13315
Breast Cancer
Shlomit Strulov Shachar, Trevor A. Jolly, Noam VanderWalde, and Hyman B. Muss
INTRODUCTION
Major advances in medical care and public health have resulted in dramatic increases in life expectancy. A woman born now has a life expectancy of 81 years, and the U.S. female population 65 years and older will grow from 26.4 million in 2015 to 46.2 million in 2050 (1). This surge in the aging female population corresponds to a striking rise in breast cancer (BC) cases, as the incidence of BC increases dramatically with age. BC is the most common cancer among women in the United States, accounting for nearly one in three female cancers. It is also the second leading cause of cancer death among women after lung cancer (2).The average age at diagnosis of BC is 62 years, and the majority of woman who die of BC are older than 65 years. The combination of an aging population with an increased incidence of BC and other comorbidities related to aging make management of this expanding group of older patients a major challenge. Treatment of BC in the elderly is especially challenging because older adults, even those with normal performance status, are more likely to have physiologic changes, functional deficits, comorbid medical conditions, and polypharmacy, which increase the risk of treatment toxicity (3). Geriatric assessment can identify such deficits, predict treatment toxicity, and may lead to interventions that improve quality of life (QoL) and preserve function (4).
SCREENING MAMMOGRAPHY
The American Cancer Society recommends that women should continue mammography screenings as long as their overall health is good and they have a life expectancy of 10 years or longer (qualified recommendation) (5). The U.S. Preventive Services Task Force has no recommendation for women older than 75, as there is insufficient evidence to support any firm recommendation (6). In a large study based on Surveillance, Epidemiology, and End Results (SEER) data, Black and White women aged 75 to 84 years who had annual mammography had lower 10-year BC mortality than corresponding women who had biennial or no/irregular mammographies (7). We recommend screening in women above 65 annually or biennially provided they have at least a 10-year average life expectancy, and after discussion of the risks and benefits. An excellent review of this topic is available (8) and a web-based model (cancerscreening.eprognosis.org/) can help in decision making (9).
BC PHENOTYPES
134After age, life expectancy, and the goals of treatment are taken into account, BC treatment decisions can be made on the basis of stage, histologic subtype, tumor grade, and phenotype. For simplicity’s sake, BC can be divided into three major phenotypes: (a) hormone receptor (HR) (estrogen and/or progesterone receptor) positive and human epidermal growth factor receptor-2 (HER-2) negative tumors, which are found in the majority of patients; (b) HR negative and HER-2 negative tumors (so called “triple negative” BC); (c) HER-2 positive tumors (with any HR status). HR positive and HER-2 negative tumors increase with age and account for about 75% of tumors in women aged 70 and above, and most relapses occur 5 years after diagnosis. Patients with HER-2 positive and triple negative BC who relapse generally do so within 5 years of diagnosis. More recently, genetic assays of tumor tissue have divided BC into several major subtypes (10). Although the frequency of more favorable subtypes (luminal A and B tumors) increases with age, many older women have high-risk subtypes—an important finding because prognosis and treatment outcomes are similar and independent of age once subtype is accounted for (11).
MANAGEMENT OF THE PRIMARY LESION
Primary Endocrine Therapy
The majority of older patients will have HR positive, HER-2 negative tumors and comorbidities associated with aging that sometimes lead to life expectancies of only several months or years. Primary endocrine therapy can be an excellent option for such patients. This strategy is also appropriate for those with HR positive, HER-2 negative unresectable primary lesions, for which preoperative endocrine therapy can decrease tumor size and allow for either mastectomy or breast preservation. We prefer aromatase inhibitors (AIs) in this setting, due to their more favorable treatment effect and toxicity profiles, and because unlike tamoxifen, there is no increased risk of uterine cancer or thromboembolism (12). Primary endocrine therapy controls tumor growth for about 18 to 24 months on average (13), making it an appropriate treatment for patients with a short life expectancy. Although time to onset of a response may take several months or longer (14), many patients will have continuous disease control throughout the rest of their lives. However, the cornerstone of early BC treatment at any age remains surgery, unless the patient has a short life expectancy, declines surgery, or is not a suitable surgical candidate (15).
Surgery
Elderly patients generally tolerate surgery well and with low complication rates (16). Most older women will be candidates for breast preservation. Sentinel node biopsy is a safe and accurate procedure (17) and should be offered to women with clinically negative axilla, provided the information will help in decision making. Axillary lymph node dissection should be considered in patients with clinically involved axillary nodes, provided such patients have a reasonable life expectancy.
135Radiation Therapy
Adjuvant radiation therapy (RT) plays an important role in the treatment of most women undergoing breast conservation surgery for early stage BC. The Early Breast Cancer Trialists, Group (EBCTG) meta-analysis demonstrates that the addition of radiotherapy to breast conservation surgery decreased recurrence by 15.7% (35.0% vs. 19.3%) at 10 years and BC-related death by 3.8% (25.2% vs. 21.4%) at 15 years for all patients (18). However, for older patients with potentially lower risks of recurrence and a higher likelihood of death from comorbid conditions, many questioned the value of breast irradiation, leading to at least five large randomized studies of older women with early stage BC comparing adjuvant RT to no RT (19–23). Arguably, the most impactful of these studies thus far has been Cancer and Leukemia Group B (CALGB) 9343. At 10 years, locoregional recurrence rates were 10% in those not receiving RT, compared to 2% in those who received RT (P < .001). No difference in disease-specific or overall survival was found, and the vast majority of deaths were due to non-BC causes (21). Due to the relatively low risk of locoregional recurrence even without RT, this and other studies have been used to justify the omission of RT in older women with T1N0 hormone positive BC (24). Care should be taken not to extrapolate the results of these studies to patients who do not meet the strict eligibility criteria for study entry; higher risks of locoregional recurrence have been found among patients with larger, higher grade, and/or hormone-negative tumors (25).
Locoregional radiation should also be considered for women postmastectomy who have large tumors and/or nodal involvement; in this setting, radiation can substantially decrease locoregional recurrence and improve survival. Multidisciplinary consultations with breast surgeons, medical oncologists, and radiation oncologists for all older patients are recommended (see Table 15.1 for more details).
ADJUVANT SYSTEMIC THERAPY
The purpose of adjuvant systemic therapy in patients with early BC is to increase the chances for long-term disease-free survival. Goals of treatment, assessment of life expectancy, and geriatric assessment should be performed before making systemic treatment decisions. The estimation of the potential value of endocrine therapy, chemotherapy, and anti-HER-2 directed therapies can be made using online calculators (e.g., www.adjuvantonline.com, and www.predict.nhs.uk/predict.html—see Table 15.2), and detailed review is available (26). The PREDICT model also estimates the absolute benefit in overall survival of trastuzumab-based regimens in patients with HER-2 positive tumors and can accurately predict 5-year survival in the elderly (27). However, the added value of chemotherapy appears to be overestimated in Adjuvant! (28). General recommendations for use of systemic therapy are shown in Figure 15.1. International Society of Geriatric Oncology (SIOG) guidelines (30) and current reviews, including one on management of BC in women older than 80 years, are available (31,32).
TABLE 15.1 Adjuvant Radiation Studies
136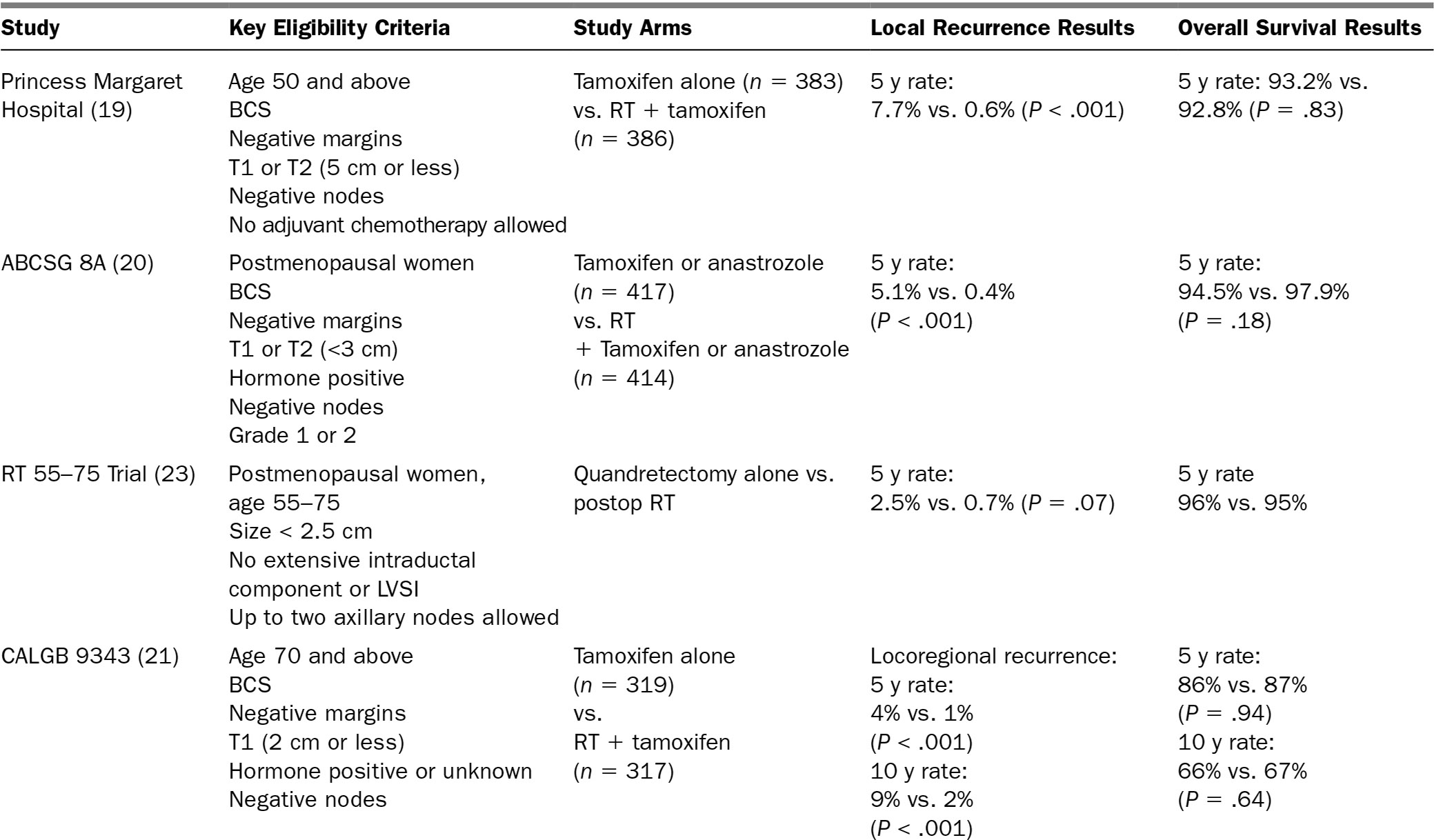
137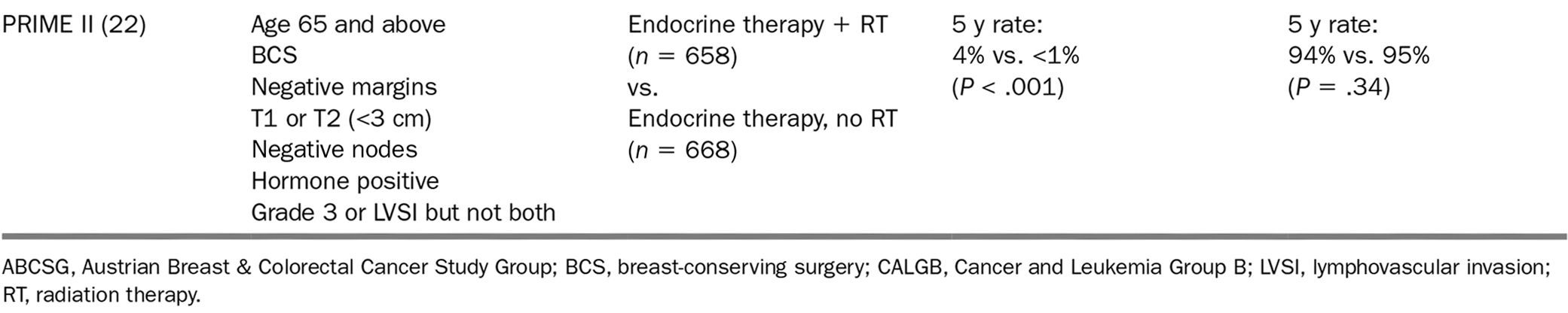
138TABLE 15.2 Web-Based Calculators for Treatment Benefit, Toxicity Risk, and Life Expectancy
Name | Details |
BC predictive websites | |
Adjuvant!* | Calculator that estimates benefits of adjuvant therapy. Also consider comorbidities. |
PREDICT | Calculates benefits of adjuvant therapy for patients with BC. Does not consider comorbidities. Does consider anti-HER-2 treatment benefits. |
Screening benefits, life expectancy, and toxicity prediction calculators | |
ePrognosis | Calculator for estimating life expectancy. |
ePrognosis | Calculator for estimating cancer screening benefit. |
Moffitt Cancer Center Senior Adult Oncology Program Tools moffitt.org/cancer-types–treatment/cancers-we-treat/senior-adult-oncology-program-tools | Calculator for estimating chemotherapy toxicity. |
CARG (Cancer and Aging Research Group) | Calculator for estimating chemotherapy toxicity. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








