Step 1
Surgical Anatomy
Surgical Landmarks
- ♦
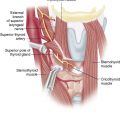
When planning the skin incision, the most important landmarks are the laryngeal prominence of the thyroid cartilage (which will help define the midline) and the isthmus of the thyroid (which will determine the position of the incision on the rostrocaudal axis) ( Fig. 7-1 ).
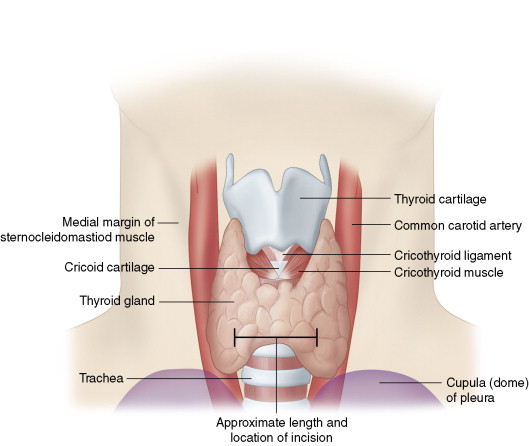
Figure 7-1
General Anatomic Considerations
- ♦
Identifying the recurrent laryngeal nerve (RLN) is not always necessary, but is sometimes helpful (and often unavoidable).
- ▴
The superior parathyroid glands tend to lie posterior to the coronal plane of the RLN, whereas the inferior parathyroid glands usually lie anterior to it. This relationship to the RLN is even respected in many cases of ectopia.
- ▴
If the dissection encroaches on the path of the RLN, it should be positively identified for the purposes of protection.
- ▴
- ♦
The inferior parathyroids are typically found within 1 cm of the lower pole, often associated with a fat lobule or cervical thymus.
- ▴
However, 3% descend into the upper anterior mediastinum (often within the thymus), 1% remain relatively cephalad due to a failure of descent, and 1% are intrathyroidal.
- ▴
- ♦
The superior parathyroids are typically found at the level of the cricothyroid junction, approximately 1 cm superior to the crossing of the inferior thyroid artery and the RLN, on the posterolateral surface of the thyroid. As with the inferior glands, expect to find an adherent fat lobule.
- ▴
When grossly enlarged (as in the case of an adenoma), the superior glands may descend in the tracheoesophageal groove to the level of the lower pole or even lower.
- ▴
Fewer than 1% are genuinely ectopic or intrathyroidal.
- ▴
- ♦
The gross characteristics of the glands (in both normal and pathologic states) are summarized in Surgery of the Thyroid and Parathyroid Glands (see reference list).
Step 2
Preoperative Considerations
Indications
- ♦
The indications for parathyroidectomy in patients with both symptomatic and asymptomatic primary hyperparathyroidism are clearly stated in the 2002 NIH Workshop guidelines ( Box 7-1 ).
BOX 7-1
2002 NIH Guidelines for Parathyroidectomy
Overtly symptomatic primary hyperparathyroidism
(nephrolithiasis, osteitis fibrosa cystica, neuromuscular syndrome)
Serum calcium 1 mg/dL above normal (i.e., > 11.5 mg/dL)
Hypercalciuria > 400 mg/24 hr
Osteoporosis (T-score < -2.5 at any site)
Creatinine clearance reduced 30% from age-matched controls
Age < 50 years
- ♦
Some authors consider these guidelines to be too restrictive and offer surgery to many patients who do not meet these criteria. Some have shown that many nonspecific symptoms never included in these guidelines improve dramatically after parathyroidectomy.
Preoperative Work-up
- ♦
In addition to the standard preoperative work-up appropriate for a patient undergoing general anesthesia, we obtain the following laboratory studies: serum calcium (total and ionized), phosphate, parathyroid hormone (PTH), magnesium, albumin, alkaline phosphatase, 25-hydroxy vitamin D and 1,25-dihydroxy vitamin D, 24-hour urinary calcium and creatinine excretion, and cross-linked telopeptides (optional).
- ♦
Imaging studies that are included as part of the work-up include the following::
- ▴
Tc 99 m sestamibi/ 123 I subtraction single photon emission computed tomography scan with computed tomography colocalization (the exact type of sestamibi scintigraphy may be institution-dependent).
- ▴
Neck ultrasound; parathyroid adenomas tend to manifest as hypoechoic masses ( Fig. 7-2 ).
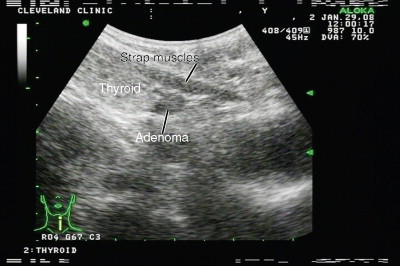
Figure 7-2
- ▴
Dual-energy X-ray absorptiometry (DEXA) is performed because of the high prevalence of osteopenia and osteoporosis in the hyperparathyroid population.
- ▴
Reoperative patients and those with a change in voice undergo fiberoptic laryngoscopy to evaluate vocal cord function.
- ▴
- ♦
Additional studies (e.g., cardiac and pulmonary testing) are obtained as needed, depending on the patient’s comorbidities.
- ♦
Patients are advised to avoid dehydration (drink at least 2 L of fluid per day), immobilization, and diuretics (especially of the thiazide class) if possible.
- ♦
Generally, patients do not need to modify their dietary calcium intake, but consumption well in excess of the RDA (1000 mg/day) has the potential to worsen hypercalcemia and lead to nephrolithiasis.
- ♦
On the day of surgery, the patient can be hydrated with normal saline solution (avoid any IV fluid that contains calcium, such as lactated Ringer’s solution).
- ♦
We do not routinely administer pre-incision antibiotics.
Reasons for Bilateral Exploration
- ♦
Bilateral exploration is the gold standard for identifying and treating multiglandular disease (MGD). Preoperative localizing studies are valuable tools for surgical planning, but cannot reliably rule out MGD.
- ▴
In our experience, even when sestamibi imaging and ultrasound are concordant on a single adenoma and the intraoperative PTH (IOPTH) drops appropriately, MGD would be missed on 9% to 16% of limited explorations (focal and unilateral).
- ▴
If only one preoperative localizing study is used or if the IOPTH is never sampled, the failure rate is even higher.
- ▴
- ♦
Bilateral exploration is safe, efficient, and extremely well tolerated by the patient.
- ▴
According to many studies, the complication rate in bilateral exploration is no higher than in limited explorations.
- ▴
The complication rate is significantly higher on reoperation as compared to a first-time operation. By identifying occult MGD, bilateral exploration may spare the patient from having to undergo reoperation, thereby avoiding this additional risk.
- ▴
The current literature indicates that postoperative pain is equivalent between these two approaches.
- ▴
Many studies have reported statistically significant differences in operative time between bilateral and limited exploration, but the actual time difference is often modest (as short as 10 to 20 minutes).
- ▴
We often perform our bilateral explorations through an incision comparable to those employed in limited explorations (2.5 cm).
- ▴
Bilateral exploration can be performed under “local” anesthesia (via a regional cervical block), but we do not routinely use this technique.
- ▴
Step 3
Operative Steps
Special Instrumentation
- ♦
Bilateral exploration can be performed with basic surgical equipment. Figure 7-3 shows the only “unique” instruments we use:
- ▴
A shielded, Teflon-tipped Bovie cautery ( a )
- ▴
A specially designed self-retaining retractor with biconcave, saddle-shaped retracting surfaces ( b )
- ▴
A McBurney retractor ( c )
- ▴
A very fine tipped Kelly clamp for dissection ( d )
- ▴
We run the Bovie cautery at 20 watts at the pinpoint setting.

Figure 7-3
- ▴
Positioning
- ♦
The patient is positioned supine, with the operating table in the “reflexed” orientation. The head is supported on a circular foam piece and the thoracic spine is elevated on a “beanbag” device, allowing the shoulders to fall back with the neck in gentle extension ( Fig. 7-4 ). The beanbag provides a much more stable platform for surgery than a rolled towel. The arms are tucked securely to the sides with the hands in the neutral position (thumbs up).
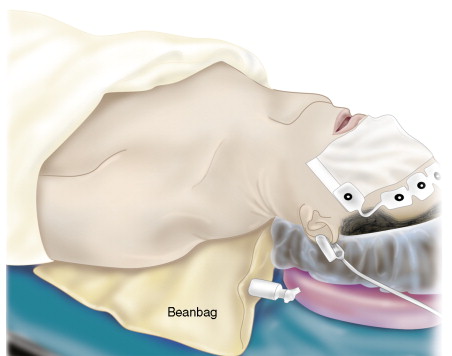
Figure 7-4
Marking and Incision
- ♦
Identify and mark the midline by palpating the laryngeal prominence of the thyroid cartilage ( Fig. 7-5 ).

Figure 7-5
- ♦
Position the incision over the lower half of the thyroid isthmus (see Fig. 7-1 ). Performing a neck ultrasound in the operating room can be helpful in locating this landmark.
- ♦
By folding the skin with a finger, a skin crease can be found in which to hide the incision.
- ♦
In experienced hands, a 2.5-cm incision can be used on select patients.
Subplatysmal Dissection
- ♦
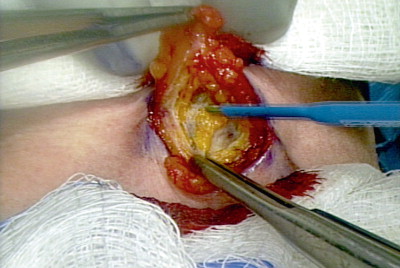
These are minimal platysma flaps, centered about the midline, and extended laterally just enough to expose the anterior strap muscles.
- ♦
Much of the dissection is done bluntly, by gently sweeping the “cold” Bovie cautery under the platysma ( Fig. 7-6 ). The flaps can be undermined with a judicious use of finger dissection as well.