CARDIOPULMONARY AND CARDIOVASCULAR CONSIDERATIONS
PEARLS
❖ Cardiovascular disease is the major cause of death after age 65, accounting for over 40% of deaths in this population.
❖ Prolonged inactivity and bed rest quickly and markedly impair cardiovascular functional capacity.
❖ Cardiopulmonary and cardiovascular changes related to aging include decreases in aerobic capacity, vital capacity, minute volume, maximum cardiac output, maximal obtainable heart rate, stroke volume, and maximal oxygen consumption and an increase in blood pressure.
❖ The outcomes of aging on the pulmonary system are an increased mechanical workload for breathing, a decrease in the efficiency of gas exchange, and a compromise in the ability to efficiently supply oxygen to peripheral tissues.
❖ Submaximal stress testing can be done safely for older persons. The various types of tests (step test, modified chair step test, walking test, treadmill testing, and cycle ergometer testing) are all useful for evaluating cardiovascular status in older adults.
❖ Intensity, duration, and frequency—the 3 major components of exercise prescription—are different for older adults. Intensity is safe at 60%; duration, which is usually 20 minutes, may need to be cut to 4 to 5 minutes initially; and frequency should be daily.
❖ When pr escribing exercise for older persons, special considerations and modifications should be made for those with pacemakers or on cardiopulmonary medications and patients with certain diseases.
Cardiopulmonary considerations are particularly important in treating the older population in geriatric rehabilitation settings. Diseases of the heart, lungs, and blood vessels are by far the most prominent causes of morbidity and mortality among older individuals, rising logarithmically with age.1,2 As the number of older individuals at risk for cardiovascular disease (CVD) continues to rise and as successful medical treatments for ischemic and hypertensive diseases in the middle-aged population drive up the number of people with known diseases surviving into older age, health care providers will be managing increasing numbers of older individuals with cardiopulmonary and CVD. Eventually, the process of aging and inactivity takes its toll on the cardiovascular and cardiopulmonary systems and compromises each individual’s ability to meet the oxygen demands of activity beyond the resting state.3
This chapter covers the cardiopulmonary and cardiovascular changes associated with aging and the physiological aspects of exercise associated with improving cardiopulmonary and cardiovascular health. Evaluation techniques specific to a frailer older population are covered, and special considerations when prescribing exercises for people with diseases are presented.
INCIDENCE OF CARDIOPULMONARY AND CARDIOVASCULAR DISEASE
The projected shift in the age distribution of the population, as described in Chapter 1 of this text, indicates that older individuals comprise an increasing proportion until the middle of the next century, when those 65 years of age and older will constitute about one-fifth of the total population. Currently, 15% of the population in the United States are 65 years of age and older.4 Of these, 50% of them have some form of cardiopulmonary or cardiovascular disorders. Indeed, CVD is the major cause of death after the age of 65, accounting for over 40% of deaths in this age group.5 CVD presents a great burden for older patients, their caregivers, and health systems. Structural and functional alterations of vessels accumulate throughout life, culminating in an increased risk of developing CVD. The growing older population worldwide highlights the need to understand how aging promotes CVD in order to develop new strategies to confront this challenge. Although deaths from CVDs have shown a slight decline in concert with a decrease in heart disease since 1990, the leading cause of death among persons age 65 or older continues to be heart disease.6 Older adults reported significant health impairments related to heart, lung, and vascular conditions, including angina, congestive heart failure (CHF), rhythm disturbances, chronic obstructive and restrictive lung diseases, and peripheral vascular disease.1,2,6 Clinical observation also reveals a substantial decline in functional ability and an increased need for health care and assistance as a result of cardiovascular compromises.
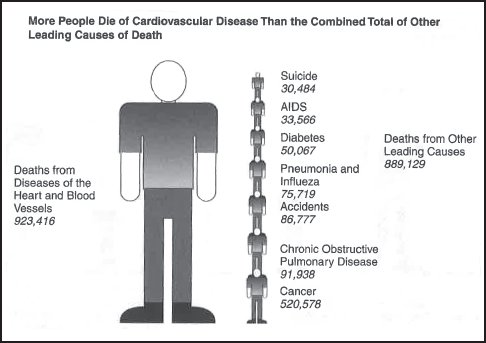
Figure 13-1. A comparison of deaths from cardiovascular disease to other leading causes of death. (Reprinted from the American Heart Association and Healthy Choice Foods, 1998.)
The majority of US residents receiving cardiovascular services are believed to be Medicare beneficiaries, and the age-associated increase in prevalence and incidence is true for all forms of CVD and cardiopulmonary disease (except congenital). Although women are often thought to be at lower risk for CVD, this relative immunity represents only a 7- to 10-year delay in onset. In fact, as age increases, prevalence rates become more equal with those of men, and ultimately cardiovascular mortality rates in women and men are equivalent.7 More people in the US population, as a whole, die of CVD than the combined total of other leading causes of death (Figure 13-1). As Figure 13-1 depicts, CVD tops the list of the 10 leading causes of death in the United States and annually kills more Americans than all the other diseases combined, including cancer, diabetes, AIDS, and suicide. One in 4 Americans, nearly 59 million, suffers from CVD. The American Heart Association estimates that the cost per year in health care and lost productivity is approximately $138 billion, which represents about one-seventh of the total health bill. As CVD does not start in old age (ie, after the age of 65), preventive measures must be addressed throughout the life cycle.
Implications
In the research by Chen and Sloan,8 disability generally was found to stay the same or increase as an individual aged. Increased trends were more apparent for near-elderly than elderly persons. Sociodemographic shifts tended to reduce disability, but their favorable effects were largely offset by increased self-reported chronic disease prevalence. Changes in smoking and heavy drinking prevalence had relatively minor effects on disability trends. Increased obesity rates generated sizable effects on lower body functioning changes. Disabling effects of self-reported chronic diseases often declined, and educational attainment became a stronger influence in preventing disability.8 The most frequently occurring problem is atherosclerotic heart disease. It is common to find hypertension coexisting with atherosclerotic heart disease. CHF, arrhythmias, and electrocardiographic abnormalities have an increased incidence with aging.8 Cardiac disease in older adults is complicated by the fact that it rarely occurs in isolation. Pulmonary problems, such as chronic obstructive pulmonary disease (COPD) and emphysema, usually result in death from the cardiac complications they impose, and vascular diseases generally accompany cardiac disease or predispose an individual to the development of cardiovascular and cardiopulmonary pathologies (see Chapter 5). Chronic inactivity, resulting from musculoskeletal or neuromuscular causes or systemic diseases, further exacerbates the effects of aging on the cardiovascular system. Deaths from CVD are only part of the story. The debilitating effects on individuals who survive a stroke or a heart attack lead to a loss in functional capabilities and severely impact the individual’s ability to maintain independence as depicted in Figure 13-2.
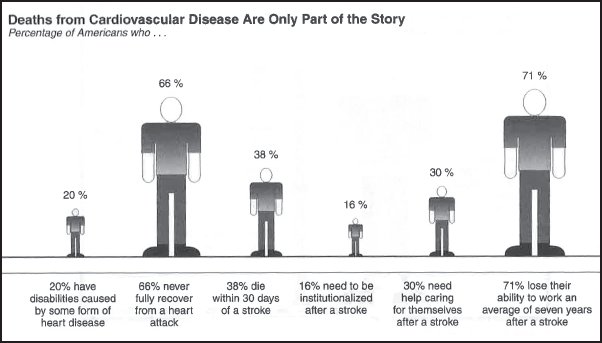
Figure 13-2. The debilitating effects of cardiovascular disease. (Reprinted from the American Heart Association and Healthy Choice Foods, 1998.)
Cardiac rehabilitation is a means of improving the cardiopulmonary response to increased oxygen demands during increased activity through endurance and conditioning exercises. The progression of the aging process eventually evolves into diseases in the cardiovascular and cardiopulmonary systems. Any of the pathologies mentioned previously will lead to an inhibition of the cardiopulmonary responses to increased oxygen demands. Functional level of activity decreases as a result of a vicious cycle of inactivity and deconditioning imposed by a variety of medical problems in the musculoskeletal, neuromuscular, and sensory systems that can cause cardiovascular disability or may exacerbate underlying cardiac disease.
Prolonged inactivity and bed rest quickly and markedly impair cardiovascular functional capacity.9–11 All too often deconditioning of the cardiopulmonary system is potentiated by excessive bed rest and overmedication for the older cardiac patient. Even prior to illness, many older patients decrease their activity level due to a varied combination of musculoskeletal and neuromuscular problems. Additionally, because of the decreased aerobic capacity with aging, any submaximal task is perceived as requiring increased work because of its increased relative energy cost and resulting fatigue. Thus, relative inactivity potentiates the decreased physical work capacity in older adults, often threatening the possibility of an independent lifestyle. This can be avoided, and indeed, functional capacity can be improved with conditioning and endurance exercises, and the reinstitution of the older person’s participation in functional activities of daily living.
There has been increased interest in research about the effects of exercise on the older cardiac patient.9–12 Perhaps this is a result of the growing numbers of older adults and changing demographic and sociologic patterns.6 Individuals are living relatively healthy lives well beyond the socially imposed demarcation line that defines old age.12,13 The expectations of acceptable levels of function for the older segment of the population have changed. Research studies have demonstrated that not only is exercise beneficial for maintaining a functional baseline condition in the unimpaired older individual, but it is also therapeutic for reversing the effects of impairment and improving baselines in individuals who have become deconditioned as a result of symptom limitations (eg, angina and dyspnea).11,14
American society’s increased focus on exercise and a corresponding broadening of the expectations among older adults for an active lifestyle have increased their participation in physical activity programs. As a result, it is important that physical therapists be involved with the development of clinical procedures that are safe and effective in exercise assessment and prescription for older adults. Therapeutic evaluation and program planning have now reached the point where the older adult, who was once confined to bed because of angina and dyspnea resulting from cardiopulmonary disease, can be evaluated and treated with a total rehabilitation program. This should include an individualized exercise prescription that considers the severity of disease, attempts symptom reversal, and has functional improvement as its primary goal. Cardiopulmonary considerations are important in the geriatric population for the prescription of any activity because cardiopulmonary pathological manifestations are most likely to accompany increasing age in close to 100% of the older population we see in the clinic.
PHYSIOLOGICAL ASPECTS OF EXERCISE
Human performance is a remarkable integration of all of the systems of the body. Practically no tissue or organ escapes involvement in increasing activity levels. While the muscles perform the work, the heart and peripheral vascular systems deliver the nutrients and, with the assistance of the pulmonary system, provide O2 to and remove CO2 from the working tissues. The nervous and endocrine systems integrate all of this activity into meaningful performance. At the cellular level, the mitochondria and numerous enzymes are activated, and energy is generated to enable the muscle to contract. Skin acts as the heating and cooling system as activity is prolonged, and the kidneys assist in maintaining a homeostatic fluid balance. It is apparent that any pathological manifestation involving any of the body systems will negatively influence the physiological response to exercise.9
The heart is an amazing organ. Despite its decreased power and ability to contract, slower rate of recovery, diminished cardiac reserve, and the other changes of aging and disease, the human heart continues to function well as long as it is not overwhelmed by disease. By the time a person is 80 to 90 years of age, the heart has long outperformed the best mechanical pumps devised by man. By the age of 100, the human heart has beat more than 3.6 billion times and pumped more than 288 billion cm3 blood. The ability of the cardiovascular and cardiopulmonary systems to respond to stress admittedly decreases with advancing age, but many older people, even with heart disease, can continue their normal routine activities well into older age.
During the normal life span, the cardiovascular and cardiopulmonary systems are subject to a variety of normal physiological stimuli and processes that may create pathological consequences. In addition, the biological changes of aging, beginning after the process of growth and development, the evolution of maturity and adulthood, and proceeding into the phases of senescence and old age, modify the anatomical, physiological, and functional capabilities of the heart, lungs, and vascular systems.
CARDIOPULMONARY CHANGES WITH AGING AND DISEASE
The changes in the cardiopulmonary system related to aging and disease have been discussed in Chapters 3 and 5, respectively, and are only summarized in this chapter as a foundation for cardiopulmonary treatment considerations in older adults.
There is some controversy over the degree of physiological change that is expressly age related as opposed to disease related. However, most investigators agree that certain changes in muscle strength and cardiac and pulmonary function are so common that they may be thought of as universal. Because rehabilitation exercise programs increase the level of activity above resting states, these changes are likely to affect the older person. Aerobic capacity (maximum oxygen consumption or VO2 max) decreases with advancing age,14 and declines in aerobic capacity are probably greater in the patient who has become deconditioned during a recent hospital stay or who had poor exercise habits prior to developing a disability. Exercise capacity may be further affected by decreases in vital capacity and minute volume.15 Additional cardiopulmonary changes related to aging include increased blood pressure and decreased maximum cardiac output (CO).11,14 Maximal obtainable heart rate and stroke volume decline in relation to the decrease in VO2 max.15 With age, lean muscle mass decreases as does muscle strength16 and is discussed in this chapter as it relates to the cardiopulmonary system’s need to meet working muscles’ energy demands. Orthostatic hypotension is frequently observed, particularly in those recently bedridden. Peripheral vascular resistance rises with age, increasing the risk of developing hypertensive episodes with exercise programs.
The heart demonstrates little change in the size of its chambers, but the left ventricular wall thickens and becomes less compliant.17 There is a thickening of or a development of nodular ridges along the attachments of the aortic cusps.18 The conduction system displays relatively little change in the atrioventricular node or the bundle of His although the number of proximal bundle fascicles connecting the left to the main bundle may be reduced.19
Coronary artery or ischemic heart disease is the most prevalent disease in individuals over the age of 60.13 In 90% to 95% of the cases, the reduction of blood flow to the heart is the result of atherosclerotic narrowing of the coronary lumen.17 This reduction in flow creates the manifestations of angina, myocardial infarction, and sudden death. Angina and infarction impair function by decreasing the maximum CO and VO2 max. Infarction or necrosis of the heart muscle limits the distensibility of the heart and reduces the stroke volume. Collectively, these pathological changes produce a self-limiting impediment to cardiac function. Increased systemic demands for oxygen necessitate an increase in CO or myocardial work. Increased work requires an increased supply of O2 to the myocardial muscle. The restricted coronary blood flow results in ischemia, which increases the left end-diastolic pressure, prolongs systole as the heart is unable to relax, and stiffens the ventricle wall. A destructive cycle is instituted as these physiological changes reduce perfusion of the myocardium and increase the degree of ischemia, further damaging cardiac tissue.14 The result of this vicious circle is progressive deconditioning of the heart as angina and dyspnea self-limit and impair functional activity and exercise capacity.
Lung changes are characterized by an increase in residual volume accompanied by a decrease in vital capacity. Declines are seen in maximal voluntary ventilation, the surface area for gas exchange, the rate of diffusion, and the arteriovenous oxygen differential.20 Both the lung tissue and chest wall lose elasticity. Cardiopulmonary demands usually can be met, but when disease or deconditioning is present, the demands may exceed the available reserve. All of these changes result in reduced tolerance for physical activity and are important to consider with regard to rate and intensity of activities for the older person. Due to the wide variety in lifestyles, the rate and magnitude of changes cannot be predicted and may not be apparent until they impact activities of daily living.
The anatomical and functional changes seen in COPD mimic those seen in aging. Both are characterized by microtraumas that occur over time, which do not interfere with resting or low-level ventilatory function.21,22 The pathological tissue changes seen with emphysema and chronic bronchitis are also similar to the tissue changes of advancing age. The degree of impairment is the distinguishing factor between what is considered “normal” aging and the degree of impairment and compromise that is considered pathological. In emphysema, there is an abnormal enlargement of the terminal airspaces as a result of a loss in tissue elasticity of the lung. This results in expiratory collapse of the larger airways. Expiration is difficult for the patient with emphysema. Chronic bronchitis is accompanied by a persistent productive cough on a daily basis. The result of these respiratory conditions is an increase in the work of breathing and an inability to meet the energy demands required for functional activities of living, exercise, or both.
Maximal Oxygen Consumption
The major function of the cardiovascular and cardiopulmonary systems during exercise is to deliver blood to the active tissues, supplying O2 and nutrients and removing metabolic waste products. If exercise is prolonged, the cardiovascular system also assists in maintaining body temperature.
The cardiac and pulmonary systems integrate a number of component functions in order to adequately acquire and distribute O2 to the working muscles. The muscles of the thorax contract to initiate an increase in thoracic volume and to lower the intrathoracic pressure. A decrease in the intrathoracic pressure creates gas flow from the higher-pressured atmosphere into the conducting tubules where the gas is warmed, filtered, humidified, and mixed with existing gases to produce an alveolar oxygen tension of 90 to 100 mm Hg.9 Alveolar oxygen is diffused across the 70 m2 blood-gas interface into pulmonary capillaries via an approximate 40 mm Hg pressure gradient where it combines with hemoglobin and then enters the left atrium. The heart, through rhythmic contraction, delivers the oxygenated blood to the myocardial muscle first and then to the peripheral tissues. The pressure created by the contraction of the heart (systolic) overcomes systemic pressure and generates blood flow through the arterial vascular system.
VO2 max is the best measure of cardiopulmonary fitness. It can be derived by the following simple equation: VO2 = Q × (aO2 – vO2). VO2 is the amount of oxygen the system absorbs and is equal to CO (Q) multiplied by the arterial oxygen content (aO2) minus the central venous oxygen content (vO2). Each link of this multistaged process needs to be adequately functioning in order for the system to efficiently acquire, transport, and deliver O2. An impairment at any phase as a result of disease, age, or deconditioning limits the amount of O2 uptake (VO2) and competent delivery to the working tissues.
Heart Rate
The resting heart rate is influenced by age, body position, the level of cardiopulmonary fitness, and various environmental factors (eg, temperature, humidity, and altitude). The resting heart rate remains relatively constant with age although in advanced age it may show a decline. Better cardiopulmonary fitness results in a decrease in the resting heart rate, whereas the resting heart rate will increase in higher environmental temperatures or at an increase in altitude.23
Before exercise, the heart rate may be increased by an anticipatory response, a reflection of a sympathetic neurohumoral effect. As exercise begins, the heart rate increases, but during low levels of exercise at a constant workload, the heart rate will attain a plateau or steady state. As workload increases, the heart rate increases in a roughly linear manner. At higher workloads, the heart rate takes longer to plateau. For the same workload, the more fit individual will have a lower steady-state value.
The older individual shows a lower response given the same workload but, at progressively higher workloads, will eventually reach a level that is totally exhausting. Prior to this, however, the heart rate will have reached a plateau at its maximum.
The maximum heart rate declines with age. Each individual has a definable maximum heart rate. The equation for maximum achievable heart rate is 220 – the person’s age. Figure 13-3 provides a worksheet for calculating aerobic and anaerobic training ranges. This provides an approximation of the mean maximal heart rate for any one age category with a standard deviation of 10, so this equation should be used cautiously. The decline in maximum heart rate with age has been attributed mainly to changes in the myocardial oxygen supply, but additional factors include pathological impairment of blood flow to the sinus node, producing a lower heart rate during maximal exercise (the “sick sinus” syndrome), and greater stiffness (reduced compliance) of the heart wall, which increases the time required for filling of the ventricles and interferes with the “feedback” of information on venous filling to the cardioregulatory center.23
Heart rate responses will vary at rest and submaximal exercise levels according to the degree of cardiovascular impairment, whereas the maximum achievable heart rate shows a progressive decline with age.9,23 Heart rate responses to physiological stimuli such as postural change and cough have also been shown to decrease with age.18 In an older, frailer population, it is not necessary to reach aerobic heart rate levels to gain improvements in cardiovascular health. Any activity above rest works! The importance of activity beyond the resting level cannot be emphasized enough in an older population.
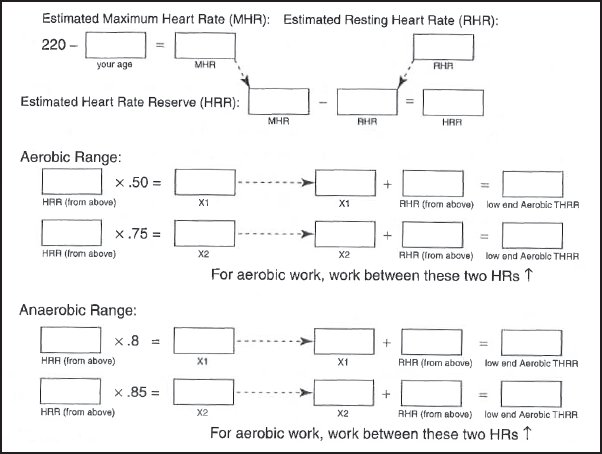
Figure 13-3. A worksheet for calculating aerobic and anaerobic training heart rate ranges (THRRs). Aerobic example: using 70 years of age with a resting heart rate (RHR) of 80. Maximum heart rate (MHR) = 220 – 80 = 140. Subtracting RHR from MHR, you get 140 – 80 = 60 for heart rate reserve (HRR). Aerobic THRR will lie between 50% and 75% of the HRR added to the RHR: 50% of 60 = 30 and 75% of 60 = 45. Adding these figures to the RHR gives the following: 80 + 30 = 110 and 80 + 45 = 125. Thus, the THRR would be 110 to 125 beats/min. Anaerobic example: to calculate anaerobic heart rate range, take 80% of 60 = 48 and 85% of 60 = 51. Adding these figures to the RHR gives 80 + 48 = 128 and 80 + 51 = 131. Thus, the anaerobic threshold THRR is 128 to 131 beats/min.
Stroke Volume
The difference between the end-diastolic and end-systolic blood volumes is the stroke volume. The stroke volume response is highly dependent on hydrostatic pressure effects. When sitting or standing, without exercise, the stroke volume is reduced relative to the supine position due to blood pooling in the extremities. The maximum stroke volume attained during exercise in the supine or sitting position is only slightly higher. The increase is sufficient to overcome the effect of venous pooling. Stroke volume at rest in the erect position varies between 50 and 80 mL. In a highly trained athlete, this volume can be as high as 200 mL. The stroke volume increases linearly with the workload until it reaches its maximum at approximately 50% of the individual’s capacity for exercise.9
There is some controversy as to whether there is a change in stroke volume with age or if the changes are a result of a decline in VO2 max, a slower maximum heart rate response, and an increased peripheral resistance that diminishes the ejection fraction.24 Understanding the significance of stroke volume changes has been hampered to some extent by the inability to accurately measure absolute left ventricular dimensions (ie, end-diastolic and end-systolic volumes).25 Studies have suggested that there is no age-related change in stroke volume at rest26 and that the ejection fraction remains unchanged with age at rest.27 During exercise, end-diastolic volume and end-systolic volume showed marked age-related increases as higher levels of exercise were achieved according to a study by Rodeheffer and associates.28 Older participants showed an increase in end-diastolic volume at low levels of exercise and continued to show progressive increases with increasing exercise intensity. End-systolic volume in older participants also increased with exercise although less dramatically. Younger participants at high levels of exercise showed no change in the end-diastolic volume from resting levels, while the end-systolic volume decreased significantly. The implication of these volume changes is that the young population maintains CO by achieving a high heart rate and that healthy older individuals maintain CO by dilating the ventricle and using the Frank-Starling mechanism to increase stroke volume.28
Cardiac Output
The CO at rest is 4 to 6 L/min. It increases linearly with workload. At exercise levels of 40% to 60%, the increase in CO is accomplished through an increase in both the heart rate and the stroke volume. At higher levels of exercise, the increase in CO results solely from the continued increase in heart rate. Maximal values of CO during exercise are dependent on many factors. Body size and the degree of physical fitness appear to have the most prominent influence on CO. For instance, in a small, deconditioned individual, the maximum CO during exercise could be as little as 20 L/min, whereas in a large, well-conditioned individual, the CO can reach 40 L/min.14,23
Physiological changes in the cardiovascular system primarily involve the determinants of CO. CO is affected by preload and afterload conditions, which are altered by aging. Early diastolic filling is decreased as a result of mitral valve thickening and/or the decrease in the compliance of the left ventricle.19 There is an increase in afterload with aging as well. This is possibly produced by an increase in the rigidity of the ascending aorta and a general decrease in the diameter of the peripheral vascular system. This combination of factors increases the overall load on the myocardium and is responsible for the age-associated decrease in CO.
Blood Pressure
The normal response of the blood pressure is a linear increase in systolic pressure with increasing work (200 mm Hg or higher). Blood pressure changes in older individuals are dependent on many factors, including extracellular fluid volume, vascular tone and reactivity, the autonomic nervous system, and the arterial baroreceptor reflexes. Each component factor can affect responsiveness in the older adult somewhat differently. Resting systolic and diastolic blood pressures tend to rise with age; however, the range is quite variable.19,23 Diastolic blood pressure changes little in healthy older individuals. An increase in systemic blood pressure with age is related to the loss of elasticity in the walls of the larger arteries, which raises systolic and depresses diastolic pressures. There is also the increased liability of vasopressor control, which tends to raise both systolic and diastolic pressures. As a result, the systolic arterial blood pressure rises progressively up to the age of 75, and the diastolic pressure rises slightly to the age of 60 and then gradually declines.29
Arteriovenous Oxygen Differential
The arteriovenous oxygen difference is the difference between O2 in the arteries compared to the O2 content in the veins. It reflects the amount of O2 that the peripheral tissues extract. The maximum arteriovenous oxygen difference tends to decrease with age.30 Sh epard3 suggests that factors contributing to this decline with age include lower levels of physical fitness, a reduction of arterial oxygen saturation, a decreased hemoglobin level, poor peripheral blood distribution, a loss of activity in tissue enzyme systems, and a greater relative blood flow to the skin.
The arteriovenous oxygen difference tends to be larger in older adults compared to young adults both at rest and at submaximal exercise levels, indicating that there is a decrease in the amount of O2 extracted in older individuals.31 Some increase in the stroke volume in combination with a decrease in mechanical efficiency of the cardiopulmonary and cardiovascular systems could explain this. Horvath and Borgia32 report that there is no reduction in the amount of O2 saturation/transport capacity of arterial blood. The metabolic potential of skeletal muscle does not decline33; however, there is a decrease in the capillary/fiber ratio in the older muscle34 and a reduction in the amount of blood that flows to the periphery.35
Peripheral Vascular Resistance
Blood flow from the heart varies with tissue needs. During exercise, blood is shunted from areas of little or no metabolic activity (eg, the gut) to those tissues that are involved in the exercise. Blood to the heart increases proportionally to the increase in metabolic activity.9 Blood to the skin and muscles is increased, and blood to the stomach and intestines is decreased. The effective blood volume decreases from maximal levels with prolonged work and in a hot and humid environment because of the increased blood flow to the periphery that promotes both metabolic and environmental heat loss.14
Vascular changes of age affect each tissue layer differently. The cells of the intima become irregularly aligned instead of orienting themselves along the longitudinal axis of the vessel.19 The subendothelial layer becomes thickened due to lipid deposition, calcification, and increased cross-linking of the connective tissue. The media demonstrates increased calcification and fraying of the elastic fibers. These changes all lead to regional differences in vessel diameter and an increase in the resistance to blood flow.
The peripheral vascular resistance may be increased by atheromatous plaques in the lumina and with a loss in vessel elasticity and a failure to vasodilate in response to increasing activity. Regular exercise can reduce the resting systemic pressure by about 5 mm Hg, but it has little influence on the peripheral pressure during maximum effort.36
Neurohumoral Factors
There is a decline in the neurohumoral controls with aging, which reduces the ability to adjust to external and internal stresses.14 The body hormones contribute to the regulation of circulating fluid volumes and cardiovascular performance. They also mobilize blood glucose, liberate fat, and break down protein to provide energy for increasing activity levels. Neurohumoral factors are important in tissue repair because they are involved with the synthesis of new protein (anabolism), which is important in the healing process at the cellular level.
Fluid loss in prolonged exercise results in a decrease in plasma volume, hemoconcentration of red blood cells, and plasma proteins. This hemoconcentration results in an increase in red blood cells by 20% to 25%, and there is a shift of fluid from the plasma to the interstitial fluid.14
The blood pH shows little change up to approximately 50% intensity of exercise. Past 50%, the pH decreases, and the blood becomes more acidic. This decrease in pH is primarily the result of an increase in anaerobic muscle metabolism and corresponds to an increase in blood lactate.
Neurohumoral regulatory changes affect the physiological response of the older adult. Catecholamines function to maintain the systemic pressure, mobilize muscle glycogen to sustain plasma glucose, liberate fatty acids, stimulate gluconeogenesis in the liver, stimulate glucagon secretion, and inhibit insulin secretion.14 Although there may be an increase in plasma catecholamine levels with advancing age,37 there is a decrease in the end-organ responsiveness to beta-adrenergic stimulation.19 This variation in circulating catecholamines or decrease in neuroresponsiveness may partially account for the decreased heart rate and blood pressure response to activities such as a cough or Valsalva maneuver. This attenuated responsiveness is also partly attributed to decreased baroreceptor sensitivity.37
PULMONARY RESPONSE TO EXERCISE
Pulmonary ventilation or minute volume increases from approximately 6 L/min at rest to above 100 L/min during maximal exercise, and in a well-conditioned individual, this can exceed 200 L/min. This is accomplished by an increase in both tidal volume and respiratory frequency. Tidal volume at rest is about 0.5 L/min and can increase to 2.5 to 3.0 L/min during maximal exercise efforts. Resting respiratory frequency ranges from 12 to 16 breaths/min and increases to 40 to 50 breaths/min during maximal exercise.9
The respiratory system is responsible for ventilation through the coordinated contraction of the diaphragm and associated ventilatory muscles, the displacement of the rib cage, and the expansion of the lungs by the negative pressure created by the contraction of these muscles. The resting length and strength of the ventilatory muscles, the thoracic cage compliance, and the compliance of the lungs are important factors in generating adequate gas flow. Aging produces a progressive decrease in the thoracic wall and bronchiolar compliance.38 Because of structural changes in bone, cartilage, and elastic structures with age, the chest wall becomes stiff. There is an increase in cross-linking of collagen fibers, a decrease in the resiliency of elastic and cartilaginous tissue, and a decrease in collagen and annulus fibrosis.14,36 The elastic fibers within the lung change so that there is an increase in compliance of the lung, but a decrease in its elastic recoil.39 Superimposed on a decreased compliance of the thoracic wall, this results in a decrease in total lung compliance with age. There is an increase in the size and number of alveolar fenestrae40 that, in combination with the change in elastic features at the alveolar levels and the loss of tissue from the alveolar walls and septa, results in a decrease in the surface area available for gas exchange. The conducting tubules become more rigid, decreasing their radius and increasing resistance to gas flow.36 The result is an increased mechanical workload for breathing and a decrease in the efficiency of gas exchange.
The pulmonary systemic changes produced by pathological lung changes as those seen in COPD, emphysema, and chronic bronchitis increase the work of breathing and decrease the energy supply available to working muscles. There is a reduction in vital capacity due to an increased residual volume, a decreased forced expiratory volume, and a reduced arterial oxygen tension with an increase in the carbon dioxide tension.3,14 In combination with a decrease in thoracic compliance and progressive narrowing of the airways, the force required for the ventilatory muscles to create airflow severely stresses the cardiopulmonary system and compromises the ability to efficiently supply O2 to peripheral tissues.41
BENEFITS OF EXERCISE TRAINING IN OLDER ADULTS
Cardiac, vascular, and pulmonary diseases need not be a barrier to better fitness. Too many health care professionals working with older adults have set their sights low by accepting as normal the reduced ability of aging people who are inactive, sedentary, or incapacitated by subclinical or clinical disease. For instance, a decline in CO is considered a normal process in aging; however, according to noninvasive studies with radioactive thallium nuclear and echocardiographic studies, a decline in CO is absent in physically fit older people without occult coronary artery disease.28 Most studies dealing with changes in the cardiopulmonary response to exercise include more sedentary and less physically fit older individuals who may very likely have subclinical cardiopulmonary disease or CVD.
There are limited studies on the role of exercise in the prevention of coronary and pulmonary problems in the older population. However, epidemiologic studies suggest the clear role that increased activities (exercise, occupational, recreational, and leisure) play in decreasing the risk of developing CVD and cardiopulmonary disease.9,10,23,42,43 A lack of exercise progressively becomes a more important risk factor in the development of cardiopulmonary and cardiovascular pathologies.10,11,42–44 The relative body weight has less influence on the chances of developing a fatal heart attack.45 This may reflect the confounding influence of an increasing loss of lean tissue.
BENEFITS OF EXERCISE FOR PERIPHERAL VASCULAR CIRCULATION
Peripheral vascular disease results in increased peripheral vascular resistance due to narrowing and loss of elasticity in the vessel walls. Peripheral arterial insufficiency is present in most older individuals in varying degrees.
Figure 13-4. The Buerger-Allen protocol: horizontal position. Lying flat on back in rest position, pump and circle feet to facilitate circulation. Position maintained for at least 3 minutes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








