PEARLS
❖ The healing process can easily be remembered by the 3 Rs of wound healing: reaction (inflammation), regeneration (proliferation and epithelialization), and remodeling.
❖ The effects of aging and age-associated diseases slow the wound healing process.
❖ Thinning and flattening of the epidermis result in an increased vulnerability to trauma from shear and frictional forces in the older adult.
❖ Inadequate blood supply can result in poor oxidative and nutritive status in the tissues and lead to an arterial ulcer, and venous ulcerations are caused by venous hypertension and valvular incompetence and are generally accompanied by a history of deep vein thrombosis.
❖ All pressure ulcers are preventable if attention is directed to insensate areas, malnutrition, skin fragility, and the physical or cognitive inability to accomplish pressure relief without guidance or assistance.
❖ Treatment approaches for wound healing in the older population include physical modalities, debridement, incontinence care, topical dressings, and nutritional interventions.
Older adults are often predisposed to wounds because of poor hydration and nutrition, poor circulation, and inactivity. Skin breakdown can be prevented through proper seating and positioning. Given the right circumstances, older individuals with wounds also heal well, despite age-related problems and nutritional deficiencies.
This chapter focuses on skin and wound care in the older patient. From a geriatric rehabilitation perspective, positioning, seating devices and mattresses, and a focus on the prevention of skin breakdown are important components of therapy. Often, in an older population, we encounter wounds that are chronic and slow to heal. The aging of the skin, nutritional status, and hydration, in addition to immobility, will impact the integrity of the external integumentary system. Integumentary conditions that therapists treat are discussed followed by an appraisal of how a wound repairs itself and what complicating factors in the healing process exist in an older individual. Evaluation, staging of a wound, and documentation are discussed. The importance of nutrition and hydration in maintaining skin health and the importance of their role in healing are presented. The types of ulcers, venous, arterial, and diabetic, are reviewed because they impact treatment approaches. Other types of wounds seen in older adults, such as extravasation sites, abrasions and skin tears, dehisced surgical wounds, fistulas, and radiation burns, are discussed. Finally, a review of treatment modalities for wound management, surgical indications, and wound care products is presented.
There are natural delays in the healing of wounds of older individuals.1 Open wounds contract more slowly, and incised wounds gain strength more slowly. Experimental studies indicate that cellular proliferation, wound metabolism, and collagen remodeling occur at a delayed rate in older people.1,2
DEFINING INTEGUMENTARY CONDITIONS
Integumentary problems involve any covering or lining of the body. Therefore, the topic of integumentary system conditions could potentially cover skin and wound care to gastrointestinal conditions such as diverticulosis, constipation, or gastric ulceration and respiratory conditions such as tuberculosis. Although the status of these systems impacts the functional status of our older patients and may be affected by exercise, positioning, nutrition, and hydration, physical or occupational therapists primarily treat integumentary problems affecting the external covering of the body (eg, the skin). Despite this, it is important that the therapist not ignore the other integumentary conditions in assessing, evaluating, and treating the whole patient. It is vital that a therapist is cognizant of integumentary conditions that affect the gastrointestinal or respiratory systems and the influence these conditions might have on mobility and functional capabilities. These pathologies, when they exist, should be cared for as a part of an interdisciplinary team approach to patient care.
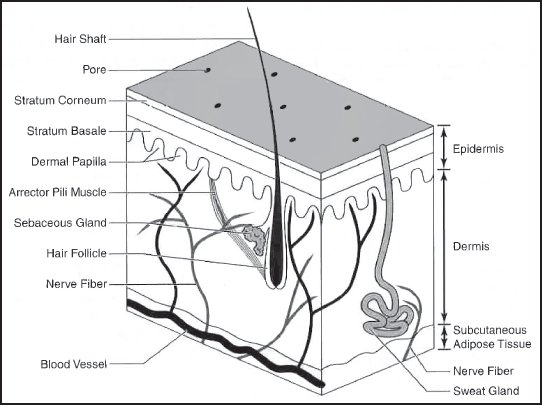
Figure 14-1. The structure of skin, including accessory structures. Hair with the follicles located deep in the dermis is shown with the associated arrector pili muscles that cause the hairs to become erect and form gooseflesh in the cold. Sweat glands with their coiled portion deep in the dermis and openings onto the surface of the skin are also depicted. Sebaceous glands are associated with hair follicles and secrete their oily sebum onto the skin to help retain moisture. Also note the relative thickness of the dermis, which is about 10 times thicker than the epidermis, the presence of sensory receptors in the dermis, and blood vessels in the dermis.
THE SKIN AND THE AGING PROCESS
It is well recognized that the skin of an older person differs in many ways from that of a younger person.2 While great variance exists among individuals’ physiologic responses to aging, certain characteristics are inherent to the aging process. In order to understand gerontodermatological changes and the effects they have on delayed wound healing, it is important to review what is normal so that the changes that take place can be put into perspective.
On average, there is approximately 20 square feet of skin (if laid out flat), and the skin is often called “the body’s biggest organ.” It is the only organ that is exposed to the external environment. It is an all-purpose covering in that it is waterproof (it keeps the water out and in), and it assists in regulating body temperature.
The skin has 3 distinct layers: the epidermis, dermis, and subcutaneous layers. Figure 14-1 provides a pictorial representation of the layers of normal skin. The epidermis is the uppermost layer of skin. This is divided into the stratum corneum (top layer), stratum spinosum (middle layer), and stratum germinativum (innermost layer). The stratum corneum, or the horny layer, is somewhat acidic and referred to as the acid mantle. It is the major barrier to the environment and effectively prevents the penetration of most environmental substances. The middle layer, or stratum spinosum, is called the prickle cell layer. This is the thickest of the epidermal layers. The cells in the stratum spinosum are squamous cells, which essentially are basal cells that have matured and migrated upward. The basal layer is the innermost layer of the epidermis and contains small, round cells called basal cells. The basal cells continually divide, and new cells constantly push older ones up toward the surface of the skin, where they are eventually shed. The basal cell layer is also known as the stratum germinativum due to the fact that it is constantly germinating (producing) new cells. The basal cell layer contains cells called melanocytes. Melanocytes produce the skin coloring or pigment known as melanin, which gives skin its tan or brown color and helps protect the deeper layers of the skin from the harmful effects of the sun.3
The dermis is the second layer. It contains collagen and elastic fibers, which are complex proteins responsible for the support and elasticity of skin. This layer enables the skin to regain its shape after being stretched or deformed. The circulatory supply is contained in the dermis, as well as the nerve endings, and the oil and sweat glands. Skin nutrition and oxygenation are supplied by numerous arteries, veins, and capillaries coursing upward through the dermis. Incredibly, each square inch of the dermis houses numerous small, nutrient-providing blood vessels. Their constriction and dilation, in response to ambient temperature changes, are responsible for keeping the body temperature constant. These small vessels also keep the skin healthy and viable by providing nutrients and remove metabolic waste materials (see Figure 14-1).
Table 14-1. Age-Related Changes in the Skin that Affect the Healing Process
CHANGE | RESULT |
| Thinning and flattening of epidermis |
|
| Decreased epidermal proliferation |
|
| Cells in horny layer become less elastic |
|
| Atrophy of the dermis |
|
| Decreased vascularity of the dermis |
|
| Changes and loss in collagen and elastin fibers |
|
| Decreased number of oil and sweat glands |
|
| Compromised vascular response |
|
| Nerve endings become abnormal |
|
| Fragility of the subcutaneous layer |
|
The subcutis or subcutaneous is the fatty layer, which gives the skin its smooth appearance. It is loosely connected to itself but adheres to the dermis and the underlying fascia. This allows skin to dissipate both pressure and shear forces. In areas where bony prominences such as the greater trochanter or heel are immediately adjacent to the subcutaneous fat layer without any muscle or other soft tissue protection, the ability of the skin to dissipate pressure is compromised. The disproportionate pressure placed on these areas can occlude blood flow, causing tissue breakdown and leading to tissue death. As well as mechanical protection, the subcutaneous layer also provides thermal insulation. Fat also acts as an energy store. By volume, fat stores approximately 20 times as much energy as the storage form of carbohydrate called glycogen.
As the skin ages, there are certain changes that occur that will ultimately impact the healing process in the event of an injury or wound. These changes are summarized in Table 14-1.
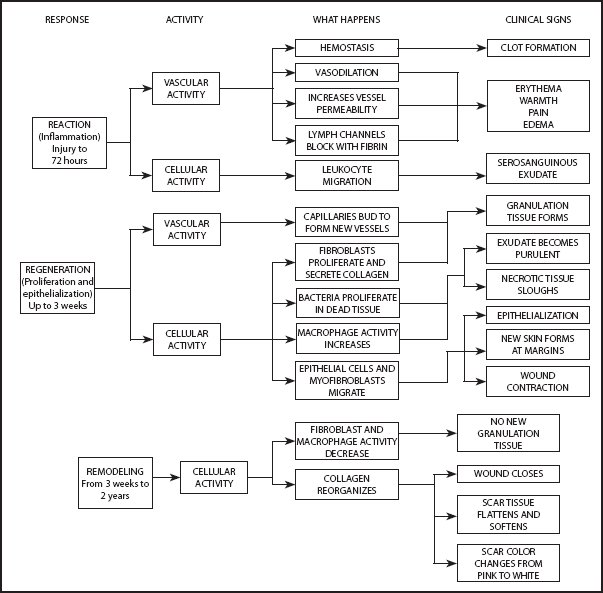
Figure 14-2. Wound healing process—the 3Rs: reaction, regeneration, and remodeling.
WOUND REPAIR
The body’s response to injury of the skin, the repair sequence, is the same regardless of the origin of the wound—whether it is a traumatic injury, a pressure sore, a venous stasis ulcer, or a diabetic ulcer. Wound repair starts the moment the tissue is injured. The healing process involves several predictable stages, which are summarized in Figure 14-2. Wound healing consists of 4 basic phases: inflammation, proliferation, epithelialization, and remodeling.4,5 This healing process can easily be remembered by the 3 Rs of wound healing: reaction (inflammation), regeneration (proliferation and epithelialization), and remodeling.
The inflammatory response is decreased with age,6,7 and undoubtedly this causes some of the alterations in healing that are subsequently discussed. The proliferative phase traditionally includes cell migration, proliferation, and maturation, all of which are changed with age. Remodeling encompasses the tertiary binding of collagen molecules, which is also altered with age.7 Although all of these stages of wound healing differ with age, the changes are qualitative. Events begin later, proceed more slowly, and often do not reach the same level. However, there are neither new events nor an absence of expected events in the healing of wounds in older adults.
Uninterrupted Wound Repair
After the injury, inflammation allows the destruction of foreign material and microbes. Neutrophils are usually the first cells to the site of injury, and they function to destroy microbes. Macrophages come later and aid in wound healing by removing debris and attracting and promoting proliferation of fibroblasts. Fibroblasts secrete the molecules that form the ground substance and fibers of the scar tissue that fill the tissue loss. The tissue that is generated forms in small piles, resembling the pebbled surface of a basketball, and because of the formation of leaky, new blood vessels, it is beefy red and shiny. This tissue is called granulation tissue, and from this, fibers are generated in random directions but provide little of the tensile strength of normal skin (this is scar tissue). During the proliferation phase, myofibroblasts in the wound pull the wound edges toward the middle, producing wound contraction. Concurrent with and continuing after the wound has completed, granulation is the process of epithelialization. As granulation tissue fills in from the sides of the wound, new epithelial cells are regenerated to cover the scar tissue below. Although mature scar tissue has many of the same components of dermis, it lacks the accessory structures (sweat glands, sebaceous glands, hair follicles, and nails) and blood vessels of natural dermis. The remodeling phase consists of reinforcement of collagen in the direction of stress and the removal of collagen bundles that are unstressed so that a mature scar has approximately 80% of the strength of normal skin.4,5 In fact, during the first 2 weeks of healing, an acute wound regains one-third to one-half of the skin’s original strength. It takes approximately 3 months for a wound to regain nearly 80% of the tensile strength of the original skin. The maturation or remodeling phase of healing continues for 1 year or more; thus, care must be taken in the older person to protect healed areas from reinjury, particularly in the first 3-month period.
An acute wound, such as a surgical incision, may be expected to complete this process in a more rapid and orderly manner than wound dehiscence or a pressure ulcer in an older malnourished individual. The stages of chronic wound repair may not follow the sequence of an acute wound.
Certain conditions need to be in place in order for a wound to heal in a timely manner. Appropriate cells need to be present, including macrophages, granulocytes, fibroblasts, platelets, and both red and white blood cells. Circulation needs to be adequate in order to provide oxygen and nutrients essential for wound healing. A proper electrolyte and fluid balance creates the ideal healing environment. Sufficient amounts of calories to fuel the very high-energy expenditure needed for healing should be present, as well as appropriate amounts of vitamins, minerals, and proteins. Finally, in order to heal 100%, wounds need to be free from infection.
Effects of Aging on Wound Healing
There is a potential for problems in wound healing related to the aging process itself as well as age-associated disease and slower healing as described in Table 14-1. Older individuals may have a decrease in sensory input or neurologic involvement such as paralysis and peripheral neuropathies that may negatively impact their ability to detect potentially destructive pressures. Older patients may experience decreased cognitive ability, fluctuating mental states, weakness and debilitation, and chronic illnesses that lead to immobility, which may predispose them to skin breakdown.6,7
These factors are not the only ones that will affect wound healing in an older population. Tissue and vascular changes related to decreased activity levels will diminish the nutritional health of tissue and increase their vulnerability to injury.
In an older individual with an impaired inflammatory response, blastema cells may appear within days of injury. This is indicative that the tissue repair process is not starting.8,9 The inflammatory response may also be prolonged in an older patient, lasting from 7 to 14 days following the initial injury (generally lasts around 2 to 4 days). The proliferation period is also extended. Typically, this phase of healing lasts for about 3 weeks. In older adults, it is more commonly 5 to 6 weeks in duration.10 A delay in wound contraction and cellular migration and proliferation may occur in older patients, and the remodeling phase varies, ranging anywhere from 2 to 5 years (sometimes even more).11 In an older adult, it is also important to keep in mind that the scar tissue is generally weaker and less elastic than that seen in a younger population.
The aging changes affecting tissue repair as depicted in Table 14-1 influence the rate of healing in older adults. Thinning and flattening of the epidermis result in an increased vulnerability to trauma from shear and frictional forces. The skin is more likely to blister or tear, resulting in a partial-thickness injury. Additionally, changes in sensation and perfusion allow the skin to become macerated or overhydrated, which can lead to breakdown. Once the epidermis has been damaged, it takes longer for the older adult to replace these tissue layers.6,7
Healing also takes longer in the older adult because the epidermal proliferation or turnover time is slowed. The production of new skin cells decreases, and the surface layer simply does not replace itself as readily. The end result is delayed wound contraction and decreased cellular migration and proliferation, resulting in an inefficient and slower rate of healing.7
Atrophy of the dermis results in less elasticity and a thinning of the tissues. This leaves the underlying tissues more exposed and more vulnerable to breakdown. This circumstance also increases the likelihood of dehiscence and delayed wound contraction.12
An older individual’s skin also shows a decrease in vascularity, not only compromising sensation because of nutrient deficiency but also altering the ability to regulate body temperature. Capillary growth decreases, resulting in a reduction in the amount of blood being delivered to the tissues.6,7 Consequently, the tissues become more susceptible to injury and breakdown. Due to the poor vascularity and nutrient status, the skin is more likely to bruise. Small insults can result in hemorrhages that are disproportional to the actual injury.
The quality of the tissue is also compromised in older adults. The loss of collagen and elastic fibers and a delay in collagen remodeling leave the underlying tissue more vulnerable to trauma. The scar tissue of a healed wound is less flexible and much more fragile than the original skin tissue.6,7
The number of sebaceous and sweat glands also decreases, making the skin less moist, lubricated, and resilient. The skin becomes drier, more easily cracked, and is susceptible to infection and fungal development. Because of the loss of hair follicles and touch/pressure receptors, coupled with dehydration, the sensory system is compromised, increasing the chance of injury.
A diminishment in the responsiveness of the vascular system impairs cutaneous immune and inflammatory responses.6,7 It also results in delayed wound closure. There is a reduction in the ability to clear foreign materials or fluids, a decrease in wound capillary growth, and an alteration of metabolic responses.
With age, the ability to discriminate touch, temperature, and vibration declines. The skin is more prone to trauma and burns, often without perception.
Last, the subcutaneous tissue, which is a natural padding system, is reduced. This leaves bony prominences directly exposed to external forces without a protective layer for shock absorption. Because of the abundant circulatory network in the subcutaneous layer, the loss of this layer of tissue also impacts the ability to regulate systemic temperature through vasodilation and vasoconstriction. Older adults are much less efficient at coping with ambient temperature changes.
In addition to alterations in skin condition related to aging, many disease processes will affect the status of the skin. Peripheral vascular disease, for instance, leads to a poor nutritional state and an increased risk for ulceration. Wounds related to the peripheral neuropathy seen in diabetes mellitus are extremely common in the older population.
Factors Complicating Wound Repair
Elimination of exogenous and endogenous impediments to wound repair and meticulous local care are required for humane and cost-effective patient care and satisfactory treatment outcomes.
This section of the chapter provides an overview of factors that might impair healing in an older population. Infection, nutrition, and the aging process are the major factors in the overall success of wound healing in an older population. Additionally, the patient’s complex medical status and potential medical complications may compromise wound healing.
The presence of infection increases the metabolic demands for wound healing and normal cellular functioning.6 The most common complication of wound repair is wound infection. Due to the changing homeostatic mechanism of core body temperature (see Chapter 3) and decreased responsiveness of blood cell production, the body temperature may not be elevated, and white blood cell production may not appear to be increased based on laboratory findings. As a result, the presence of infection may go undetected. Therefore, it is important for the clinician to look for indicators of infection, such as wound color, odor, drainage, pain, and edema, or changes in cognition such as lethargy, confusion, or restlessness. Patients with infection may also report dizziness or light-headedness. In fact, sometimes a fall is the first indicator of an infection. The therapist must be alert to these signs and symptoms, especially when a wound is present.
Many drugs that an older patient may be on compromise wound repair.12 These include the following:
❖ Steroids
❖ Nonsteroidal anti-inflammatory drugs (NSAIDs)
❖ Narcotics and sedatives
❖ Immunosuppressive agents
❖ Antineoplastic drugs
❖ Anticoagulants
❖ Antiprostaglandins
The use of many medications can affect the skin and can lead to an increased risk of breakdown and delay in healing. Steroids and NSAIDs are only a few of the many drugs that affect the skin in older adults. In fact, the use of steroids before or shortly after injury can prolong healing by inhibiting epidermal regeneration and collagen synthesis and decreasing the tensile strength of wound tissues. Not only is the function of fibroblasts and collagen synthesis impaired, but the use of steroids may affect the phagocytic and antibacterial elements of wound repair.7
The use of NSAIDs can delay the reepithelialization of the stratum corneum. Oral NSAIDs, which have been shown to reduce the inflammatory response, may have a significant effect on wounds during the acute phase or on those wounds in which inflammation is a desired response. Narcotics and sedatives can increase the risk for skin disruption simply by decreasing the patient’s mental alertness, thus leading to decreased mobility and activities.
Chemotherapy (immunosuppressive agents) is associated with an increased risk of infection and alteration of collagen synthesis, metabolism, and fibroblast and myofibroblast function.11 The use of immunosuppressive agents may decrease the tensile strength of tissues as well as negatively influence a patient’s response to customary wound care.
Other important drug categories that can affect healing are antineoplastic drugs, anticoagulants, and antiprostaglandins. Complications may also occur as a result of the following factors and need to be considered:
❖ Immunosuppressive diseases
❖ Cytotoxic cleaners, dressings, agents
❖ Radiation therapy
❖ Patient’s environment
❖ Lack of attention to primary etiology of the wound (inadequate pressure relief, inappropriate shoe gear, and inadequate compression with venous disease) and poor patient care
❖ Patient noncompliance
❖ Inappropriate wound care
❖ Nutritional state (including obesity or malnutrition)
❖ Decreased sensation or paralysis
❖ Altered mental status
❖ Urinary incontinence
❖ Hypovolemia
❖ Physical disability and chronic illness leading to immobility
Diseases of the immune system result in an increased risk of infection. A decrease in hematocrit (red blood cells as a percentage of blood volume) or diminished hemoglobin (red blood cell volume) will decrease the availability of oxygen to the system. Any disease that reduces red blood cell production will lead to anemia. Too many red blood cells will also affect healing due to the predisposition of blood clot formation. Low platelet counts can increase the risk of bleeding because of the impaired coagulation function.
Diabetes mellitus is not only associated with poor circulation and ischemia from mechanical factors but also this disease is complicated by an impaired immune system. These patients are less resistant to bacteria that can lead to infection. A decrease in perspiration resulting from the autonomic involvement allows the skin to crack and fissure and increases the vulnerability to infection. Infection can lead to necrosis, gangrene, and amputation.
Chronic venous insufficiency is another problem that increases the risk for infection and is a common medical problem among older adults. This condition also increases the risk of acute thrombophlebitis with potentially life-threatening results. Arterial insufficiency leads to ulceration due to an insufficient blood supply to the lower extremities. Any of these circulatory conditions can be exacerbated by smoking, diabetes, hypertension, or trauma. There is poor perfusion in the lower extremities with arterial insufficiency, leading to claudication and self-restricted activity levels.
Pulmonary diseases reduce the amount of oxygen introduced into the system, thereby affecting peripheral perfusion. Neurologic disorders not only reduce mobility but also impair sensation and increase the risk of breakdown.
