axial skeleton, talus, and calcaneus, whereas chondrosarcomas are rare in the short tubular bones. Large size, lesser extent of matrix mineralization within the lesion, greater depth and extent of endosteal scalloping, cortical penetration, periosteal reaction, cortical remodeling, soft tissue extension, and high uptake on bone scan can be suggestive of a chondrosarcoma.
- 3.
Intraosseous ganglion
An intraosseous ganglion appears radiographically as a well-defined lucency with a sclerotic margin adjacent to the articular surface. It most commonly involves the proximal tibia, proximal femur, and the medial malleolus.
- 4.
Skeletal sarcoidosis
Perivascular granulomatous infiltration of sarcoidosis in the Haversian canals of bone may destroy the fine trabeculae and produce a mottled or lacelike coarsely trabeculated pattern. This appears as single or multiple sharply circumscribed, punched-out areas of lucency, primarily involving the small bones of the hands and feet. There may be cortical thinning, expansion, or destruction.
3.3 Periosteal Chondroma (Juxtacortical Chondroma)
Overview
Periosteal or juxtacortical chondroma represents the surface variant of an enchondroma and believed to originate from the periosteum. Periosteal or juxtacortical chondroma presents as focal swelling. Histologically, periosteal chondroma demonstrates lobules of hyaline cartilage limited to the cortex and beneath the periosteum without an extension into the medullary cavity. It grows slowly and ranges from 1 cm to 7 cm in size at presentation. Periosteal chondroma is usually a solitary lesion. Patients with more than one periosteal chondroma should be suspected of having Ollier disease.
Epidemiology
Periosteal chondroma is a lesion of children and young adults, and most patients are in their second through fourth decades of life. It is more prevalent among males.
Common Locations
Periosteal chondroma occurs in the surface of tubular bones, characteristically in the metaphysis. It is most common in the proximal humerus followed by the femur, tibia, short tubular bones of the hands and feet. Pelvis and ribs are uncommon sites.
Imaging Features
Radiograph
Periosteal chondromas present as lesions scalloping the cortex from the periosteal side and eventually forming a sclerotic rim separating them from the medullary cavity of the parent bone (Fig. 3.8). Saucerization or a well-defined depression of the adjacent cortex with a soft tissue mass can be seen. The lesion is sharply circumscribed by a solid buttress of reactive bone or overhanging cortical edges which may entirely cover the lesion. Periosteal chondromas may be purely lytic or may show internal chondroid mineralization.

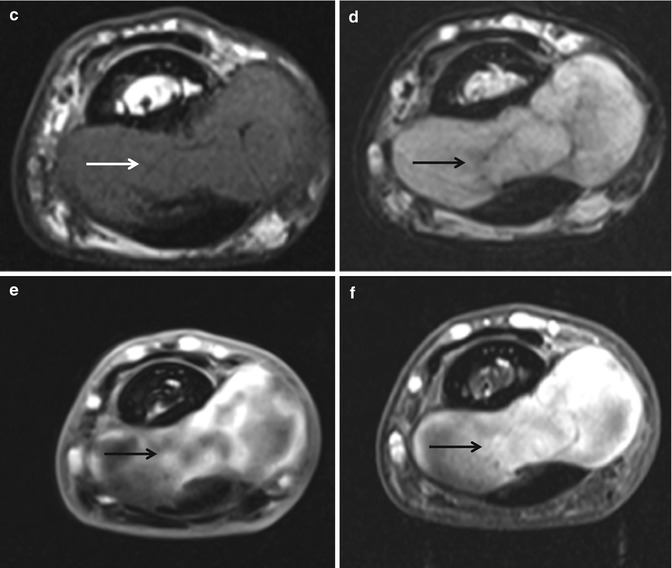
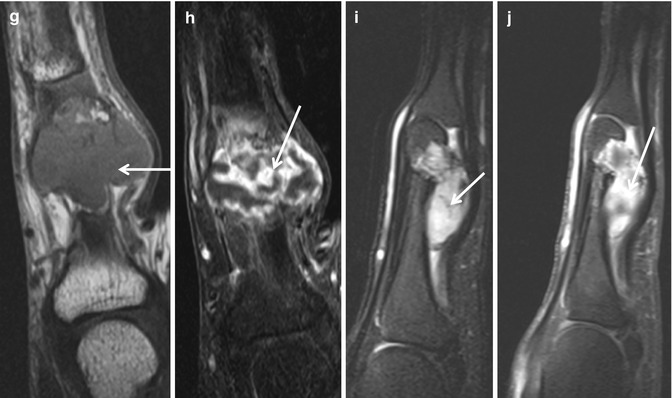

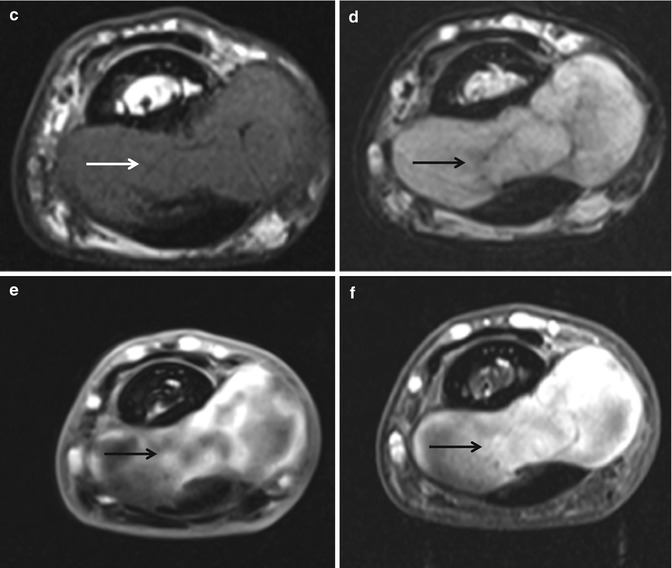
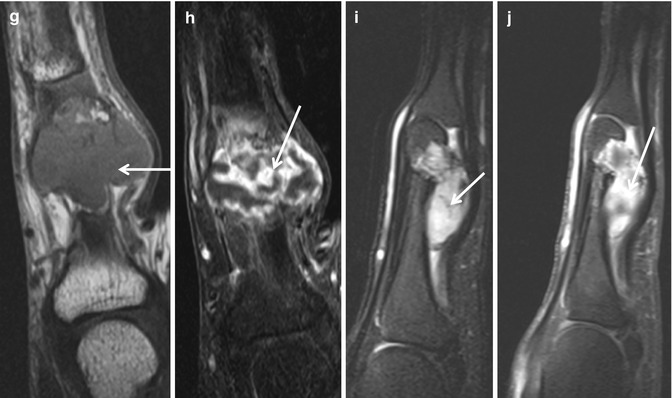
Fig. 3.8
Periosteal chondroma. (a) Anteroposterior radiograph of the right fifth finger shows a well-defined osteolytic lesion (arrow) in the proximal phalanx with adjacent soft tissue mass (arrowhead). (b) Lateral radiograph demonstrates a saucerization of the volar cortex and a soft tissue mineralization (arrow). (c) Axial T1-weighted MR image shows a cortical-based periosteal mass that has intermediate signal intensity (arrow). (d) Axial T1-weighted MR image shows a cortical-based periosteal mass with increased signal intensity (arrow). (e) Axial fat-suppressed contrast-enhanced T1-weighted MR image demonstrates a cortical-based periosteal mass that shows heterogeneous enhancement (arrow). (f) Additional axial fat-suppressed contrast-enhanced T1-weighted MR image demonstrates a cortical-based periosteal mass that shows heterogeneous enhancement (arrow). (g) Coronal T1-weighted MR image shows a lobulated mass with intermediate signal intensity (arrow). (h) Coronal fat-suppressed contrast-enhanced T1-weighted MR image demonstrates a lobulated mass with peripheral enhancement (arrow). (i) Sagittal fat-suppressed contrast-enhanced T1-weighted MR image demonstrates a juxtacortical mass with heterogeneous enhancement (arrow). (j) Additional sagittal fat-suppressed contrast-enhanced T1-weighted MR image demonstrates a juxtacortical mass with heterogeneous enhancement (arrow)
Magnetic resonance imaging
Periosteal chondroma is typically multilobulated and shows a low signal intensity rim on MR imaging. MR imaging shows the high water content of the cartilage tissue (Fig. 3.8). Peritumoral edema is typically absent. Administration of contrast depicts peripheral enhancement. MR imaging also confirms the lack of communication of this lesion with the medullary canal.
Differential Diagnoses
- 1.
Periosteal chondrosarcoma
Periosteal chondrosarcoma usually presents later in life and demonstrates invasion of the medullary cavity and peritumoral edema. Periosteal chondrosarcomas are generally larger (>3 cm), may contain hazy windblown densities, and do not show an endosteal border of sclerosis.
- 2.
Juxtacortical osteosarcoma
Juxtacortical osteosarcoma is usually more aggressive, frequently with a pattern resembling a sunburst-type periosteal reaction, and may have an osteogenic matrix.
- 3.
Chondromyxoid fibroma
Chondromyxoid fibroma generally appears as an eccentric expansile metaphyseal osteolytic lesion with cortical expansion, coarse trabeculation, endosteal scalloping, and scalloped sclerotic medullary border.
- 4.
Aneurysmal bone cyst
Surface aneurysmal bone cysts show predominantly extraosseous extension with varying amounts of preservation of the inner cortex. Typically, a thin layer of inner cortex remains, and the lesion is surrounded by a radiographically visible shell of periosteal new bone.
3.4 Chondromyxoid Fibroma
Overview
Chondromyxoid fibroma is composed of varying degrees of cartilaginous, fibrous, and myxoid components. It presents with swelling and may occasionally be painful.
Epidemiology
Chondromyxoid fibroma is the least common benign tumor of chondroid origin and <1 % of primary bone tumors. It has a slight male predilection. Most cases occur younger than age of 30, although it affects a wide range of age between 3 and 70 years.
Common Locations
It arises most often around the knee, with the proximal tibia as the single most common location. The foot and pelvic bones also are common sites. Chondromyxoid fibroma is usually located in the metaphysis of the long bones as an eccentric lesion, and it is often cortical.
Imaging Features
Radiograph
Chondromyxoid fibroma generally appears as an eccentric expansile metaphyseal osteolytic lesion with cortical expansion, coarse trabeculation, endosteal scalloping, and scalloped sclerotic medullary border on radiographs (Fig. 3.9). Calcification is infrequent, unlike chondroblastoma and other cartilaginous lesions. Inner narrow zone of transition with the adjacent normal bone and a thinned or absent outer margin may simulate a more aggressive lesion. Larger lesion may show destruction of the cortex resulting in a hemispherical osseous defect or “bite” without periosteal reaction. In the foot and flat bones, it presents as a central expansile lesion.
