Abstract
Solid tumors in neonates can arise anywhere in the body and present unique challenges to clinicians. Benign tumors are most common [1], and are typically less amenable to chemotherapy or radiation and more in need of surgical approaches. Radiation’s role in childhood cancer is diminishing as better chemotherapeutic approaches are developed and its use in neonates is rare due to its devastating long-term toxicity. Finally, differences in neonatal physiology imparts a variable upon chemotherapy pharmacokinetics that is difficult to fully control and frequently results in greater toxicity. These factors, combined with the biology of the tumors uniquely seen in the neonate, worsen the survival for neonates with cancer. This chapter acquaints the clinician with the array of tumors most commonly found in the infant <28 days of age (Table 22.1).
Introduction
Solid tumors in neonates can arise anywhere in the body and present unique challenges to clinicians. Benign tumors are most common [1], and are typically less amenable to chemotherapy or radiation and more in need of surgical approaches. Radiation’s role in childhood cancer is diminishing as better chemotherapeutic approaches are developed and its use in neonates is rare due to its devastating long-term toxicity. Finally, differences in neonatal physiology imparts a variable upon chemotherapy pharmacokinetics that is difficult to fully control and frequently results in greater toxicity. These factors, combined with the biology of the tumors uniquely seen in the neonate, worsen the survival for neonates with cancer. This chapter acquaints the clinician with the array of tumors most commonly found in the infant <28 days of age (Table 22.1).
| Brain tumors | Cardiac tumors | Pulmonary/thoracic tumors |
|
|
|
|
|
|
Epidemiology
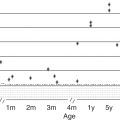
Fortunately, tumors in newborns are rare. Among infants less than 1 year of age, 13% of malignancies are diagnosed in the first month of life with an incidence of 30–36 cases per million neonates [2, 3], which is significantly less than the overall 233 cases per million children <1 year of age [2]. The distribution of tumors seen in neonates is quite different than seen in older children (Table 22.2). Solid tumors outside the central nervous system (CNS) make up the majority of neonatal tumors [4, 5], and quite the opposite distribution is seen in older children [6]. Other entities found in infants typically not included in the tumor registries include vascular tumors and histiocytic disorders and these are briefly discussed in this chapter. Overall survival (OS) is worse in neonates either due to inability to give optimal therapies, differences in tumor biology or potentially due to decisions to forgo therapy when chance of cure or good quality of life is perceived as low by family and/or providers. Recent SEER analyses found a 5 year OS of 60.3% (95% CI, 56.2%–64.4%) with the highest survival seen in those with solid tumors (71.2%) versus leukemias (39.1%), and CNS tumors (15%)[4], and all significantly worse than in children ages 1–14 years whose 5 year OS is 80.6% [7]. Some exceptions exist, e.g., infants with neuroblastoma whose tumors are significantly less likely to contain the adverse MYCN oncogene and which frequently have the unique characteristic of spontaneous regression not seen in older children.
| Source | ||||||
|---|---|---|---|---|---|---|
| Alfaar et al. [4]SEER (1973–2007) | Parkes et al. [5]Midlands, UK (1960–1989) | Desandes et al. [3]France (2000–2009) | Rao et al. [1] Glasgow (1955–1999) | Total (solid tumors) | Ries et al. [6]SEER (1975–1995)** | |
| Age group | <1 month | <1 month | <28 days | <28 days | <1 month | <15 yrs |
| Total (N) | 615 | 99 | 285 | 83 | 19,845 | |
| Solid tumors – N (% of all tumors) |
|
| 256 | 83 | 879 | (51.7%) |
| % of non-CNS solid tumors | ||||||
| Peripheral nerve tumors (including neuroblastoma) | 38% | 17% | 52% | 17% | 38% | 21% |
| Germ cell (including teratomas) | 37% | 53%* | 32% | 40% | 37% | 10%** |
| Soft tissue | 11% | 9% | 9% | 16% | 11% | 27%*** |
| Renal tumors | 4% | 8% | 2% | 16% | 5% | 17% |
| Retinal tumors | 6% | 2% | 3% | – | 4% | 8% |
| Hepatic tumors | 2% | 7% | 1% | 5% | 2% | 4% |
| Other | 2% | 2% | – | 7% | 2% | 10% |
| CNS tumors – N (% of all tumors) |
|
| 29 | – | – | (20.2%)**** |
| Leukemias/lymphomas − N (% of all tumors) |
|
| N/A | – | – | (42.2%) |
| Lymphoid | (3.6%) | (24.7%) | ||||
| Myeloid | (7.3%) | (6.8%) | ||||
| Unspecified or lymphoreticular | (4.2%) | (10.7%) | ||||
Notes: * These were all reported as teratomas
** Does not include borderline malignancies such as teratomas
*** Includes both soft tissue (7%) and bone (4.5%) sarcomas
**** Does not include benign/low grade brain tumors
When encountering a neonatal solid tumor one must consider the possibility of a genetic predisposition and certainly the family will want information regarding this potential association. In a large pediatric series 8.5% of pediatric cancer cases were associated with a germline mutation in a cancer predisposition gene [8]. As techniques and genetic data improve, we may find a higher association. The most important first step is obtaining a detailed family history followed by full assessment of any additional clinical features pointing toward an associated syndrome. Screening tools are available to help determine the need for further work-up and referral to genetics [9].
Peripheral Nerve Tumors and Adrenal Masses
Neuroblastoma, the most common extracranial malignant tumor in infants, has an incidence in the neonatal period of 17–19.7 per million live births [10–12]. The true incidence may be vastly underestimated as a number of infants are never symptomatic and tumors spontaneously regress as shown in past newborn screening studies [13, 14]. Neuroblastomas and their more benign histologic variants, ganglioneuroblastoma and ganglioneuroma, originate from neural crest cells and most commonly arise in the adrenal glands but may present anywhere along the sympathetic chain. Infants frequently present with abdominal distention due to a mass but clinical presentation varies depending upon tumor location. Some may present with Horner syndrome or paralysis due to compression of neurovascular structures, with hepatomegaly due to metastatic disease or with respiratory distress related to a posterior mediastinal tumor. Metastatic lesions, such as a blueberry muffin rash, periorbital and other bone lesions, or bone marrow involvement with cytopenias may be the initial presentation rather than the primary tumor. Other manifestations may include refractory hypertension and diarrhea due to tumor secretion of hormones such as norepinephrine and vasoactive intestinal peptide [15].
Diagnosis and staging includes CT (abdominal lesions) or MRI (paraspinous lesions) and biopsy if feasible. Neuroblastomas concentrate meta-iodo-benzyl-guanidine (MIBG), thus an MIBG scan should be performed if available [16]. Urinary catecholamines, homovanillic acid (HVA), and vanillylmandelic acid (VMA), should be obtained and are elevated in more than 90% of patients. Bone marrow examination completes the staging evaluation [17].
Neuroblastoma treatment is based on risk including age, stage of disease, and tumor features such as histology, DNA ploidy, 11q aberration, and MYCN amplification [18]. The International Neuroblastoma Risk Group (INRG) stages disease based on metastatic disease (stage M), image defined features suggestive of resectability in those without metastatic disease (L1 or L2) or patients <18 months of age with metastatic disease but no bone involvement (MS) [17, 19]. MYCN amplification confers high risk regardless of other factors and requires intensive chemotherapy, radiation when able and immunotherapy [18, 20]. When MYCN amplification is not present (90% of infants), subsequent treatment ranges from surgery alone to the intensive therapy just described depending upon other risk features [18]. Spontaneous regression is a unique possibility in infants with neuroblastoma [21]. When a small adrenal mass is the sole manifestation, expectant observation has been successful with 100% survival and sparing 81% eventual surgery [22]. Infants with stage MS may also experience spontaneous regression of their tumors. In one Children’s Oncology Group study, 55% required only supportive care; however, some may develop respiratory compromise due to extensive liver involvement and require chemotherapy and/or radiation therapy as symptomatic infants under 2 months of age are at the highest risk of mortality [23, 24].
While prognosis is similar in neonates and older infants with neuroblastoma of similar biologic features, the overall prognosis in infants is superior to older children as most lesions in this age group are lower stage, respond well to therapy and, in some cases, spontaneously regress [25–27]. The 5 year OS approaches 80% for children less than 1 year at diagnosis and >95% for infants with neuroblastoma without MYCN amplification [25, 28].
Benign adrenal masses are common occurrences in the prenatal and newborn period and are commonly adrenal hemorrhage or subdiaphragmatic extralobar pulmonary sequestration (SEPS) [29]. Though the majority of these lesions spontaneously regress, it is important to distinguish them from adrenal malignancies such as neuroblastoma [29]. Adrenal hemorrhage is the most common neonatal adrenal mass and may present unilaterally or bilaterally [29]. Most adrenal hemorrhages spontaneously resolve, thus careful observation is sufficient.
Subdiaphragmatic extralobar pulmonary sequestration (SEPS) is a rare congenital anomaly composed of nonfunctioning pulmonary tissue. These sequestrations may be found within the lung or below the diaphragm and have similar ultrasound appearance to neuroblastoma. Prenatally detected neuroblastoma is 2.5 times more common than SEPS [30]. SEPS are identified in the second trimester and are usually left-sided echogenic masses; neuroblastomas are identified in the third trimester and are usually right-sided cystic masses [30]. In fact, approximately 25% of neuroblastomas diagnosed in the perinatal or neonatal age are cystic [27].
Non-CNS Germ Cell Tumors
Germ cell tumors (GCT) are a heterogeneous group of benign and malignant neoplasms derived from primordial germ cells. In neonates, they are the most common neoplasm accounting for 35%–40% of all tumors in the first month of life [31]. In order of prevalence, the most common histologic subtypes of germ cell tumors in the neonate include teratoma (mature or immature), yolk sac tumor and choriocarcinoma [32]. Though most are benign in the neonatal period, there remains a high morbidity rate due to hydrops, premature delivery, and peri-operative and post-surgical anatomical defects.
Teratoma is the most common GCT in neonates. Teratomas are equally divided between mature and immature histologic types, the latter having a higher incidence of yolk sac components [32]. Most teratomas are extra-gonadal and frequently occur in the sacrococcygeal region but may arise in any midline location. Sacrococcygeal teratomas (SCT) present as an extrapelvic mass protruding between the coccyx and rectum. Hereditary SCT, which are less common, are almost always presacral and may be an isolated finding or part of the Currarino triad (presacral tumor, anorectal malformations, and sacral anomaly) [33]. Hereditary SCT are less likely to contain malignant elements [32]. Treatment generally consists of complete, early surgical resection often with coccygectomy taking extreme care to avoid tumor rupture and spillage which may lead to serious life threatening bleeding complications [24]. Congenital head and neck teratomas, though infrequent (4%), may present unique challenges including potential need for ex-utero intrapartum treatment (EXIT) to establish a patent airway [34]. In addition to surgery, platinum-based chemotherapy protocols have been successful in SCT with malignant features [24]. After treatment, monitoring for recurrence with physical exams and serum tumor markers (if elevated at diagnosis) is paramount as most recurrences occur within 3 years.
Yolk sac tumor (YST) is the most common malignant GCT in infancy [32]. Other synonymous terms for YST include endodermal sinus tumor, orchioblastoma, Teilum’s tumor, and clear cell adenocarcinoma [35]. On macroscopic exam, these tumors often appear cystic and yellow with areas of hemorrhage, necrosis and liquefaction [35]. Alpha fetoprotein (AFP) is typically elevated at diagnosis and should raise the suspicion for malignant yolk sac components even in those with teratomas. It is important to remember that AFP at birth is significantly higher than normal adult ranges and thus an infant’s AFP levels must be compared to infant norms until greater than 1 year of age [36]. Successful treatment outcomes involve surgical resection and in rare cases platinum-based chemotherapy.
Choriocarcinoma is a rare tumor in neonates that is highly fatal if left untreated. In neonates, choriocarcinoma is thought to arise as metastatic disease from a focus of choriocarcinoma in the placenta. Patients often present with anemia, failure to thrive, hepatomegaly, respiratory distress, and seizures. Evaluation should include measurement of human chorionic gonadotrophin (β-hCG) which is often markedly elevated [37]. Unlike most GCT, surgical resection alone is not curative and is not recommended upfront due to friability of the tumor and potential for bleeding. Whereas a high mortality was historically seen in affected neonates, more modern approaches with platinum-containing multi-agent chemotherapy has improved survival [35].
Soft Tissue Tumors
Sarcomas are of mesenchymal origin and are the fifth most prevalent malignancy in infants with an incidence of 1.6/100,000 in children less than 1 year of age [38]. In neonates they comprise 11% of non-CNS solid tumors. Age correlates strongly with the epidemiological pattern and clinical behavior of various soft tissue sarcomas (STS) within the pediatric population [39]. Neonates experience a uniquely different distribution of soft tissue tumors as compared to older patients with only one-third of neonatal STS comprising rhabdomyosarcoma followed by infantile fibrosarcoma [4, 40].
Rhabdomyosarcoma (RMS) in newborns comprise only 1%–2% of all RMS patients and are rarely diagnosed prenatally. Clinical symptoms vary and are dependent upon mass effect on surrounding organs by these rapidly proliferating tumors. Based on the Intergroup Rhabdomyosarcoma Studies (IRS), approximately 40% of RMS occur in the head and neck region, followed by the genitourinary tract (slightly less than 25%), and then extremities (approximately 20%) [41]. Within the neonatal period, tumors in the face or neck region may be misdiagnosed as vascular tumors or oropharyngeal teratomas. Twenty percent of patients at diagnosis have regional lymph node involvement and distant metastases commonly involving the lungs, bone marrow, and bones. The presence of metastatic skin lesions and early metastatic brain lesions are more common in neonatal RMS [42].
Sufficient tumor tissue is required for complete characterization. Histologically RMS is grouped into two main subgroups: embryonal (ERMS) and alveolar (ARMS). ERMS has a better prognosis than ARMS which is characterized by the t(2;13) or t(1;13) chromosomal translocations [43]. Diagnostic workup includes MRI or CT scan of the primary lesion, chest CT, bone scan, and bone marrow evaluation. These tumors are rarely resectable at diagnosis. Therapeutic management is divided into systemic (chemotherapy) and localized therapy (surgery and/or radiation therapy). Chemotherapy varies based on the site and stage of tumor, but in order to minimize toxicity dose-modifications are made in the management of neonatal RMS. Overall, the IRS Group reported a 3 year OS of 49% in newborns [44], and in the SEER database a 5 year OS of 38% [39].
Fibroblastic-myofibroblastic tumors are relatively frequent soft tissue tumors in children less than 1 year of age. Morphology frequently mimics sarcomas and their histology may be inconsistent with clinical findings making the diagnosis difficult. These tumors frequently present as large unresectable tumors posing a therapeutic challenge to surgeons and oncologists. Current therapeutic strategies involve a multidisciplinary approach with the use of systemic therapies to reduce sequelae of radical surgery.
Fibromatosis is a major subgroup of fibroblastic-myofibroblastic tumors and can occur in three forms: solitary, multicentric, or generalized. Solitary fibromatosis can occur at a multitude of sites; surgery is the mainstay of treatment and local recurrence is likely with incomplete resection. Unresectable tumors may be monitored closely for regression. Systemic therapy is often necessary for lesions in precarious locations or those that are progressive and/or symptomatic. Low-dose chemotherapy may play a role in the management of aggressive fibromatosis; however, the role for adjuvant chemotherapy remains unclear. Therapy may also be initiated with non-cytotoxic agents such as anti-inflammatory agents or hormonal therapy [45]. If possible, deferment of chemotherapy or radiation therapy is most advantageous until these children are older. Desmoid type fibromatosis can be sporadic or can arise within the setting of familial adenomatosis polyposis (FAP) including the Gardner’s variant. Potential drivers of tumorigenesis involve mutations of beta-catenin, CTNNB1, and the APC gene on chromosome 5q21 [46]. Typically, these tumors are deep-seated masses without a pseudocapsule and are located within musculo-aponeurotic structures (neck, chest, extremities, abdominal wall) rendering them difficult to resect. Even with wide resection, recurrence rate is high.
Hemangiopericytomas (HPC), now termed as myofibroma, are rapidly growing, highly vascularized soft tissue neoplasms of pericytic origin. These usually arise in the lower extremities or pelvis. Congenital hemangiopericytoma represent about one-third of pediatric HPCs, and are considered a distinct entity from the adult form of the disease. Most infantile hemangiopericytomas are benign. These tumors may regress but often require multimodal therapeutic approaches including surgery, chemotherapy, and radiotherapy if they possess aggressive features [47–49].
Infantile fibrosarcoma (IFS) is classified as a soft tissue tumor with an intermediate prognosis. They represent approximately 5%–10% of sarcomas in children younger than 12 months [50, 51]. Sixty percent of cases are diagnosed before 3 months of age, with 30%–50% of these noted at birth or diagnosed in utero [40, 52]. The translocation t(12;15) with the transcript ETV6-NTRK3 is characteristic for IFS [53]. IFS generally present as an enlarging non-inflammatory mass and are often highly vascular with ulceration. Typical locations for IFS are within the soft tissue of the extremities (66% of cases), followed by the trunk (25%), and then head and neck (7%) [51]. Distant metastases are rare and prognosis is favorable with greater than 80% survival [50, 54]. Tumors not primarily resectable may be monitored for spontaneous regression. Chemotherapy may be considered in an effort to render tumors more easily resectable. Vincristine and actinomycin (VA) are the chemotherapeutic agents of choice however more intensive therapy may be needed [54].
Leiomyosarcoma behaves benignly in the neonatal period. These tumors frequently arise in the intestines and may present with aseptic chemical peritonitis due to gut perforation with meconium peritonitis or intestinal obstruction. Management is surgical [55].
Central Nervous System Tumors
Central nervous system (CNS) tumors are the most common solid tumor in pediatrics, most commonly are low grade gliomas and most commonly arise in the posterior fossa [56]. In contrast, neonatal CNS tumors are extremely rare making up 0.5%–1.9% of all pediatric brain tumors [57], are more frequently supratentorial, and are most commonly teratomas [58]. Prenatal ultrasound may identify CNS tumors prior to birth due to enlarged head circumference, abnormal brain or skull development or visualization of the tumor itself. Prenatal MRI may be utilized to better image the mass and allow for safer delivery planning [59]. Survival for neonatal CNS tumors is very poor. A California center reviewed 250 cases and showed a 28% survival with 21% of deaths being stillbirths. For the most commonly encountered tumor, teratomas, only 12% survived [60]. Tumors that are identified prior to 30 weeks’ gestation have nearly 100% mortality [59].
Teratomas, more frequent outside of the CNS, are the most common intracranial neoplasm representing up to 50% of cases. Teratomas most commonly arise in the midline (i.e., pineal or suprasellar region) but may occur in the cerebral hemispheres or cerebellum. A solid and cystic mass with mineralization (calcifications) may be identified on imaging with more invasive, larger masses with more significant solid components pointing towards a more immature, malignant form [59]. Serum and/or cerebrospinal fluid (CSF) tumors markers such as AFP and β-hCG may aid in the diagnosis and if elevated point to a malignant component [61]. These tumors may grow very large leading to poor cerebral development, macrocephaly, and commonly result in fetal demise [62]. Rarely, surgically removed mature teratomas may result in long-term survival [63].
Gliomas arise from multiple cells of origin anywhere in the brain or spine and include astrocytic tumors, oligodendroglial tumors, oligoastrocytic tumors, and ependymal tumors. Histologic grading ranges from WHO Grade I (most commonly pilocytic astrocytoma) to WHO Grade IV (most commonly glioblastoma) [64]. Molecular profiling is increasingly incorporated into the comprehensive diagnosis and helps classify these entities into various prognostic groups with many new therapeutic targets [65]. Low grade gliomas are the most common CNS tumor in pediatrics and they most commonly arise in the posterior fossa [56]. In contrast, gliomas are the second most common CNS tumor in neonates, more commonly arise in the cerebral hemispheres, are 1.5 times more likely to be higher grade, and often present with macrocephaly, hydrocephalus and hemorrhage [66]. In a large series overall survival for astrocytic tumors was 30%; however, if separating low grade and high grade tumors, the survival ranges from 90% to 20%, respectively [58, 60, 66]. Complete surgical resection of low-grade gliomas is considered curative. For unresectable tumors, options increasingly include use of targeted agents after molecular profiling [67]; however, traditional chemotherapy approaches remain first line. In neonates, radiation is not a viable option.
Subependymal giant cell astrocytoma (SEGA) may present in the neonatal period with hydrocephalus or a large mass in up to 2% of patients with tuberous sclerosis complex (TSC) and these patients more commonly have TSC2/PKD1 mutations [68]. Surgical resection remains the preferred treatment for SEGA, however, treatment with mTOR inhibitors (Everolimus) can be attempted where results in older pediatric patients have shown around 80% of patients had a 50% or more reduction in tumor volume [69]. Tumor size reduction may lead to safer surgical options.
Embryonal tumors include medulloblastoma, atypical teratoid rhabdoid tumor (ATRT) and the group formally classified as primitive neuroectodermal tumor (PNET) [65]. In neonates, the most common embryonal tumors are medulloblastoma and ATRT and both are aggressive tumors with high frequency of CNS metastasis. Up to 66% of patients with congenital rhabdoid tumors have been reported to have rhabdoid tumor predisposition syndrome due to germline SMARCB1 or rarely SMARCA4 mutations and must be screened for synchronous malignant rhabdoid tumors of the kidney and soft tissues [70, 71]. Unless a gross total resection can be achieved in a patient without metastatic disease palliative care may be warranted without therapy given the poor prognosis [71]. Even with aggressive treatment the survival rate is approximately 40% [72]. Medulloblastomas by definition arise from the cerebellum and have been divided into multiple molecular subgroups with infant tumors most commonly falling into the sonic hedgehog (SHH) subtype [73]. For infants with medulloblastoma, Gorlin syndrome (nevoid basal cell carcinoma syndrome) due to mutations in PTCH1 in the SHH pathway must be considered as a predisposing factor [74]. Molecular profiling and classic clinical staging such as metastatic disease state and extent of resection both play a role in prognostication. Although radiation is effective, it is avoided in the youngest patients and treatment instead includes only aggressive chemotherapy approaches often including high dose chemotherapy with autologous stem cell rescue. The outcome with this approach has been reported to result in 5 year OS as high as 76% [75]. Although radiation in infants is avoided these patients are still left with significant neurocognitive dysfunction [76, 77].
Choroid plexus tumors arise in the ventricles and are divided into three WHO Grades: WHO Grade I choroid plexus papilloma, WHO Grade II atypical choroid plexus papilloma, and WHO Grade III choroid plexus carcinoma [64]. Choroid plexus tumors may be identified by ultrasound imaging showing the intraventricular mass or present with massive hydrocephalus due to overproduction of CSF [78, 79]. Choroid plexus papillomas may be treated with surgical resection alone; however, choroid plexus carcinomas require aggressive chemotherapy even after complete resection and survival is poor [80]. Patients with choroid plexus carcinoma have a high risk of a germline mutation in TP53 (Li–Fraumeni syndrome) and should undergo genetic screening [81].
Renal Tumors
Renal neoplasms comprise 7% of all neonatal tumors [82]. Congenital mesoblastic nephroma is most prevalent followed in incidence by the malignant tumors Wilms tumor, rhabdoid tumor, and clear cell sarcoma.
Congenital mesoblastic nephroma is the most common renal mass in neonates accounting for approximately 60% of cases [82–84]. It is a tumor predominantly of infants (median age 1–2 months) presenting typically as a unilateral large mass often associated with polyuria, hypertension, hypercalcemia, and occasionally congestive heart failure [85]. Prenatal diagnosis of CMN is seen in 15% of cases [84]. Metastatic disease is rare primarily occurring with relapse [86]. Histologically three subtypes are recognized: classical (most common), cellular, and mixed (least common) [83, 84]. The cellular subtype is often (58%) characterized by the translocation t(12;15)(p13p15), a fusion of ETV6 and NTRK3 genes that is also seen in infantile fibrosarcoma [87]. Treatment is complete surgical resection (achieved in >80%) via radical nephrectomy which is curative in more than 90% of cases [83, 84, 86]. Chemotherapy is reserved for large unresectable tumors or after relapse (most common among cellular subtypes) [88, 89]. Surgical complications are frequent (23%) and half of deaths due to CMN are associated with surgical complications occurring primarily in the youngest patients, emphasizing the need for care in experienced centers [84, 90]. Infants younger than 2 months with stage III tumors (incomplete resection or tumor spillage) may be observed as later recurrence is typically retrievable with surgery and/or chemotherapy [84].
Wilms’ tumor is the most common pediatric renal tumor but represents only 20% of neonatal renal tumors [83, 86]. Occurrence is often sporadic though a small percentage of diagnoses are associated with congenital syndromes (Beckwith–Wiedemann, WAGR, and Denys–Drash) [82, 91]. Tumors may be unilateral or bilateral (rare) and typically present as a palpable abdominal mass with or without associated abdominal pain, distention, and hypertension. Almost all bilateral Wilms’ tumors contain nephrogenic rests but in unilateral Wilms’ tumor these abnormal foci increase the risk of developing bilateral Wilms’ tumor and must be carefully monitored [92]. Histologic subtypes include favorable and anaplastic histology though the latter is rarely seen in neonates. Treatment often involves radical nephrectomy, adjuvant chemotherapy and in cases of tumor spillage, radiation to the primary tumor site. Cure rates are >90% with poorer outcomes seen in patients with metastatic disease, anaplastic histology and other unfavorable prognostic factors [86]. For those with stage I (completely resected with no capsular invasion) favorable histology tumors weighing <550 g, chemotherapy may be deferred to use only in those who recur [93].
Rhabdoid tumor of the kidney (RTK) is a rare but lethal disease seen in 11% of neonates with renal tumors [83, 94]. Universal to RTK is the loss of function of the SMARCB1/INI1 gene located on chromosome 22q11.2 resulting in INI1 negative immunostaining. This mutation is germline in 25% of patients [95]. Patients usually present with an abdominal mass and associated fever and hematuria. Often advanced stage disease is present at diagnosis due to the high potential for brain, bone, liver, abdominal, and lung metastasis [83, 86]. The high prevalence of brain metastases (26%) mandates early imaging [83]. Treatment generally follows high risk renal tumor protocols with surgical resection, chemotherapy, and radiation. Despite treatment, outcome is poor with survival in neonates <10%–20% [83, 86, 94].
Clear cell sarcoma of the kidney (CCSK) is a rare (<2%–3%) diagnosis in the neonate. Present in nearly all cases is the BCOR mutation [96]. Patients typically present with palpable abdominal mass with associated hypertension, hematuria, and abdominal pain. This aggressive tumor often metastasizes to bone but may also involve brain, lungs, and liver [89]. Treatment involves complete surgical resection, chemotherapy, and radiation [83]. Outcomes for neonates with CCSK are superior to that of older children as most neonates who are treated survive [83], though prognostic information is limited in this group.
Retinoblastoma
Retinoblastoma is the most common tumor of the eye in children and accounts for 1%–3% of all childhood malignancies [97]. In neonates, retinoblastoma almost exclusively occurs in offspring of parents with retinoblastoma 1 (RB1) gene mutation of chromosome 13q14.2. Older infants and children may be noted to have leukocoria, strabismus, and lack of red reflex. Differential diagnoses of leukocoria includes congenital cataracts, toxocariasis, retinopathy of prematurity, persistent fetal vasculature, retinal detachment, and vitreous hemorrhage [98]. The American Association of Ophthalmic Oncologists and Pathologists recommends children without a family history undergo red reflex testing at routine visits until 5 years of age, at which time the retina is mature.
Recommendations for children with RB1 mutation or positive family history include more frequent examinations [99]. RB1 testing may be performed upon delivery or prenatally via amniocentesis between 16 and 33 weeks’ gestation [100]. Children with RB1 mutation may have unilateral tumors but the other eye may become affected. Bilateral retinoblastoma tends to occur in children with germline mutation and is typically seen in younger patients (14–16 months) than unilateral retinoblastoma (29–30 months) [101–103]. Children with suspected retinoblastoma need an MRI to determine extent of disease including evaluation for possible trilateral retinoblastoma with pineal involvement.
Treatment, based upon the degree of retrievable vision and extent of disease, includes enucleation of the eye, intravenous chemotherapy, and intravitreal chemotherapy. Infants greater than 3 months of age may receive intra-arterial chemotherapy via the ophthalmic artery. Bridge therapy with intravenous carboplatin until 3 months of age and 6 kilograms in weight has successfully been utilized for neonates [104]. Overall survival exceeds 90% [4, 105].
Children with RB1 mutation are predisposed to secondary malignancies including STS and breast cancers. The American Association of Cancer Research has published recommendations for surveillance [106].
Hepatic Tumors
Hepatic tumors are uncommon in the perinatal period accounting for only 2%–7% of solid tumors [107–109]. Benign tumors such as infantile hemangioma and mesenchymal hamartoma are more predominant than malignant tumors during this period.
Infantile hemangiomas are the most common benign tumors of the liver in the fetus and neonate and often present as multiple liver lesions [110, 111]. These highly vascular tumors are characterized by rapid proliferation in the neonatal period followed by a slower period of involution during childhood. Though benign, they may lead to serious complications including consumptive coagulopathy, severe anemia, and high output cardiac failure. Treatment and outcomes are detailed in the section on Vascular Tumors.
Mesenchymal hamartoma is the second most common benign tumor of the liver in fetuses and neonates and presents as a multicystic liver mass [112]. These fluid-filled masses are characterized by rapid growth and expansion often leading to abdominal distention, respiratory distress, and compression of surrounding vessels and organs [113]. Severe, life-threatening complications such as fetal hydrops, congestive heart failure, and still birth may also occur [113]. Treatment consists of surgical resection when feasible. If surgery is not an option then close ultrasound monitoring until surgery can take place is warranted [114, 115]. One study showed 76% survival with surgery compared to 64% survival for all patients with mesenchymal hamartoma [112].
Hepatoblastomas are the most common primary hepatic malignancy [116]. though most hepatic malignancies in the fetus and neonate are actually metastatic lesions from other tumor sites. Neuroblastoma, GCT, renal tumors, RMS, and leukemias are some of the malignancies that can metastasize to the liver [117].
Hepatoblastoma incidence has increased possibly owing to increased survival of preterm and low birth weight infants and their associated increased risk of hepatoblastoma [118, 119]. These tumors often present as a firm, palpable mass with associated abdominal distention and pain. Hepatoblastoma may be associated with genetic syndromes such as Beckwith–Wiedemann, Li–Fraumeni, FAP, and trisomy 18, thus a comprehensive family history and genetic testing is indicated [120]. AFP levels are elevated in approximately 70% of cases, while lower AFP levels are associated with more aggressive features and poorer outcomes [121]. Thrombocytosis may also be present as part of a paraneoplastic effect. Treatment consists of surgical resection alone for well-differentiated fetal histology hepatoblastoma, but pre-operative platinum-based chemotherapy may be utilized to reduce tumor volume. Patients with other histologic subtypes of hepatoblastoma all receive chemotherapy regardless of extent of resection. Liver transplantation is reserved for patients with unresectable disease after neoadjuvant chemotherapy [122, 123]. Past studies suggested worse outcomes in neonates with hepatoblastoma but more recent cooperative group trials have significantly improved outcomes which are now comparable to or better than older children with current 5 year OS in excess of 85%–90% [112, 124, 125].
Vascular Tumors
Vascular tumors are the most common soft tissue and subcutaneous neoplasm in infants. Differentiating amongst the various types of vascular tumors and more importantly between vascular tumors and sarcomas may be difficult [126]. In neonates, the primary vascular tumors are benign congenital hemangiomas that arise prenatally and are present at birth, benign infantile hemangiomas that arise late in the first month from pre-existing telangectasias or areas of skin discoloration, and borderline, locally aggressive kaposiform hemangioendotheliomas and their variant tufted angiomas.
Hemangiomas are a benign neoplasm with a predilection to arise in the head and neck region. Cutaneous infantile hemangiomas (IH) are the most common benign vascular tumor of infancy occurring in 4%–5% of infants, are more prevalent in premature infants and commonly manifest at the age of 3–6 weeks [127, 128]. An initial phase of rapid proliferation lasting an average of 5 months followed by a slow involutional phase occurring over years is typical [129, 130]. IH is not associated with coagulopathies. Diagnosis is typically clinical with biopsies rarely needed; however, histopathology should include GLUT1 as endothelial cells in IH express GLUT1, whereas congenital hemangiomas do not. Underlying malformations should be ruled out, e.g., PHACE syndrome [131]. Visceral hemangiomas, most frequently involving the liver, should be sought in infants with more than five cutaneous hemangiomas [130]. Most hemangiomas require no intervention, but in functional impairment or dramatic aesthetic concerns, may require treatment [132, 133]. Beta blockers, such as propranolol [134], are most commonly utilized in the setting of diffuse or multifocal hepatic hemangiomas displaying symptoms such as high cardiac output failure or profound hypothyroidism. Other medical treatment options include steroids, laser therapy, excision, and in diffuse visceral lesions, even cyclophosphamide or vincristine have been used [135, 136]. If medical management is unsuccessful liver transplant may be indicated [137]. Vascular cutaneous lesions present at birth are most frequently congenital hemangiomas (CH) [130, 138]. These tumors present at birth, typically regress and do not grow further unless internal hemorrhage occurs. Coagulopathy has been associated with these types of hemangioma. Therapy for CH typically is supportive but may require embolization or surgery.
Kaposiform hemangioendothelioma (KHE) (and the variant tufted angioma) is an extremely rare aggressive vascular neoplasm, with 60% of cases occurring within the neonatal period. KHE are commonly located in the retroperitoneum and deep soft tissues of the extremities (83% of the cases) [139]. Superficial soft tissues, scalp, neck, chest wall, and mediastinum involvement have also been reported. KHE is most often solitary. Infants with KHE frequently (70%) experience the consumptive coagulopathic Kasabach–Merritt phenomenon (thrombocytopenia, hypofibrinogenemia, elevated d-dimers). Patients with larger visceral tumors have a 40%–50% mortality rate [40]. MRI is preferred as the imaging modality and if feasible histologic confirmation is advised. Treatment varies based upon severity of the case. Due to size, site, and involvement of several tissue planes, there is often an inability to safely resect these tumors. Initial medical treatment is most commonly corticosteroids [140], followed by vincristine [141]. Other therapeutic options include antiplatelet therapy [142], interferon-alpha [143], anti-fibrinolytic therapy, chemotherapy, propranolol [144], embolization [145], and sirolimus as a monotherapy or in combination with steroids [146]. Even with therapy, KHE often do not fully regress and may recur [147].
Histiocytic Disorders
Histiocytic diseases are defined by clonal proliferation of histiocytes, which are normal cells in the skin and bone marrow, leading to tissue destruction, cytokine release, and variable clinical appearance. This family of disorders includes Langerhans cell histiocytosis, hemophagocytic lymphohistiocytosis, juvenile xanthogranulomatous disease, and sinus histiocytosis with massive lymphadenopathy/Rosai–Dorfman. These are rare in the general population, but especially so in the neonatal period. Of the histiocytic disorders, the most common in infants include Langerhans cell histiocytosis and hemophagocytic lymphohistiocytosis.
Langerhans cell histiocytosis (LCH) most commonly presents with skin rash (50%) and bone lesions (10%) [148]. In neonates skin involvement is more prevalent, present in 86%–92% [149]. The neonate may present with “blueberry muffin rash” or other skin findings that may self-resolve. This has been referred to in the past by a variety of names including congenital self-healing reticulohistiocytosis, histiocytosis X, and Hashimoto-Pritzker syndrome. The differential diagnosis includes seborrheic dermatitis, diaper dermatitis, and chronic otitis media. The rash of LCH is a diagnostic challenge as it has varying appearance of vesiculo-pustules, molluscum, or petechial rash and can be nonspecific. Subcutaneous nodules of LCH present similarly to neuroblastoma, congenital leukemia, mastocytosis, and vascular lesions. When presenting as vesicles or bullae, LCH of the skin appears similar to erythema toxicum, herpes simplex or varicella infection, miliaria cystallina or rubra, neonatal pustular melanosis or incontinentia pigmenti [148]. Children have the potential to develop disseminated disease. Most concerning is involvement of risk organs which include liver, spleen, and bone marrow but disease may also commonly involve lungs, lymph nodes, and other tissues. Current nomenclature is to define the organ systems involved, either single system or multisystem and include risk organ involvement status. Incidence in the neonatal period is estimated at one to two cases per million [150]. Of neonates enrolled on LCH trials, 59% had multisystem involvement [149]. Biopsy of an LCH lesion may demonstrate CD1a positivity, S100 positivity and Langerin/CD207 positivity by immunohistochemistry. In young children, there is a more severe form of the disease that includes skin, risk organs, and the central nervous system which was previously called Letterer–Siwe disease. In neonates with multisystem involvement the 5 year OS was 57%, lower than in those with single system involvement (94% 5 year OS) and worse than older children with multisystem involvement [149, 151]. Treatment of LCH may include topical agents for isolated skin disease or systemic chemotherapy for multisystem disease. Surveillance for disease reactivation is imperative for up to five years following diagnosis [152].
Hemophagocytic lymphohistiocytosis (HLH) classically presents as fevers, failure to thrive, hepatomegaly, splenomegaly, liver failure, thrombocytopenia, and hydrops in the neonatal period [151]. Fever and hypertriglyceridemia may be less common in neonatal HLH as compared to older children, thus one must have a high index of suspicion [153]. Primary (familial) and secondary (acquired) HLH have similar presentations and are often difficult to distinguish. Positive family history may be of assistance and often other children were born with rapid decline and typically death occurs without specific therapy. Most common genetic mutations are in the Perforin, Syntaxin and Munc genes though a good portion of children with suspected primary HLH do not have an identified mutation to date [154]. Clinical diagnosis may be made by either genetic confirmation of pathogenic mutation or five of the eight clinical criteria: fever, lymphadenopathy, hepatomegaly or splenomegaly, elevated ferritin >500 ng/mL, serum triglyceride level >265 mg/dL or fibrinogen <150 mg/dL, hemophagocytosis on pathologic specimen, elevated serum interleukin 2 level >2,400 units/mL, and impaired natural killer (NK) cell activity. With HLH-directed therapy, survival in all ages is approximately 61% [155, 156]. In neonates the few reports have noted less optimistic outcomes between 26%–40% [151, 153]. Given the nonspecific clinical appearance of children with HLH, other diagnoses including sepsis and immune deficiencies must be considered.
Juvenile xanthogranuloma (JXG) typically presents as a cutaneous yellow nodule or papule that is most commonly located on the head, upper trunk, or neck. JXG makes up 20% of histiocytic diagnoses at birth in one review, however, the median age of diagnosis is 2 years [151, 157]. Natural history of the disease is slow resolution over a period of 3 to 6 years [158]. Cutaneous disease is most common with deep seated lesions less so (27% of neonates). Lesions can be seen in the liver, lung, soft tissue, spleen, eye, and brain. JXG lesions may present similarly to hematoma, LCH, myofibroma, sarcoma, and IH [158]. Ocular disease is more common in children less than 2 years of age and presentations may include unilateral hyphema, glaucoma, or exophthalmos [157]. Treatment is usually supportive, however, intervention may be required for those with systemic disease [151]. Screening ophthalmologic exams to monitor for ocular involvement is recommended until the age of 2 years [157].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree