Abstract
Thromboembolism (TE) in pediatrics is relatively rare compared with adults, with an estimated venous thromboembolism (VTE) incidence of 0.07–0.14/10,000 children [1, 2]. A bimodal age distribution has been well demonstrated in the pediatric VTE population and children less than 1 year of age, especially those less than 1 month of age, are most commonly affected [1, 2]. The incidence of VTE in this very young population, particularly when hospitalized, is increasing [3–6]. Between 1997 and 2018, up to a 13-fold increase in neonatal TE incidence has been described in all live births and a greater than six-fold increase in neonatal TE incidence has been described for neonatal intensive care unit (NICU) admissions [4–7]. This increase has been attributed to improving survival rates in critically ill and/or premature neonates, the increased utilization of central venous catheters (CVC), and a much greater awareness of VTE and the associated risk factors in this population [3, 6, 8, 9]. The aim of this chapter is to review the congenital and acquired risk factors associated with neonatal TE and to discuss the clinical presentation, diagnosis, and management of this rare complication that has been shown to significantly impact the morbidity and mortality rates of those afflicted [1–3, 8].
Introduction
Thromboembolism (TE) in pediatrics is relatively rare compared with adults, with an estimated venous thromboembolism (VTE) incidence of 0.07–0.14/10,000 children [1, 2]. A bimodal age distribution has been well demonstrated in the pediatric VTE population and children less than 1 year of age, especially those less than 1 month of age, are most commonly affected [1, 2]. The incidence of VTE in this very young population, particularly when hospitalized, is increasing [3–6]. Between 1997 and 2018, up to a 13-fold increase in neonatal TE incidence has been described in all live births and a greater than six-fold increase in neonatal TE incidence has been described for neonatal intensive care unit (NICU) admissions [4–7]. This increase has been attributed to improving survival rates in critically ill and/or premature neonates, the increased utilization of central venous catheters (CVC), and a much greater awareness of VTE and the associated risk factors in this population [3, 6, 8, 9]. The aim of this chapter is to review the congenital and acquired risk factors associated with neonatal TE and to discuss the clinical presentation, diagnosis, and management of this rare complication that has been shown to significantly impact the morbidity and mortality rates of those afflicted [1–3, 8].
Risk Factors
Developmental Hemostasis
Developmental hemostasis is a term used to describe the physiologic changes in the dynamic hemostatic system evolving from intrauterine life, through the neonatal and pediatric time periods, into its maturation in adulthood [10]. The variations in procoagulant and anticoagulant activities in neonates compared with adults has been well described and is even more pronounced in premature infants [11, 12]. At birth, the plasma concentration of procoagulants factor (F) V, FVIII, FXIII, and von Willebrand have been shown to have similar, if not increased, activities compared to adult levels [10, 13]. All vitamin K dependent factors, including procoagulant FII, FVII, FIX, and FX and anticoagulant proteins C and S, are decreased and can take months to even years to reach adult normal values [13]. Procoagulants FXI and FXII, have also been shown to be decreased compared to adult norms, and anticoagulants antithrombin and plasminogen have also been shown to have significantly less activity in neonates [10, 13].
Although these differences seem to infer a prothrombotic state, other factors, including a decreased ability to generate thrombin, provide a balance that prevents spontaneous TE in otherwise well neonates [14]. However, if other acquired or congenital risk factors are present (see Table 19.1), this balance can be disrupted, predisposing certain neonates to TE [15].
Table 19.1 Risk factors for the development of neonatal TE
| Maternal risk factors | Delivery risk factors | Neonatal risk factors |
|---|---|---|
|
|
|
Clinical Risk Factors
Studies have shown that male gender, extreme prematurity (<25–27 weeks’ gestational age), extremely low birth weight (<1,000 g), and prolonged NICU stay all increase the risk for neonatal TE [2–4, 16]. Most pediatric VTE are associated with at least one if not more clinical risk factors, and neonatal VTE are no different, with over 80% of symptomatic neonatal TE being associated with the presence of acquired risk factors (see Table 19.I) [1, 2, 4–6]. The primary risk factor associated with the vast majority of neonatal TE development is the presence of a CVC or arterial catheter, with a reported symptomatic CVC-associated VTE incidence of 2.2%–33.6% [2, 4, 5, 17–20]. The greatest VTE risk factor in premature infants is the presence of an umbilical venous catheter (UVC) [21]. Sepsis and any congenital heart disease have also been shown to carry significant risk in neonatal TE [7, 9].