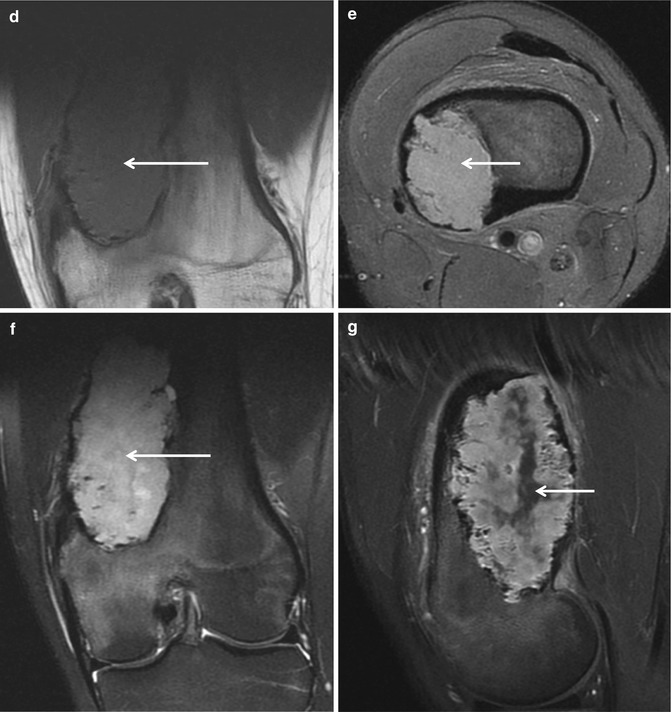
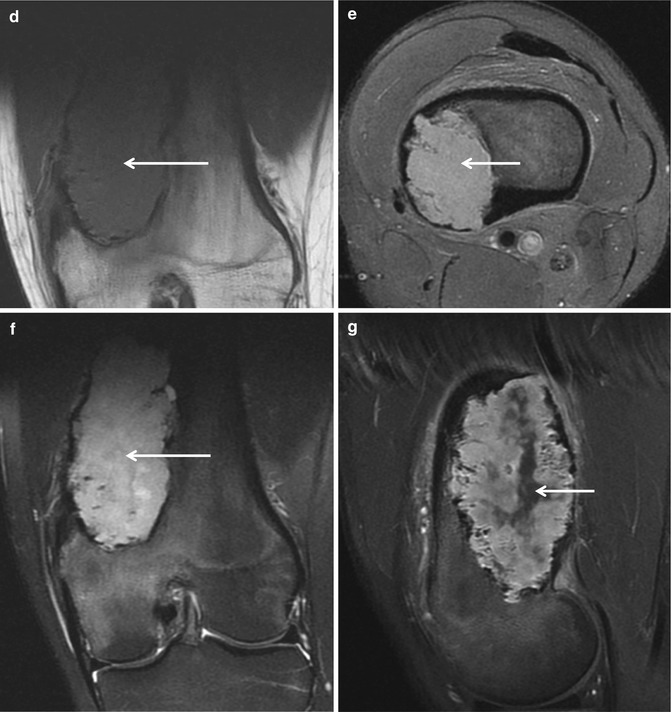
Fig. 3.9
Chondromyxoid fibroma. (a) Anteroposterior radiograph of the left knee shows an eccentric expansile metaphyseal osteolytic lesion with cortical expansion, coarse trabeculation, endosteal scalloping, and scalloped sclerotic medullary border. (b) Lateral radiograph of the left knee demonstrates an expansile osteolytic lesion with cortical expansion and endosteal scalloping. (c) Bone scan shows an increased uptake (arrow) with photon defect in the central portion in the left distal femur. (d) Coronal T1-weighted MR image demonstrates a lobulated mass with intermediate signal intensity (arrow). (e) Axial fat-suppressed proton density-weighted MR image demonstrates a lobulated mass with increased signal intensity (arrow). (f) Coronal fat-suppressed T2-weighted MR image demonstrates a lobulated mass with high signal intensity (arrow). (g) Sagittal fat-suppressed contrast-enhanced T1-weighted MR image demonstrates a lobulated enhancing mass with central nonenhancing component (arrow)
Magnetic resonance imaging
MR imaging may demonstrate a lobulated margin. The MR signal intensity of this lesion is variable (Fig. 3.9).
Differential Diagnoses
- 1.
Periosteal chondroma
Periosteal chondroma may be purely lytic or may show internal chondroid mineralization, saucerization, or a well-defined depression of the adjacent cortex with a soft tissue mass.
- 2.
Aneurysmal bone cyst
Aneurysmal bone cyst can be found in the metaphysis or diaphysis of long bone and show morphological signs of slow growth. Matrix calcifications detected radiographically or by CT exclude this entity. MR imaging is able to differentiate a solid lesion like chondromyxoid fibroma from cystic lesions.
- 3.
Giant cell tumor
Giant cell tumor is more likely than chondromyxoid fibroma to reach the subchondral bone in the epiphysis, and more frequently penetrates the cortex without neocortex formation.
- 4.
Enchondroma in the short bones
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree