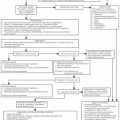
Class of Agents |
Indication |
Dose and Schedule |
Interferons |
Interferon α-2a |
CML |
SQ: 5 million or 2 million units/m2 daily for 1 mo, followed by 3 times/wk. |
Interferon α-2b |
HCL Melanoma Kaposi sarcoma |
IM or SQ: 2 million units/m2 3 times/wk for up to 6 mo for HCL SQ: 5 million units 3 times/wk for up to 18 mo for FL.
IV: Induction: 20 million units/m2 for 5 consecutive days per week for 4 wk, followed by maintenance dosing of 10 million units/m2 SQ 3 times/wk for 48 wk for melanoma.
IM or SQ: 30 million units/m2 3 times/wk for Kaposi sarcoma. |
Interleukins |
Interleukin 2 |
Melanoma RCC |
IV: 600,000 int. units/kg every 8 h for a maximum of 14 doses; repeat after 9 d for a total of 28 doses per course (repeat if tumor shrinkage). |
Tumor necrosis factors |
TNF-α |
Melanoma Sarcoma |
Different dose schedules according to studies. Rarely used. |
Cancer vaccines |
Sipuleucel-T |
Metastatic prostate cancer |
IV: ≥50 million autologous CD54+ cells activated with PAP-GM-CSF. |
MAb |
|
MAb Target |
Antigen |
Indication |
Dose and schedule |
Lymphoproliferative disorders |
Rituximab |
CD20 |
CLL, FL DLBCL |
IV: 375 mg/m2 on the day 1 of FCR, then 500 mg/m2 on day 1 (every 28 d) of cycles 2-6 in CLL.
IV: 375 mg/m2 QW for 4 or 8 doses for LG NHL, or on day 1 of each combination chemotherapy cycle for up to 8 doses in HG NHL. As maintenance in LG NHL QW for 4 doses then Q6 months for up to 4 cycles. |
|
Ofatumumab |
CD20 |
CLL FL |
IV: 300 mg week 1, followed by 2000 mg QW for 7 doses, followed by 2000 mg Q4W for 4 doses. |
|
Tositumomab |
CD20 |
Relapsed refractory low-grade NHL |
IV: 450 mg over 60 min followed by I 131 Tositumomab. Repeat 7-14 d later by Tositumomab 450 mg and I 131 to deliver 65-75 cGy TBI. |
|
Ibritumomab Tiuxetan |
CD20 |
Relapsed refractory low-grade NHL |
IV: Rituximab infusion: 250 mg/m2 followed by 5 mCi of In-111 Ibritumomab infusion on day 1, Repeat day 7-9 with up to 32 mCi of Ibritumomab. |
|
Alemtuzumub |
CD52 |
CLL, T-PLL |
IV: 3 mg/d on d 1; up to 30 mg/dose 3 times/wk on alternate days for up to 12 wk. |
|
Brentuximab |
CD30 |
HL, ALCL |
IV:1.8 mg/kg every three weeks for up to 16 cycles |
Myeloid disorders |
Gemtuzumab Ozogamicin |
CD33 |
AML |
Withdrawn from the market. |
Solid tumors |
trastuzumab |
HER2 |
Breast cancer, Gastric adenocarcinoma |
IV: 4 mg/kg day 1, followed by 2 mg/kg QW for 1 y or 8mg/kg followed by 6 mg/kg Q3W for 1 y or until disease progression. |
|
Bevacizumab |
VEGF |
Breast, colon, NSCLC, RCC |
Mainly in combination with chemotherapy: IV: 5 mg/kg Q2W in breast or colon cancer. |
|
|
|
Glioblastoma |
IV: 10 mg/kg Q2W for colon, RCC or glioblastoma.
IV: 15 mg/kg Q3W for NSCLC. |
|
Cetuximab |
EGFR |
Colon, NSCLC and H&N cancer |
IV: 400 mg/m2 day 1, followed by 250 mg/m2 QW. |
|
Panitumumab |
EGFR |
Colon cancer |
IV: 6 mg/kg Q2W. |
|
Ipilimumab |
CTLA4 |
Melanoma |
I.V.: 3 mg/kg every 3 weeks for 4 doses |
Abbreviations: DLBCL, diffuse large B cell lymphoma; HCL, Hairy cell leukemia; CML, chronic myelogenous leukemia; CLL, chronic lymphocytic leukemia; RCC, renal cell carcinoma; FL, follicular lymphoma; NHL, non hodgkin lymphoma, HL, hodgkin lymphoma; T-PLL, T cell prolyphocytic leukemia; AML, Acute myeloid leukemia; NSCLC, non small cell lung cancer; H&N, head and neck; CD, cluster of differentiation; IM, intramuscularly; SQ, subcutaneous route; IV, intravenously; QW, every week; LG, low grade; HG, high grade/aggressive. |