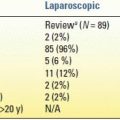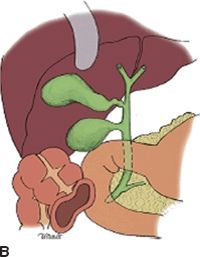
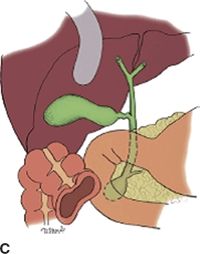


FIGURE 26.1 Classification of biliary cysts. A. Type I. B. Type II. C. Type III. D. Type IV. E. Type V. (From Lipsett PA, Pitt HA, Colombani PM, et al. Choledochal disease: a changing pattern of presentation. Ann Surg 1994;220(5):644.)
Type I cyst is a dilation of the common hepatic duct and represents 50% to 80% of all cysts. Type 1 CC is subclassified into three types based on shape: type Ia cystic, type Ib focal, and type Ic fusiform.
Type II cyst is a supraduodenal diverticulum of the extrahepatic duct to which it is connected with a narrow stalk. It represents only 2% to 3% of all cysts.
Type III cyst, also known as choledochocele, is a dilation of the common bile duct confined to the wall of the duodenum. Type III CC represents less than 10% of all cysts.
Type IV cyst refers to multiple cystic dilations of the biliary tract and is further subclassified into type IVa where multiple cysts are present in the intrahepatic and extrahepatic bile ducts and type IVb where multiple cysts only involve the extrahepatic bile duct. Type IVa cyst is the second most common type of CC representing 30% to 40%, while type IVb only accounts for less than 5% of all cysts.
Type V cyst (Caroli disease) involves only the intrahepatic biliary ducts and can be unilobar or bilobar. It represents less than 10% of all CCs.
DIAGNOSIS
Presentation
The historically described pathognomonic triad of abdominal pain, jaundice, and right upper quadrant palpable mass is only present in 10% to 17% of children. However, 85% of children present with at least two symptoms of the triad compared to only 25% of adults.
Vague right upper quadrant abdominal pain associated with nausea and emesis is often the presenting symptom in adults. Laboratory evaluation of liver function and pancreatic enzymes frequently reflects common conditions such as cholangitis or pancreatitis, where concurrent pancreatitis may be present in 30% to 70% of adult patients. Additionally, concurrent cystolithiasis and cholecystolithiasis are present in approximately 70% of patients. As a result, an interval of up to 6 years from the first presenting symptoms to the diagnosis of cystic disorder of the biliary ducts is relatively common. This delay in diagnosis often leads to additional procedures such as cholecystectomy or other surgical exploration. Most often, adults are diagnosed with CC during evaluation and treatment of complications such as cholecystitis or acute pancreatitis. Diagnosis may also be discovered incidentally during radiologic investigation for other problems. In contrast to other cyst types, patients with type III choledochal cyst (choledochocele) commonly present with acute pancreatitis.
Although rare, hepaticolithiasis and intrahepatic abscess have been described as presenting complications of type IV and V bile duct cysts. This can eventually lead to secondary biliary cirrhosis and portal hypertension with subsequent liver failure.
Cyst rupture and biliary peritonitis have been also described as presenting symptoms but usually in children. These situations are extraordinarily rare.
The most common malignancy associated with CC disease is cholangiocarcinoma, though the presence of CC also increases the risk of developing gallbladder cancer.
Imaging
Demonstration of the continuity of the cystic lesion with the biliary duct is paramount in distinguishing it from other intra-abdominal cysts such as pancreatic pseudocyst, biliary cystadenoma, or echinococcal cysts. In patients with equivocal bile duct dilation (i.e., 1 to 2 cm), the presence of APBDJ strongly suggests the diagnosis of CC.
Abdominal ultrasound (US) is often the primary and the most cost-effective imaging modality in diagnosing bile duct cyst; the sensitivity of US ranges from 71% to 97%.
Endoscopic ultrasound has been described in the literature in order to overcome the intrinsic limitations of transabdominal US such as body habitus, bowel gas, the presence of overlying intra-abdominal structures, and poor visualization of distal bile duct. It also gives you information of the pancreas and biliary duct anatomy.
Computed tomography (CT) scan is now widely available and presents several advantages in the diagnosis of CC. Some of these advantages include characterization of intrahepatic bile ducts, dilation evaluating the cysts surrounding structures, and more visualization of the distal bile duct and the pancreatic head. It also allows for evaluation of malignancy that may mimic CC or may be originating from a CC. (i.e., very thick cyst wall or portal lymphadenopathy).
Computed tomography cholangiography (CTCP) though not widely available currently has 90% sensitivity for diagnosis of CC and can correctly visualize the bile duct anatomy prior to a surgical procedure.
Magnetic resonance cholangiography (MRCP) is becoming the gold standard in diagnosis with a reported sensitivity ranging between 90% and 100%. Though MRI/MRCP is relatively more expensive than CT, MRCP offers similar excellent cross-sectional imaging evaluation as well as superior visualization of the entire biliary tree (including APBDJ).
Particularly challenging in children is proper distinction between biliary atresia and bile duct cyst. In this situation, a 99technetium HIDA scan will demonstrate continuity of the cystic lesion with the bile duct and eventually emptying of contrast into the bowel. Retention of contrast in the biliary system is typical of biliary atresia or any condition causing distal common bile duct (CBD) obstruction. The sensitivity of a hepatobiliary iminodiacetic acid (HIDA) scan, however, is subject to wide variation ranging from 100% for type I to only 67% for type IVa. This inaccuracy is mainly due to HIDA inability to visualize the intrahepatic bile ducts.
In light of the increased accuracy of MRCP and CTCP, invasive cholangiography modalities such as percutaneous transhepatic cholangiogram (PTC) and endoscopic retrograde cholangiopancreatography are applied less frequently. However, in the scenario where biliary drainage is inadequate (type IV/V), PTC and stent placement may be required.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree