FIGURE 27.1 Bismuth-Corlette classification scheme of malignant biliary strictures.
TABLE 27.1 AJCC Staging System, Seventh Edition, for Hilar Bile Duct Cancer
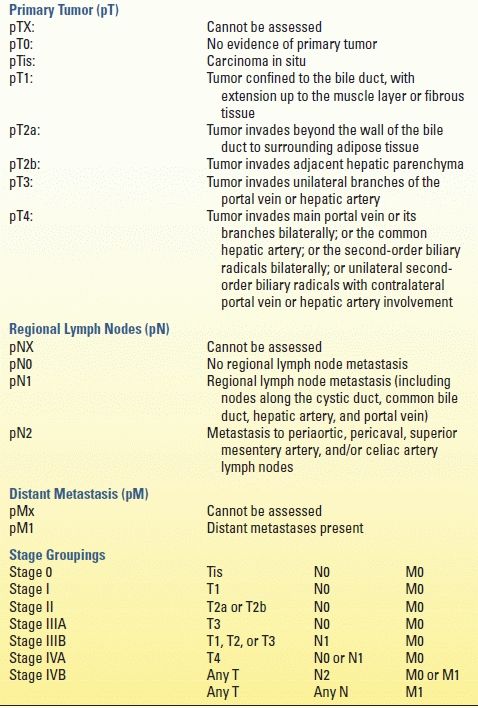
From Cholangiocarcinoma. In: Edge SB, Byrd DR, Compton CC (eds.). AJCC Cancer Staging Manual, 7th ed. New York, NY: Springer, 2010, with permission.
TABLE 27.2 Preoperative Staging System for Hilar Cholangiocarcinoma
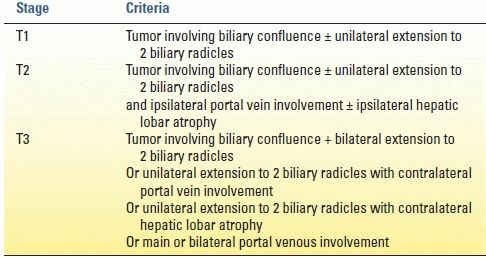
From Jarnagin WR, Fong Y, DeMatteo RP, et al. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 2001;234:507–519, with permission.
The role of fluorodeoxyglucose positron emission tomography (FDG-PET) in the preoperative staging of patients with carcinoma of the gallbladder or biliary tract is unclear. The putative benefits of FDG-PET to identify occult metastatic disease or advanced regional lymphadenopathy have been difficult to realize in clinical practice that utilizes timely, high-resolution cross-sectional imaging routinely.
Preoperative Planning
High-resolution MRI cholangiopancreatography and direct cholangiography (e.g., ERCP or percutaneous cholangiography) provide important anatomic information, including the location of the tumor and the biliary extent of disease, both of which are crucial in operative planning. High-quality cholangiograms are essential for accurately diagnosing the extent and level of bile duct involvement. High-performance MRCP has almost replaced endoscopic and percutaneous cholangiography as the initial preoperative assessment of hilar cholangiocarcinoma. MRCP not only identifies the tumor and the level of biliary obstruction but also may reveal obstructed and isolated ducts not appreciated at endoscopic or percutaneous study (Fig. 27.2). MRCP also provides information regarding the patency of hilar vascular structures, the presence of nodal or distant metastases, and the presence of lobar atrophy. Ultrasound, albeit operator dependent, is another useful noninvasive study during the preoperative planning process. When utilized by experienced centers, it often delineates tumor extent accurately. Ultrasound not only shows the level of biliary ductal obstruction but also can provide information regarding tumor extension within the bile duct and in the periductal tissues. Duplex ultrasound is firmly established as a highly accurate predictor of vascular involvement and technical resectability.
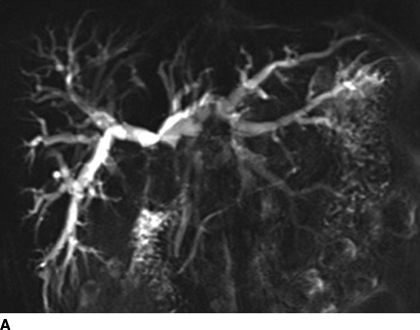
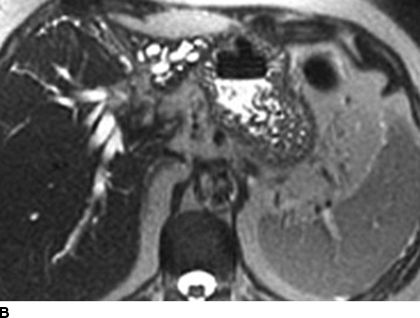
FIGURE 27.2 Coronal (A) and axial (B) MRCP images of a patient with hilar cholangiocarcinoma. The tumor involves the right and left hepatic ducts. The bile ducts in this study appear white. Extreme atrophy of the left hemiliver is apparent.
ERCP, when performed skillfully, provides useful ductal detail and can effectively drain functional liver segments prior to operative planning. Percutaneous cholangiography, while invasive, outlines the extent of intrahepatic bile duct involvement and has been the preferred study in the past for patients with hilar cholangiocarcinoma. Compared to endobiliary drainage, PTC may provide more reliable biliary drainage of the functional liver remnant when major hepatectomy is planned along with biliary resection. The benefits of preoperative biliary drainage have been difficult to prove, but most centers currently advocate for such intervention prior to resection of the extrahepatic bile ducts along with major hepatectomy.
The absolute indications for preoperative biliary drainage for jaundiced patients prior to pancreatoduodenectomy are not clear. Randomized controlled trials fail to demonstrate an improvement in postoperative outcomes for patients with periampullary cancers; however, most experts continue to advocate for preoperative endobiliary drainage for patients with deep jaundice, that is, serum total bilirubin greater than 15 mg/dL. Preoperative ERC with endobiliary drainage is the preferred approach in this situation.
For patients with hilar and intrahepatic cholangiocarcinoma who will require major hepatectomy, three-dimensional CT offers the capacity to generate volumetric models of the total liver, planned hepatic resection, and functional remnant liver volume. Since patients subjected to resection of more than 70% of functional liver parenchyma have substantially a higher risk of postoperative liver failure regardless of existing cholestatic liver disease, routine preoperative volumetry may help to identify patients who may be at considerable risk for postoperative hepatic failure and select candidates for preoperative portal vein embolization. The purpose of portal vein embolization is to increase the functional liver mass by inducing compensatory hypertrophy in the future liver remnant with the ultimate goal to minimize postoperative liver dysfunction that contributes to mortality substantially.
In right portal vein embolization, the volume of the left lobe increases by 130 cm3 on average within 2 weeks after embolization, and the estimated resection volume decreases by an average of approximately 10%. In the absence of randomized controlled trials, the indications for portal vein embolization remain somewhat arbitrary, but many centers utilize this technique preoperatively for patients undergoing extended right hepatectomy in the presence of underlying liver disease. In recent years, some centers have experimented with associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) as a perioperative technique to induce rapid hypertrophy of the future liver remnant and avoid postoperative liver dysfunction.
OPERATIVE INDICATIONS AND THERAPY
Staging laparoscopy for biliary tract malignancy should be considered for all patients with suspicious clinicopathologic findings for metastatic disease (e.g., remarkable elevations of serum CA 19-9 level, extreme weight loss, rapidly declining performance status, indeterminant nodules involving the liver or peritoneum). With an overall yield of 30%, staging laparoscopy should be utilized for all patients with gallbladder cancer and intrahepatic cholangiocarcinoma involving the liver capsule. Since the detection rate for occult metastases is stage dependent, most surgeons apply staging laparoscopy selectively for patients with extrahepatic bile duct cancer.
For gallbladder cancer in general, operative resection is indicated for patients with localized disease, that is, tumors limited to the gallbladder, liver bed, and regional lymph nodes. Peritoneal dissemination, extensive liver or bile duct (especially left hepatic duct) involvement, nodal metastases beyond the hepatoduodenal ligament (i.e., N2 disease, Fig. 27.3), left hepatic artery or portal vein encasement, or pancreatoduodenal infiltration should serve as contraindications for reasonable attempts at curative resection. Intraoperative ultrasound is a useful tool to further delineate spatial relationships between the tumor, liver, and surrounding hilar structures.
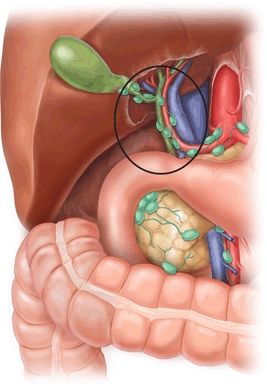
FIGURE 27.3 Regional lymph nodes associated with gallbladder cancer. The subhilar N1 level lymph nodes within the hepatoduodenal ligament are encircled. Lymph nodes outside of the circle (e.g., celiac, aortocaval, and mesenteric nodes) are considered N2 level. (Figure borrowed from Lillemoe K, Jarnagin WR (eds.). Hepatobiliary and pancreatic surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