Along with neonatal risk factors, there are maternal factors that directly affect the risk of neonatal TE. Maternal diabetes, hypertension, fetal thrombotic vasculopathy, preeclampsia, prolonged rupture of membranes, and chorioamnionitis have all been reported as risk factors, but the reports vary [7, 14, 22]. Maternal autoimmune conditions can also influence neonatal TE development. Maternal antiphospholipid antibodies, including anticardiolipin, β2-glycoprotein, and lupus anticoagulant, seem to confer a significant risk of neonatal TE, especially perinatal arterial ischemic stroke (PAIS). These antibodies can cause placental thromboses or may cross the placenta and directly influence TE development in the neonate [23–25].
Inherited Thrombophilia
The role of inherited thrombophilia (IT) in neonatal TE is poorly defined [26]. The literature is scarce, but between 20% and 33% of neonatal TE has been associated with IT [4, 6]. A recent systematic review of the literature found that while thrombophilic conditions may play a role in neonatal TE, clinical risk factors have more influence on the development of TE [27]. This seems to be particularly true regarding CVC related neonatal TE, where only few cases have an associated IT [28, 29]. More recent evidence has suggested that multiple IT or a combination of an IT and a clinical risk factor influence neonatal TE development [14]. Clinical risk factors seem to more heavily influence neonatal TE development, but IT evaluation may be appropriate in certain situations, especially in unprovoked TE or if there is a family history of TE, depending on the thrombosis severity, location, as well as the number of acquired risk factors present [30]. Due to the large volume of blood typically needed to perform the investigations, a step-wise approach can be used with only certain studies required during the acute event and others obtained around 3–6 months of life (see Table 19.2).
Table 19.2 Laboratory evaluation for inherited thrombophilia
| Laboratory testing if other acquired risk factors present | Laboratory testing if other acquired risk factors not present |
|---|---|
|
|
Notes: *May be performed from maternal serum during first few months of life.
** Protein-based assays are affected by the acute thrombosis and must be repeated at 3–6 months of life, before a definitive diagnosis may be made. Therefore, recommend that complete evaluation (excluding DNA-based assays) be performed at 3–6 months of life [107, 136]. If anticoagulation is being administered, then these assays should be obtained 14–30 days after discontinuing the anticoagulant. Lipoprotein(a) levels may need to be repeated at 8–12 months of life.
***DNA-based assays.
Adapted from Saxonhouse and Manco-Johnson. The evaluation and management of neonatal coagulation disorders. Semin Perinatol 2009;33:52–65, 59, with permission [14]. Refs: [131, 132, 136, 139, 140].
Activated protein C is a vitamin K dependent anticoagulant that inactivates the activated forms of FV (FVa) and FVIII (FVIIIa). A mutation in FV, most commonly FV Leiden (FVL), can lead to a resistance in activated protein C, resulting in a thrombophilic state. It is the most common IT, with heterozygous mutations affecting about 5% of the white European population, and it confers about a 5-fold increased TE risk and 80-fold increased TE risk in adults with heterozygous and homozygous mutations, respectively [31–34]. Although most individuals with a FVL mutation will not have their first TE event until later in life, there have been meta-analyses that have shown a significant association with FVL mutations and neonatal cerebral sinus venous thrombosis (CSVT) [35].
Prothrombin gene 2021 A (PTG) mutation is the second most common IT, as 1%–2% of the white European population is affected. This mutation increases circulating prothrombin, the precursor to thrombin, concentrations by 15%–30%, which increases the TE risk about two- to three-fold in the adult population [36, 37]. There have been reports of PTG mutations in neonatal TE, but these are rare, and other studies have shown no significant neonatal TE risk with this mutation [15, 35].
Protein C deficiency is a rare condition resulting in the inability to inactivate FVa and FVIIIa, which results in an approximate 10-fold increased risk of TE in the general population in those heterozygous for the mutation [38]. Although there are case reports and case series suggesting heterozygous protein C deficiency may increase arterial and venous TE in neonates, especially CSVT, numerous studies report that the risk of neonatal TE is relatively low [27, 39–41].
Homozygous protein C deficiency is rare, but manifests hours after birth with cerebral damage noted in utero, large vessel thrombosis, and most commonly purpura fulminans, a dermal vascular necrosis that causes a progressive hemorrhagic necrosis of the skin [42, 43]. Newborns will have a diffuse disseminated intravascular coagulation with resulting hemorrhagic complications with large bullae lesions primarily on the extremities, buttock, abdomen, scrotum, and other sites of pressure [44]. Treatment would include either fresh frozen plasma (FFP) at 10–20 ml/kg every 12 hours or the use of protein C concentrates until there is resolution of the skin lesions [45, 46]. After the initial treatment, protein C concentrates are safe, efficient, and available for prophylactic use in severe congenital protein C deficiency [47].
Protein S is a vitamin K-dependent endogenous anticoagulant that acts as a cofactor for the activated protein C inactivation of FVa and FVIIIa [48]. It usually circulates as an active free form and a complement 4B (C4B) bound inactive form, but, due to a deficiency of C4B, it circulates predominantly in the free form in neonates [49, 50]. A recent systematic review of the literature showed that very few neonatal and pediatric TE are due to heterozygous protein S deficiency [27]. Compound heterozygous and homozygous protein S deficiencies are rare and usually present at birth with purpura fulminans [51–53]. There are no isolated protein S concentrates available, so treatment involves FFP at 10–20 ml/kg every 12 hours until lesions resolve, with potential long-term pharmacologic anticoagulation to follow [54].
Antithrombin is a serine protease inhibitor that inactivates FIIa (thrombin), FIXa, FXa, FXIa, and FXIIa [55]. It may be acquired, especially in congenital nephrotic syndrome, or inherited. Heterozygous antithrombin deficiency has been reported in neonatal arterial and venous TE but is not associated with purpura fulminans. It is, however, associated with TE in unusual sites like the coronary arteries, the aorta, and the central nervous system [56–61]. Homozygous antithrombin deficiency is quite rare but has been implicated in severe spontaneous venous and arterial TE in neonates. Neonatal pulmonary artery TE, IVC/abdominal vein, and extremity venous TE have all been reported [62–64]. Treatment would require anticoagulation, but heparin may not be effective as it relies on antithrombin as a substrate so substitution of antithrombin with a plasma derived concentrate is usually required and has been shown to be effective [65].
Lipoprotein(a) (Lp(a)) is composed of a polypeptide chain and low-density lipid particle and is structurally similar to plasminogen. Due to the resemblance, it competes with plasminogen in binding to fibrin, which reduces fibrinolytic activity. Elevated levels of Lp(a) can reduce fibrinolytic activity significantly enough that TE risk is increased. Although pediatric venous and arterial TE have both been described, the true risk associated with neonatal TE and elevated Lp(a) is not well defined, but it seems that elevated Lp(a) may play a role in neonatal PAIS [66, 67].
Clinical Presentations and Locations of Neonatal TE
Locations for the variety of neonatal TE and the proper imaging modalities to diagnose them are presented below. Many of the gold standard imaging techniques used in adults are unable to be utilized in neonates, thus Doppler ultrasonography (US) is the most widely and safely used modality [20].
Arterial TE
Perinatal Arterial Ischemic Stroke (PAIS)
Perinatal arterial ischemic stroke refers to insults, ischemic or hemorrhagic, occurring from 20 weeks’ gestational age to 28 days postnatally. PAIS is defined as a condition with acute encephalopathy, seizures, or neurologic deficits presenting in the term or preterm infant before the 29th postnatal day with brain imaging confirming a parenchymal infarct in the appropriate arterial region [68, 69]. Most abnormalities occur in the left hemisphere within the distribution of the middle cerebral artery with the origin of the left carotid artery from the aorta allowing for a more direct vascular route to the brain as a corridor for cardiac emboli [23, 70]. Multi-focal cerebral infarctions may occur, but these tend to be embolic in origin. Many potential risk factors have been implicated in the etiology of PAIS (see Table 19.1). Between 22 and 70% of congenital hemiplegic cerebral palsy in neonates has been attributed to PAIS [23, 71, 72]. Other neurological comorbidities include seizure disorders, delayed language development, and behavioral disorders [25].
Placental pathology is a major risk factor for PAIS. Maternal/fetal conditions including fetal thrombotic vasculopathy and antiphospholipid antibody syndrome may result in emboli that break off the placental circulation and enter the fetal circulation [73, 74]. Studies have identified prothrombotic risk factors, especially elevated lipoprotein (a) and protein C deficiency, in as much as 68% of neonates with PAIS [66].
Screening for neonates with suspected PAIS can be done with cranial ultrasound (CUS) as it is the least invasive method. However, studies have found that 75% of cases of PAIS were missed using this modality alone [75]. Therefore, all cases of suspected PAIS should have MRI with diffusion-weighted imaging (DW MRI) performed [76]. This technique allows the detection of cerebral edema, which is an early sign of cerebral ischemic damage [77, 78]. Angiography can also be performed and allows for the detection of thromboses if there is a history of instrumentation/difficult delivery [79].
Iatrogenic/Spontaneous Arterial TE
Umbilical arterial catheters (UACs) and peripheral arterial catheters (PAL) are frequently used in the NICU (10%–64% of neonates) as means for continuous monitoring of arterial blood pressure and blood gases [15]. Femoral arterial catheters are used more frequently in neonates with congenital heart disease or those requiring extensive surgery. Despite their value, they can have devastating complications such as infection, limb loss, renal failure, and even death [80–82]. High UAC positioning (T6-9) has been found to have fewer clinical complication, while low dose continuous heparin infusion at 1 u/ml prolongs catheter patency but does not reduce the risk of TE [83, 84]. Catheter material, duration of placement, and solutions infused influence the risk for catheter related TE. Suspicion of an arterial TE should be confirmed by Doppler US but contrast angiography may be required for complicated cases [18].
Venous TE
Catheter-Related TE
Although vital to the improvement in care to the most critical of neonates, the presence of a central venous catheter (CVC) represents the greatest risk for TE. Additional risk factors further increase this risk. Providers must evaluate the risks and benefits every day that a CVC remains in place and prompt removal should occur whenever the risks of a CVC outweigh its benefits. Damage to blood vessel walls during insertion, disrupted blood flow, infusion of substances that damage endothelium, and thrombogenic catheter materials are the main reasons that TE develop [85, 86]. The exact incidence of CVC-related TE varies but recent reports have ranged from 0.7% to 67% [19, 87, 88].
The majority of CVCs placed in neonates include umbilical venous catheters (UVCs) and peripherally inserted central venous catheters (PICCs) [85]. Autopsy studies have estimated that 20%–65% of infants who die with a UVC in situ have microscopic evidence of TE [16, 89, 90]. Intracardiac TE from UVC placement ranges from 1.8% to 5.3% [85].
Persistent infection and/or thrombocytopenia, line dysfunction, and bilateral lower limb edema should alert the clinician of a possible UVC-related TE [91]. Most centers remove UVCs within 7 days of placement, but they should always be removed by 14 days [92]. PICCs or surgically placed CVCs tend to remain in place for weeks until antibiotic treatment is completed, or an infant has reached adequate enteral feedings. Signs of either PICC or CVC-related TE include unilateral limb swelling/pain/discoloration, superior vena cava syndrome, chylothorax, chylopericardium, intracardiac thrombosis, persistently positive blood cultures, thrombocytopenia, and cardiac failure [21, 93, 94].
Evaluation for CVC-related TE should start with Doppler US but false negative results can occur due to obstruction of the distal subclavian veins by the clavicles [18].
Intracardiac TE and TE in Infants with Complex Congenital Heart Disease
A major complication of a CVC in neonates is the development of a right atrial TE. This type of TE has been associated with endocarditis, pulmonary arterial obstruction, ventricular dysfunction, and death [5, 95–97]. Right atrial and other types of intracardiac thrombi have also been reported commonly in neonates undergoing repair for complex congenital heart disease [98]. Reviews of neonates who underwent palliative repair found evidence of thrombi in 23%–33%, whereas a more recent case-control study performed at a high-level referral NICU demonstrated an incidence of intracardiac TE of 22.5 cases per 1,000 admissions [99] [95].
Echocardiography is the preferred modality for diagnosing either right atrial TE formation, intracardiac vegetations, or TE formation in infants with single ventricle physiology. Signs suggestive of an atrial TE include new onset murmur, sepsis, persistent thrombocytopenia, and cardiac failure.
Renal Vein Thrombosis (RVT)
The most prevalent noncatheter-related TE during the neonatal period, RVT has an incidence of about 0.5 per 1,000 NICU admissions [5]. Recent reviews have demonstrated that about 70% of cases are unilateral, with 64% of these involving the left kidney and a male predominance [100–102]. The cardinal signs suggesting RVT are macroscopic hematuria, a palpable abdominal mass, and thrombocytopenia. Other symptoms include oliguria, proteinuria, acute renal failure, and hypertension. Risk factors are frequently found in RVT cases, with prematurity and perinatal asphyxia being the most common [100]. Because of the potential association of an IT and RVT, an evaluation for an IT is warranted. Doppler US is the modality of choice for diagnosing RVT in neonates with radiographic criteria including presence of echogenic clot, venous distension secondary to presence of a thrombus, or absence of flow [100].
Complications of RVT include adrenal hemorrhage, extension of the clot into the IVC, renal failure, hypertension, and death [101]. Survival is currently at around 85%, however, renal atrophy did not seem to change whether supportive care or anticoagulation/fibrinolysis were used, suggesting that many of these events may be in utero and chronic in nature [100].
Portal Vein Thrombosis (PVT)
Sepsis/oomphalitis and UVC use represent the two major risk factors for PVT [103]. Diagnosis may be difficult since most cases are clinically silent. Doppler US is the preferred modality for evaluation. Cavernous transformation of the portal vein with subsequent splenomegaly and reversal of portal flow are used to document severity [103]. Although spontaneous resolution of asymptomatic PVT in neonates is common, detection of PVT warrants close observation to follow for signs of portal hypertension. This complication may manifest itself up to 10 years after the neonatal period [103].
Cerebral Sinovenous Thrombosis (CSVT)
A subcategory of perinatal stroke, CSVT symptoms are similar to PAIS [104, 105]. Other clinical findings may include anemia and/or thrombocytopenia. Predisposing risk factors are common, with infection, perinatal complications, and IT being the most frequently reported [105]. The superficial and lateral sinuses are the most frequently involved vessels, and up to 30% of cases have reported venous infarction with subsequent hemorrhage [23, 106]. Intraventricular hemorrhages (especially in term neonates) and hemorrhages within the caudate nucleus and thalamus are associated with thrombosis of the deep cerebral venous sinuses. Therefore, the presence of an intraventricular hemorrhage or thalamic hemorrhage in a term or late preterm infant warrants evaluation for CSVT [106]. Diagnosis of CSVT is best made through diffusion MRI with venography [21, 30, 91, 107]. Mortality rates for neonatal CSVT range from 2% to 24%, with long-term complications consisting of cerebral palsy, epilepsy, and cognitive impairments in 10%–80% of infants [108–110].
Management
General Information
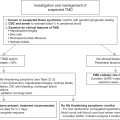
When possible, neonates with TE should be managed under the care of an experienced pediatric hematologist or neonatologist with pediatric hematology consultation at tertiary care centers with appropriate radiologic, pharmacologic, surgical, and laboratory support [111]. Management is based on the type of TE, location, severity, and risk factors. Most neonatal TE are managed with therapeutic anticoagulation, but there are situations where active monitoring for thrombus extension without anticoagulation therapy is appropriate, as studies have demonstrated spontaneous resolution of TE in up to 50% of asymptomatic neonates with UVCs [88, 112–114]. In addition, the smaller the thrombus, the more likely it will spontaneously resolve [114]. Therefore, certain neonatal TE can be monitored closely with serial US investigations, with the intent to initiate anticoagulation should the TE increase in size or become symptomatic. The duration and type of therapy depends on the location and size of the TE. The complexity in the decision of when and how long to treat neonatal TE reinforces the notion that the care should be managed under the guidance of experienced providers [111]. Long-term complications such as post-thrombotic syndrome may develop as a result of a catheter-related thrombosis from 1 month to up to 10 years following the event [115].
Arterial TE
Current guidelines recommend anticoagulation for PAIS if there is an ongoing cardioembolic source or evidence of recurrent PAIS [91, 116]. Arterial catheters should be immediately removed whenever there is suspicion or confirmation of a TE [91]. If vascular spasm occurs, removal of the catheter may alleviate symptoms. If spasm persists, warming of the contralateral extremity for 15 minutes may resolve symptoms. However, persistent symptoms may require the local application of 2% nitroglycerin ointment at 4 mm/kg with close monitoring of blood pressure [117]. Management options for neonates with arterial TE include therapeutic anticoagulation or potentially thrombolytic therapy (see Table 19.3).
Table 19.3 Management of neonatal arterial TE
| Type | Severity | Treatment |
|---|---|---|
| Femoral arterial catheter related | Non-limb threatening | Anticoagulation |
| Limb or organ threatening | Anticoagulation but change to thrombolytic therapy if clot does not improve or symptoms worsen within 24–48 hours | |
| PAL related | Non-limb threatening | Anticoagulation |
| Limb threatening | Thrombolytic therapy followed by anticoagulation | |
| Spontaneous or UAC related | Non-limb or organ threatening | Anticoagulation |
| Limb or organ threatening | Thrombolytic therapy followed by anticoagulation |
Venous TE
Many neonatal TE will be found in association with a CVC. Prior to removing any CVC, including UVCs, that has an associated VTE, it is recommended that 3–5 days of therapeutic anticoagulation be administered to prevent emboli [111]. Currently, most neonatal CVC-associated VTE are treated with therapeutic anticoagulation with thrombolysis reserved for life or limb threatening VTE. Current management strategies are extrapolated from adult data, but the optimal management neonatal CVC-associated VTE is currently being evaluated in the Netherlands [87]. Depending on risk categories, CVC-associated VTE will be managed with either thrombolysis followed by therapeutic anticoagulation, therapeutic anticoagulation alone, or close observation. This will be one of the first studies evaluating treatment options specifically in this population and it will provide a unified, national approach to neonatal thromboses as all NICUs in the Netherlands will follow this protocol [87]. Thrombolytics and/or anticoagulation should also be used for neonates with infective endocarditis that is resistant to antibiotic therapy alone and should be based on the size and symptoms of the TE [118].
Treatment guidelines for RVT (Table 19.4) and PVT (Table 19.5) are provided. There are currently no evidence-based neonatal PVT treatment guidelines due to insufficient data, thus treatment for each neonate should be individualized [103]. Also, there is no evidence to suggest that anticoagulation would improve outcomes, primarily reducing rate of portal hypertension. Due to the lack of evidence, avoidance of anticoagulation if possible is the guiding principle, but if anticoagulation in initiated, duration of therapy should be as short as possible [103].
| Unilateral RVT | Bilateral RVT | |
|---|---|---|
| Absence of renal impairment and/or no extension into the inferior vena cava |
| Anticoagulation |
| Extension into the inferior vena cava or presence of renal impairment | Anticoagulation* | Anticoagulation* |
| Renal failure | N/A | Initial thrombolytic therapy with rt-TPA*, followed by anticoagulation |
| Treatment plan | Description | Recommended ultrasound (US) follow-up |
|---|---|---|
| Observation | Non-occlusive thrombus and no evidence of portal hypertension | 2–3 days |
| Anticoagulation* | Occlusive thrombus or idiopathic | 10 days |
| If thrombus resolved, may stop therapy. If still present, treat for 6 weeks to 3 months depending on US follow up | ||
| Thrombolysis* | End-organ compromise with extension of the thrombosis into the IVC, RA, and/or RV | Daily |
| May stop thrombolysis when symptoms improve but would transition to anticoagulation for 6 weeks to 3 months |
Notes: IVC, inferior vena cava; RA, right atrium; RV, right ventricle
*For dosing options, please see Tables 19.7–19.10.
Data from Ref. [111].
Adapted from Williams S, Chan AK. Neonatal portal vein thrombosis: Diagnosis and management. Semin Fetal Neonatal Med 2011;16:337; with permission.
A systematic review of anticoagulation for CSVT in neonates demonstrated that anticoagulation did reduce the risk of thrombus propagation, but did not have a significant effect on mortality before discharge either in the presence or absence of pre-existing intracranial hemorrhage (ICH) [111, 119]. Current recommendations are to initiate anticoagulation in the presence of CSVT. Risk vs. benefit must be taken into account if acute hemorrhage is present. Anticoagulation should be continued for 6 weeks with repeat imaging at that time. Surgery is reserved for those with hydrocephalus or large intracerebral hematomas with mass effect.
Anticoagulation Therapy with Heparins
Treatment guidelines for anticoagulant dosing regimens for neonates are extrapolated from adult and pediatric data since there are no randomized controlled trials, which at this point will likely never be completed due to the risk of withholding this therapy [111, 117]. This is disappointing as the significant differences in the coagulation system of neonates make it difficult to assess the true risk for serious complications, specifically intracranial hemorrhage (ICH), which is potentially increased even more in premature infants. The presence of certain clinical factors, including recent central nervous system surgery, active bleeding, recent seizure activity, or significant coagulopathy, need to be considered in this especially at risk population as they can affect the initiation of anticoagulant therapy as well as the type of therapy selected [15]. Family discussions highlighting the risks and goals for treatment must be documented prior to initiating any therapy. Before initiating any treatment, absolute and relative contraindications to antithrombotic therapy should be reviewed (Table 19.6).
Table 19.6 Contraindications for anticoagulation/thrombolysis
| Absolute | Relative | |
|---|---|---|
| Medical conditions | 1. CNS surgery or ischemia (including birth asphyxia) within 10 days | 1. Platelet count < 50 × 104/microliter (100 × 104/microliter for ill neonates) |
| 2. Active bleeding | 2. Fibrinogen concentration <100 mg/dL | |
| 3. Invasive procedures within 3 days | 3. INR > 2 | |
| 4. Seizures within 48 hours | 4. Severe coagulation deficiency | |
| 5. Hypertension |
Notes: CNS, central nervous system; INR, international normalized ratio.
Adapted from Manco-Johnson. Controversies in neonatal thrombotic disorders. In Ohls RY, ed. Hematology, Immunology and Infectious Disease: Neonatology Questions and Controversies (Philadelphia, PA: Saunders Elsevier, 2008), p. 68; with permission [24].
Heparin anticoagulants require antithrombin (AT) to achieve their therapeutic effect. Antithrombin baseline levels are lower in neonates compared with children and adults and neonates clear heparin at an increased rate, thus neonatal dosing may be at higher levels than adult recommended dosing in order to attain therapeutic levels [15]. In rare cases, significant difficulty obtaining therapeutic heparin levels may occur and monitoring AT activity may be recommended with administration of AT concentrate. If AT is administered, close monitoring of heparin levels is required as supratherapeutic anticoagulant levels can be obtained which would increase the risk of bleeding complications. This is not frequently recommended and should only take place with pediatric hematology assistance.
Low molecular weight heparin (LMWH) is a commonly used anticoagulant in infants and children that selectively inhibits activated factor X (FXa), with enoxaparin utilized most frequently [3, 120–122]. Clinical trials have shown that LMWH generally has fewer bleeding complications than unfractionated heparin (UFH), has a longer half-life, and has a consistent pharmacokinetic and pharmacodynamic profile [123, 124]. LMWH therapy has been effective in the NICU with centers reporting either partial or complete resolution of TE events in 59%–100% of neonates treated [125, 126]. Initial dosing guidelines are based on gestational age (Table 19.7), followed by close monitoring with adjustments as needed to maintain a therapeutic LMWH anti-Xa assay level of 0.5–1 units/mL (Table 19.8). Maintaining therapeutic levels in neonates may be a challenge [111]. A recent review evaluating enoxaparin use in 240 neonates found that the mean maintenance dose of enoxaparin ranged from 1.48 to 2.27 mg/kg q 12 h for all infants, but was higher for preterm neonates at 1.9 to 2.27 mg/kg q 12 h [125, 126]. These findings have influenced the current recommended dosing (Table 19.7).