Obesity is a neglected problem in the older adult population. With obesity, adipose tissue is poorly vascularized, decreasing the nutrients’ supplies to the various layers of the skin. The increased load places undue stress on the tissues. These patients, although this may not be suspected, are most often malnourished. They consume large amounts of empty calories that do not contain sources of vitamins and minerals.
The converse to obesity is emaciation in older adults. This clearly will increase vulnerability of tissues, especially over bony prominences, and the likelihood that skin status will be compromised as a result of nutritional deficiencies is great.
Older adults are often plagued with urinary or bowel incontinence. Many older adults with incontinence suffer from skin breakdown due to the irritants in excrements and the chronic exposure to moisture. The destruction of the skin’s integrity from moisture combined with bacteria and acidic pH from urine and feces make the skin more susceptible to infection.
Prolonged hypovolemia can result in reduced venous return and a decrease in cardiac output (see Chapter 13) and can lead to a decrease in leukocyte production and activity and compromise collagen production.13
Factors affecting repair of wounds in the older patients include, but are not limited to, delayed cellular activity, decreased wound breaking strength, decreased barrier properties, diminished biosynthetic activity, delayed collagen remodeling and contraction, and decreased vascularity.12 Although caution is suggested in treating older adults, particularly those with friable skin, not all older individuals have a decreased ability to heal. Variations in medical status and health allow many members of the older population to heal as well as the younger population. Surgeries are frequently performed on older adults with no problems with healing. When treating older adults for healing wounds from any origin, keep in mind the following12:
❖ Exercise caution when using adhesives and tapes on friable skin
❖ Avoid frequent scrubs
❖ Avoid irritating and cytotoxic agents
Complication of wound repair may occur because of numerous intrinsic and extrinsic factors. It is important for the wound care team to consider the whole of a patient’s medical status when dealing with a wound in an older person. When a wound shows no response to treatment after 2 weeks, the patient’s medical and wound status should be reevaluated. When there are no new findings regarding medical status, a different wound care approach (product, modality, and medication) should be considered.
NUTRITIONAL CONSIDERATIONS IN WOUND CARE
Optimal nutritional status is essential for healing a wound, regardless of the age of a patient.14 However, protein-calorie, vitamin, and mineral malnutrition, especially in hospitalized postsurgical older patients, occurs in about 50% of older individuals. In fact, it has been determined that nutritional status often deteriorates during a hospital stay.15 Older patients discharged from the hospital with open wounds are likely to have tenuous nutritional status and need careful attention to diet if their wounds are to heal. Nutritionally, the immune system can be bolstered through attention to the diet.
PATIENT AND WOUND EVALUATION
Accurate assessment and evaluation of a wound are very important. Identifying causation problems (positioning, diagnoses, and functional capabilities) will assist the clinician in treating the current wound and preventing future wounds from occurring.
Thorough knowledge and assessment of the physical and pathological etiologies of wounds are prerequisites to treating lesions successfully. Patient evaluation should include a comprehensive review of systems, review of medications, prior and current treatment modalities, the patient’s awareness of the problem, the external environment that may affect wound care and future prevention, and nutritional status. If possible, the date of wound onset should be established in addition to identifying contributing factors. A history of significant medical diagnoses such as diabetes, hypertension, congestive heart failure, renal disease, chronic obstructive pulmonary disease, peripheral vascular disease, lymphatic insufficiency, recent weight loss, and other problems that may impact the effective treatment of the wound should be established. A history of previous wounds and the types of treatments and results are also important areas of assessment. Medications that may affect wound healing such as steroids or anticoagulants need to be documented. Identifying allergies to topical medications or whirlpool additives should be determined.
Laboratory findings, especially culture reports of the wound if available, will assist in establishing the direction of intervention. Any malnourished geriatric patient is not at a greater risk for the development of an ulceration but will require more healing time. Testing the protein and serum albumin levels is crucial to predicting wound healing. A low protein level will impede collagen synthesis, fibroblast proliferation, and wound remodeling. Phagocytosis and the immune response will also be impaired. An older patient with a wound will need higher protein sources. Low serum albumin levels represent late manifestation of protein deficiency. Normal albumin levels are 3.5 to 5.0 g/dL. A severely compromised albumin level would be less than 2.5 to 3.0 g/dL.
Laboratory evaluation may also be needed to determine the availability of other nutrients that will expedite wound healing. For example, vitamins A and C assist in collagen synthesis. vitamin C affects fibroblastic and immune function, while vitamin A promotes reepithelialization. Minerals such as zinc may increase epithelialization and cell production.
Chapter 13 provides a model for assessing peripheral circulation and central cardiovascular status. Evaluating the presence of pulses, particularly in distal wounds of the lower extremity, will determine the viability of the tissues for healing. Assessing the overall skin integrity including hydration, turgor, and areas of discoloration will provide information on the tissue’s nutritional status and the prospect of healing the wound.
Arterial pathologies need to be assessed in an objective manner. It is crucial that the tissue receive oxygen. If blood flow to a wound is impeded, oxygenation and nutrients will be blocked and CO2 and metabolic by-products will not be removed. Without oxygen, collagen synthesis and fibroblast differentiation will not occur. In the course of the physical examination, beyond assessing the dorsal pedis pulse and a posterior tibial pulse, if a portable Doppler is available, this is an objective means of evaluating peripheral circulation. The Buerger-Allen protocol of assessment described in Chapter 13 is also an excellent means of objectifying the status of peripheral circulation.
Venous problems will affect the removal of waste products from the lower extremities and affect the nutritional health of the tissues.16 Has the patient ever experienced a leg injury? A previous injury often leads to increased venous hypertension, which will progress to lipodermatosclerosis—the visible brown pigmentation and induration of the legs. Edema will keep oxygen and vital nutrients from entering the wound site.
Determine the neurosensory status (eg, anesthesia, paresthesia, pain, and pressure) using the Semmes-Weinstein filaments as described in Chapter 13 to establish the integrity of sensory input. Assessing pain patterns will help to identify symptoms and activities that increase or decrease pain.
Determining mobility status including activities of daily living (ADLs), flexibility, strength, locomotion, and self-positioning will be predictive of the rate of healing as well as the potential efficacy of preventive interventions. Assess position needs and equipment to promote wound healing. Immobility is the leading cause of pressure ulceration.16 A healthy individual capable of feeling noxious stimuli over a bony prominence will alleviate pressure by moving that part. On the other hand, older patients who are immobilized secondary to illness with sensory deprivation, friable skin, and poor circulation have no comparable defense, nor do patients with diabetes, who have a diminished protective sensory threshold. If the individual cannot reposition him- or herself or move the affected limb, an ulcer sets in via hypoxia. This is a patient who needs pressure-relieving devices and repositioning on a regular schedule.
The presence of incontinence is another risk factor that increases the potential for skin breakdown by creating a moist environment, which, if not attended to, leads to maceration and chemical irritation. If incontinent patients move their extremities in a urine- or bowel-soaked environment, shear and friction will easily tear the outer layer of soft wet skin, eventually resulting in a breach in integument and paving the way for the possibility of wound infection.
When evaluating a wound, it is important to augment the assessment by appraising the following risk factors:
❖ Is the patient ambulatory?
❖ Is the patient oriented and able to understand directives?
❖ Is the patient eating independently or receiving nourishment through other sources (supplements or tube feeding)?
❖ Does the patient have a sensory deficit, or can pain be felt in the wound area?
❖ Does the patient have a significant other or caretaker who can assist with care of the wound?
❖ Are there other contributing factors, such as urinary incontinence, poor nutrition, arterial occlusions, venous insufficiency, or perhaps diabetes?
Table 14-2. Common Descriptions of Wound Appearance in Documentation
DESCRIPTION | IMPLICATION |
| Red-reepithelializing | Bright red with indications of superficial cell migration; good wound bed and healing well |
| Red-granulating | Bright or true red in appearance associated with islands of granulation tissue and good healing |
| Red-chronic | Red appearance but no indication of granulation; poor or delayed healing |
| Red-dusky | Dull, gray, or dark red in appearance without signs of granulation, with or without signs of localized ischemia; poor healing with possibility of infection |
| Yellow-granulating | Areas of fibrotic tissue (not usually classified as healthy or unhealthy) present in conjunction with areas of granulating tissue; no necrotic tissue present; delayed healing |
| Yellow-chronic | Areas of fibrotic tissue without areas of granulation; poor healing |
| Yellow-ischemic | Fibrotic tissue in conjunction with signs of ischemia or tissue necrosis; delayed or poor healing |
| Black-dry | Dry, desiccated eschar whether black or brown in appearance; poor healing with tissue death |
| Black-wet | Wet gangrenous appearance; tissue death with progressive infection |
| Black-mixed | Areas of necrotic tissue present with areas of yellow and/or red tissue; tissue death with areas of infection and sporadic areas of healing |
DOCUMENTATION AND STAGING OF WOUND STATUS
In the present arena of wound care, accurate documentation is critical for securing reimbursement. While the principal rationale for documentation is to legally record information, equally important is communication with other health care professionals and third-party payers. Over time, documentation can also be used as a database for clinical research, outcomes, peer review, and the quality improvement process.
Wound evaluation and documentation includes determination of the following:
❖ Etiology and type of wound
❖ Infection vs contamination
❖ Size of wound
❖ Undermining of sinus tracts
❖ Quality and quantity of exudate
❖ Underlying structures (muscles, tendons, and bones)
❖ Stage of healing
❖ Chronicity
❖ Response to previous treatment
In evaluating the wound, it is important to document the location of the wound and the type of wound (eg, arterial vs venous insufficiency, vasculitic, pressure ulcer, diabetic ulcer, burn, abrasion, surgical, laceration, shearing, hematoma, stasis). The charting of the size of the wound should include the length, width, depth, presence of undermining, and description of the shape of the wound. The status of the wound bed and the surrounding tissue should be described in a clear and concise manner. Color, odor, and exudate are all indications of wound status. The color of the wound is indicative of the stage of repair. Odor is the best way to determine if the wound is infected. It is helpful to evaluate odor after a wound has been cleansed with sterile water or saline. Foul odor may result from the accumulation of wound exudate, necrotic tissue, and dressing by-products, especially after the use of occlusive dressings. Common examples of appearance of wounds are provided in Table 14-2. Necrotic tissue promotes bacterial growth and when left in a wound will slow the formation of granulation tissue and epithelialization, inhibiting angiogenesis.16
The presence of the exudate should be recorded, and the description of the drainage would include the amount, color, and viscosity (ie, serous, serosanguineous, sanguineous, or purulent). The condition of the wound tissue includes a description including the presence of granulation, epithelialization, slough, eschar, or hemorrhage. It is also important to note the condition of the surrounding tissue in terms of pain, swelling, tenderness, erythema, discoloration, maceration, inflammation, skin temperature, skin texture, and hair loss. If edema is significant, baseline girth measurements need to be taken.16
It is important that the wound be graded in some fashion so that all health care professionals know the nature of the wound they are dealing with. There are many acceptable staging guidelines. Many clinicians use the Wagner’s ulcer grade classification system, which is specific to foot ulcerations; others prefer the more general staging system developed by the National Pressure Ulcer Advisory Panel. Both provide a means of objectifying wound status and facilitating consistent communication of the status of the wound.
Wagner’s classification17 was developed to objectively evaluate foot condition and ranks vascular dysfunction in grades of 0 to 5 as follows:
❖Grade 0: The skin is without ulceration. No open lesions are present, but potentially ulcerating deformities, such as bunions, hammer toes, and Charcot deformity, may be present. Healed partial foot amputation may also be included in this group.
❖Grade 1: A full-thickness superficial skin loss is present. The lesion does not extend to bone. No abscess is present.
❖Grade 2: An open ulceration is noted deeper than Grade 1. It may penetrate to tendon or joint capsule.
❖Grade 3: The lesion penetrates to bone, and osteomyelitis is present. Joint infection or plantar fascial plane abscess may also be noted.
❖Grade 4: Gangrene is noted in the forefoot.
❖Grade 5: Gangrene involving the entire foot is noted. This is not salvageable with local procedures.
The National Pressure Ulcer Advisory Board16 provides a staging scheme for nonfoot ulcers. This staging is as follows:
❖Stage I: Nonblanchable erythema of intact skin, heralding lesion of skin ulceration. Dangerous if left unprotected. Often progresses quickly to Stage II or greater.
❖Stage II: Partial-thickness skin loss involving epidermis and/or dermis. Clinically, the lesion presents as a large blister or abrasion. Displayed most commonly under heels of older adults due to friction and shear from heel movement, especially in immobile older adults following hip surgery.
❖Stage III: Full-thickness skin loss involving damage or necrosis of subcutaneous tissue, which may extend down to, but not through, underlying fascia. It is imperative to check for undermining or sinus tracts.
❖Stage IV: Full-thickness skin loss with extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures.
These classification systems assist in describing the severity of the wound. In many cases, these staging systems have prognostic value and, in some instances, reimbursement value. Complete description and classification are essential components of the diagnostic and therapeutic process in wound care.
Included in the grading or staging of a wound, the following descriptors should be provided in the initial and ongoing documentation of the wound:
❖ Location of wound
❖ Surface dimension of wound
❖ Color of wound base
❖ Presence of necrotic tissue (amount and color)
❖ Depth and tissue layers involved
❖ Exudate (amount, color, and odor)
❖ Condition of the surrounding skin
❖ Undermining
❖ Clinical signs of infection (see the subsequent section on microbiology)
There are several methods that can be used to determine the size and shape of a wound. Whichever method is chosen, it is imperative that the therapist continues to use the same method consistently throughout the healing process because different methods give different results. The therapist may wish to use a combination of methods. For example, measuring length and width as well as volume gives an excellent 3-dimensional representation of the wound’s actual size. As the wound heals, the length and width may actually become larger; yet, the total volume of the wound will decrease. It is imperative to document which methods are being used, so the same techniques can be followed by other therapists. Therapists must also coordinate measuring procedures with the nursing staff or wound care team members.
It is helpful to keep the time intervals between measurements consistent. A decline in the rate of healing may be the first indication of a need to change treatment approaches.
In the presence of an ulceration, objective documentation of wound size is best accomplished by tracing the wound on sterilized x-ray film or through photographs on a line-graphed film. This is helpful in monitoring improvement or decline in wound status. Some x-ray–type films are available with a bull’s eye pattern that provides diameter and metric measures. This sort of industry-prepared measuring tool is useful in objectively tracing wound perimeters. Figure 14-3A provides an example of this sort of device.
Tracings, tape measurement guides, volumetric displacement, plain meter, and photographic measurement are all excellent ways of documenting wound status. The combination of measurement techniques used will be dictated by the patient’s individualized status and plan of care. Wounds may be measured in a linear fashion and described as an area (eg, 6 cm × 4 cm) or traced on an acetate measuring guide as presented in Figure 14-3A. The length and width of a wound to obtain size may be accomplished by using a clear ruler and measuring the longest and the widest aspects of the wound. Tracings on acetate can be transferred to a grid as shown in Figure 14-3B. As depicted in this drawing, the wound is represented by the solid line, and the measured area of undermining is represented by the dashed line. Periodic tracing can be superimposed on this graph in varying colors and dated to indicate ongoing status of the wound. This gives a wonderful visual representation of the change in wound size and status. By using graph paper, width and length measures are easy to obtain. The area of the wound can be calculated by counting the number of squares contained within the boundaries of the wound.
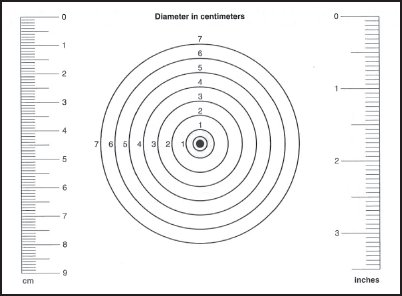
Figure 14-3A. Bull’s eye and linear measurement acetate (x-ray) film for tracing and measuring the size of the wound. The center of the bull’s eye is placed in the center of the wound, and the periphery of the wound is traced.
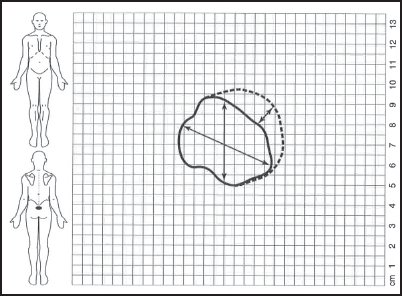
Figure 14-3B. Grid documentation of the location and area of a wound.
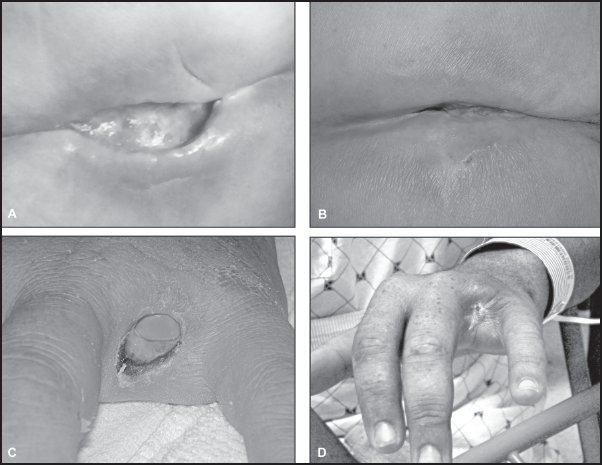
Figure 14-4. Pho to graphic documentation of wound status over time. (Reprinted with permission from Irion G. Comprehensive Wound Management. 2nd ed. Thorofare, NJ: SLACK Incorporated; 2010.)
If acetate film is not available for tracing, placing 2 layers of plastic wrap over the wound and using a permanent ink marker to trace the outline of the wound is an inexpensive way of tracing the wound. Dispose of the bottom layer of plastic as infectious waste and photocopy the top layer onto the metric graph paper. Approximate the area within the wound by counting the boxes within the wound’s borders (see Figure 14-3B).
Tracings enable more accurate comparison of change in wound perimeter over time. These small acetate (x-ray film) measuring sheets are provided at no charge by numerous companies that provide wound care products. Many clinicians add photographic documentation.18 A series of accurate photos taken over time provides historic data about the wound and its progress and serves as visual support for written documentation. A photograph of the wound is the most reliable documentation. Serial photographs provide objective evaluation of wound healing as demonstrated in Figure 14-4.
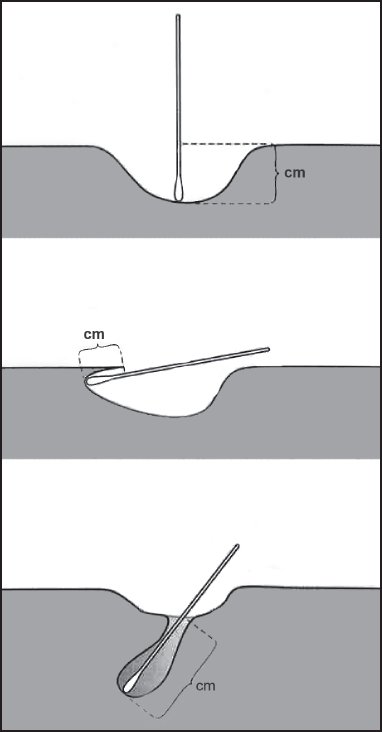
Figure 14-5A. Measurement techniques for determining the depth, extent of undermining, and sinus tract of a wound using a cotton swab applicator.
Measuring wound depth can be accomplished by putting a cotton-tipped applicator or tongue depressor into the base of the wound and then placing the acetate or ruler across the wound surface and marking the point it encounters the cotton swab or depressor. This measures the distance from the tip of the swab to where the applicator is even with the intact skin and provides a measure of the depth of the wound.
Undermining, which is defined as skin overhanging a dead space, should be measured with a gloved finger or a cotton-tipped applicator. To measure undermining, place a cotton-tipped applicator into the wound to the extent of the undermining. Gently lift the applicator toward the skin surface until the skin is raised slightly. Mark this location with a skin pencil. Repeat at close intervals around the perimeter of the wound. On the grid paper, the areas of undermining and their depth can be indicated with dashed lines as indicated in Figure 14-3B. This area, as it is probed, can be traced on the plastic wrap or acetate film as described earlier.
When sinus tracts are suspected, they should be probed gently with a cotton-tipped applicator or a small red rubber catheter to determine their length. A cotton-tipped applicator is placed into the tract, and the distance is measured from the tip of the swab to where the tract enters the wound bed. T he position of the tract should be noted by using a clock system with the head of the patient at 12 o’clock and the feet at 6 o’clock. Measurement techniques for depth, sinus tract, and undermining are provided in the drawing in Figure 14-5A.
Volumetric measures are also very helpful. By filling the wound with sterile water or saline just to the point of overflowing and then suctioning the water out of the wound using a needleless syringe, the volume of water it takes to fill the wound can be measured in cubic centimeters or milliliters by reading the syringe markings. This gives an accurate measure of the volume of the wound. (Note: The wound must be in a position that it can be filled without the water spilling out.) Figure 14-5B provides a pictorial demonstration of this technique.
One technique for measuring volume is to use a substance called Jeltrate (Dentsply Sirona). This is a hydrocolloid substance that will not adhere to the wound or damage granulation tissue. However, this gel-like substance should not be used in wounds with very small surface openings or with large areas of undermining or tracking. The Jeltrate technique involves adding water to the Jeltrate powder according to the package instructions. Then pour the liquid into the wound and allow it to solidify (takes around 5 minutes). Remove the mold from the wound and place it into a graduated cylinder partially filled with a premeasured amount of water. Record the amount of water displaced as demonstrated in Figure 14-5C. This water displacement represents the volume of the wound. This mold is also an excellent teaching tool for patients, family members, or nursing staff.
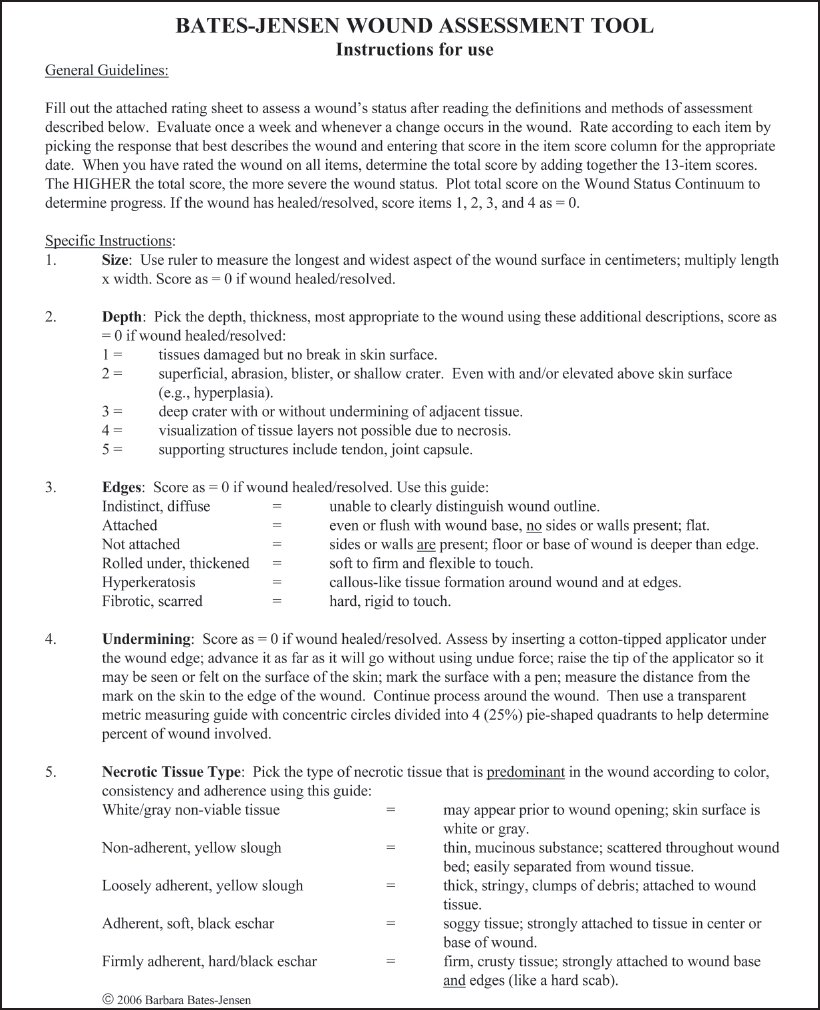
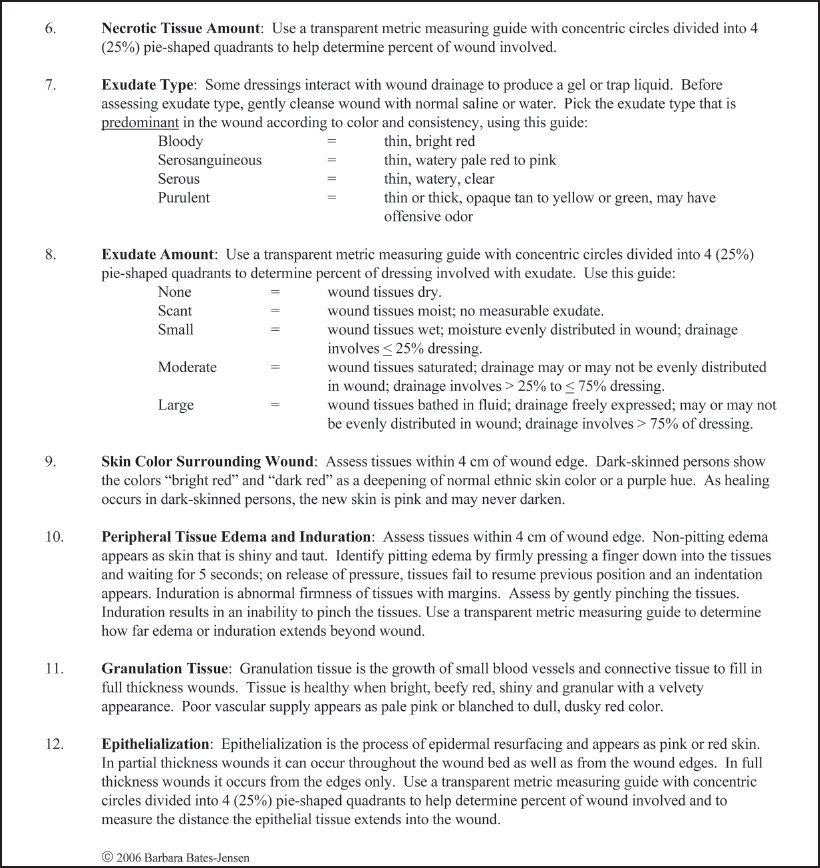
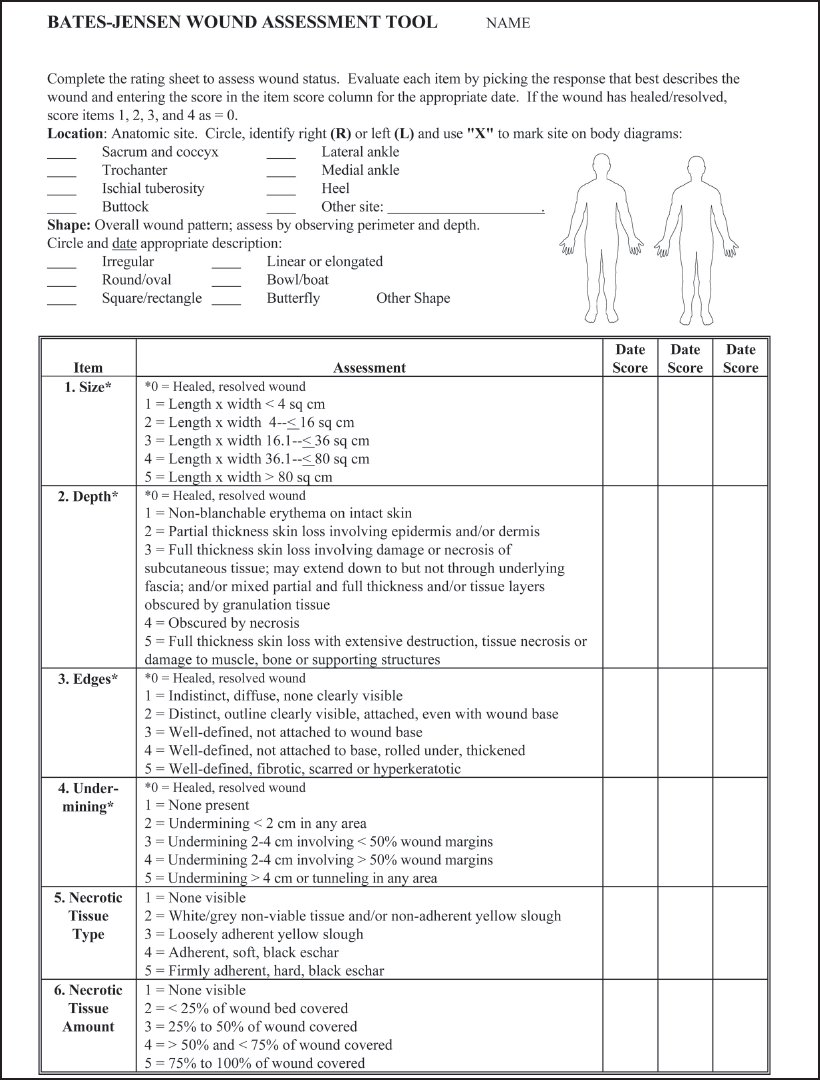
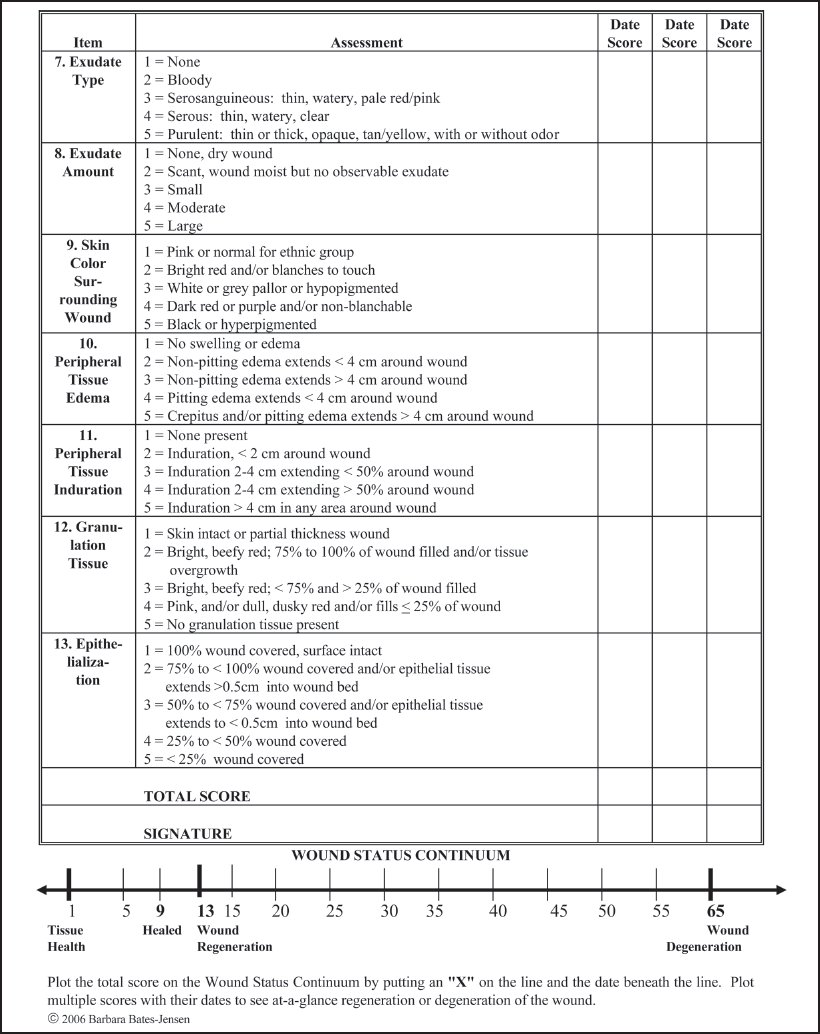
There are many excellent wound assessment tools available that provide a standardized format for documenting wound status. A helpful tool, because it objectively scores each parameter for accurate monitoring of the patient’s condition, was developed by Barbara Bates-Jensen (Figure 14-6).19,20
Accurate documentation enables critical evaluation of the wound healing process and helps to inform clinicians of the wound status in an objective way. The key to future research in the pathophysiology of chronic wounds and therapeutic efficacy depends on precise reporting of incidence and types of chronic wounds and the use of consistent terminology. Documentation can provide the database of healing as well as nonhealing wounds required to establish the need for physical therapy or the database of healing needed to secure reimbursement from intermediaries.
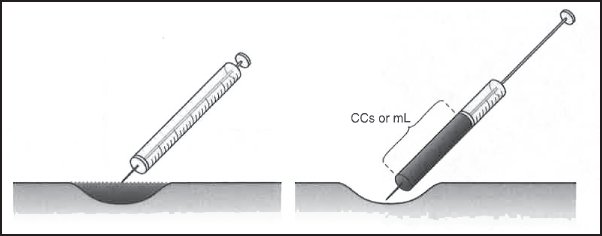
Figure 14-5B. Measuring the area of the wound using a volume measurement. Fill the wound with sterile water or saline to a level point. Suction fluid from the wound to get volume measure in cubic centimeters or milliliters.
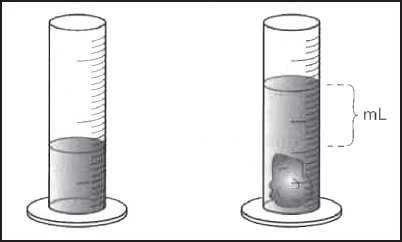
Figure 14-5C. Volumetric measurement using a Jeltrate mold of the wound and determining the displacement of water in a premeasured vessel.
MICROBIOLOGY
Bacteria is often found in chronic wounds. There is a distinction drawn between a contaminated wound and an infected wound. According to Mulder and associates,12 wound appearance can be misleading. The degree of contamination and the distinction between contamination and infection are difficult to determine; other signs of wound infection may need to be assessed.12
Indicators of wound contamination may include periwound erythema, inflammation, nonpurulent drainage, malodorous (foul smelling) wound prior to cleansing, and multiple organisms present on swab culture. The same signs are present with infection; however, other established signs of infection are elevated body temperature, cellulitis, purulent drainage, wet gangrene, increased leukocytosis, persistently malodorous wound (even after cleansing), and greater than 105 organisms per gram tissue on culture.12 Other indications of infection might include pain, swelling, redness, inflammation, and heat.
Swab cultures are of questionable value as multiple bacteria are often present in wound fluid and wound surface, particularly when occlusive dressings have been used. Surface organisms do not correlate well with the number and type of organisms present in the tissue. Other clinical signs of infection must be present when determining that organisms present on culture are of clinical significance. For the most accurate results, it is important that the wound be thoroughly cleansed prior to culturing. Organisms found need to be coupled with other clinical indicators of infection.
LOWER EXTREMITY ULCERS
Different wound types exhibit different characteristics depending on their underlying etiology and cannot all be treated identically. Combinations of wound types further complicate the identification and treatment of wounds, especially in older adults. For example, many diabetic ulcers result from pressure. Likewise, many patients with peripheral vascular disease may also be diabetic or have other chronic disabilities that limit their activity levels, which puts them at greater risk for breakdown as a result of immobility and pressure. The type of pressure causing diabetic ulcers is repetitive, callus-forming pressure, whereas pressure ulcers are an ischemic event. Therefore, the identification and treatment of a diabetic ulcer are different from that of a pressure ulcer. The fact that current treatment strategies are based on proper wound classification illustrates the need for the clinician to assess and classify wounds properly, even if a particular wound type is not seen in the clinician’s practice setting. Table 14-3 provides 5 different types of wounds that may be encountered in the clinic and describes characteristics that differentiate each one.21–25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree