Benign Soft Tissue Tumors
Timothy A. Damron
Gustavo De La Roza
Benign soft tissue tumors outnumber soft tissue sarcomas by approximately 100:1. In adults, lipomas are the most common soft tissue tumor; in children, hemangiomas are the most common. Recognition of these relatively more common benign tumors is important not only to avoid overtreatment but also to allow distinction from their malignant counterparts. Soft tissue tumors, both benign and malignant, are classified according to the purported cell of origin or resemblance, and the organization of this chapter will follow the latest World Health Organization (WHO) scheme in that regard.
Fatty Benign Soft Tissue Tumors
Lipoma
Lipoma is the most common soft tissue tumor in adults. However, because it is, soft tissue sarcomas are sometimes assumed to be lipomas, unnecessarily delaying the diagnosis. Hence, recognition of the distinction between benign lipomas and soft tissue sarcomas is very important.
Pathogenesis and Pathophysiology
Etiology is unknown.
More common in obese patients
Peak age: 40 to 60 (rare in children)
Multiple lipomas in 5%
Histopathology
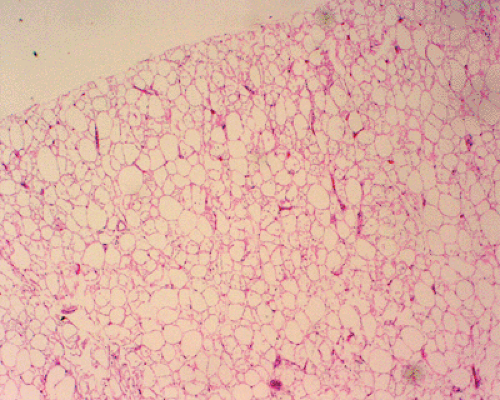
Lobules of mature adipocytes
Occasionally other areas of tissue formation
Bone = osteolipoma
Cartilage = chondrolipoma
Myxoid change = myxolipoma
Genetics
Chromosomal aberrations in up to 75%
Three patterns
12q13-15 aberrations
6p21-23 aberrations
Loss of material from 13q
Classification
Histologic variant subtypes have no prognostic significance.
Infiltrative
Intermuscular Versus Intramuscular
Intermuscular: easily shelled out between muscles
Intramuscular: two types within muscle
Well demarcated
Infiltrative: infiltrates and encases atrophic muscle fibers
Lipoma Arborescens
Subsynovial located lipoma
One type of intra-articular lipoma
Diagnosis
Clinical Features
Most common: painless mass with characteristic doughy feel
Most superficial lipomas are small (<5 cm).
Most deep lipomas are large (>5 cm).
Lipoma arborescens presents as articular swelling.
Radiologic Features
Superficial lipomas: difficult to see on radiographs or magnetic resonance imaging (MRI)
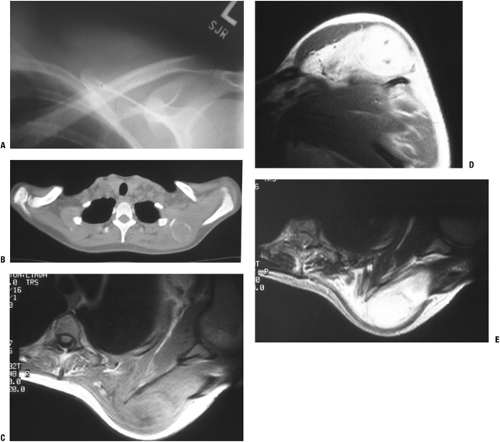
Deep lipomas (Fig. 11-1)
Fatty intramuscular shadow
Homogeneous fatty signal on all MRI sequences
No gadolinium enhancement
Occasional entrapped muscle fibers or fibrous strands
Lipoma arborescens
Fatty infiltration throughout affected synovium with fat-distended villi
Diagnostic Work-up
Most superficial lipomas are distinguished by their doughy characteristics on physical examination and do not warrant radiographic evaluation.
Larger or deep masses warrant plain radiographic and MRI evaluation, which is usually diagnostic.
Biopsy is rarely indicated.
Treatment
Surgical and Nonoperative Options
Superficial lipomas
Observation favored
Excision only if symptomatic
Deep lipomas
Observation if radiology identifies clearly as benign lesion (not atypical lipoma or liposarcoma)
Excision for most
Surgical Goals and Approaches
Marginal excision (complete excision through pseudocapsule)
Avoid transaction of nerves running within deep lipomas (piecemeal excision preferred).
Results and Outcome
Rarely recur following marginal excision
Lipomatosis
Lipomatosis is a diffuse systemic or regional overgrowth of mature adipose tissue that differs from normal fat only in
its distribution. Lipomatosis should be distinguished from lipomas, as the former conditions may be correctable by addressing the underlying condition and tend to recur after attempted excision.
its distribution. Lipomatosis should be distinguished from lipomas, as the former conditions may be correctable by addressing the underlying condition and tend to recur after attempted excision.
Pathogenesis and Pathophysiology
Etiology is poorly understood.
Possibly due to point mutations in mitochondrial genes
See Table 11-1 for epidemiology.
Histopathology: mature fat in poorly circumscribed lobules or sheets infiltrating surrounding tissues
Classification
Classified by distribution for idiopathic types (diffuse, pelvic, symmetric) or by etiology (steroid, HIV lipodystrophy)
Diagnosis
Notable accumulations of fat in affected areas may resemble neoplasms (see Table 11-1).
Radiologic studies document extent of fatty deposition.
Neither radiological evaluation nor biopsy is usually necessary to diagnosis the lipomatoses.
See Chapter 2.
Treatment and Outcome
Palliative surgery is rarely indicated unless life-threatening fat accumulation (such as that causing laryngeal compression in Madelung’s disease).
Correction of steroid lipomatosis follows lowering of steroid levels.
Table 11-1 Epidemiology and Clinical Features of Lipomatosis Subtypes | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Lipomatosis of Nerve (Lipofibromatous Hamartoma)
Lipofibromatosis, also referred to variously as lipofibromatous hamartoma, fibrolipomatosis, and intraneural lipoma, among other names, is a fatty and fibrous infiltrative process affecting the epineurium and leading to enlargement of the affected nerve. The median and ulnar nerves are most commonly affected.
Pathogenesis and Pathophysiology
Etiology is unknown.
Peak age: 10 to 40
Frequently evident at birth or early childhood
Female > male if macrodactyly present; male > female if none
Gross histopathology: yellow fibrofatty infiltration of nerve (Fig. 11-2)
Microscopic histopathology: epineurial and perineural fibrofatty infiltration isolating individual nerve bundles
Diagnosis
Clinical Features
Gradually enlarging mass with variable neurologic deficits
Median nerve or branches > ulnar nerve
Foot, brachial plexus less common sites
Macrodactyly in one third
Radiologic Features
MRI findings pathognomonic
Fusiform neural enlargement following branching pattern of nerve
Hypointense serpentine nerve bundles on both T1- and T2-weighted images
Variable intramuscular fatty deposition
Diagnostic Work-up
Because MRI is diagnostic, biopsy is usually not needed.
Treatment
Goal of surgical intervention is to decompress nerve if symptomatic.
Avoid attempted excision, which may damage nerve.
Lipoblastoma
Lipoblastoma is a tumor resembling fetal adipose tissue that occurs predominately in infants and may be localized (lipoblastoma) or diffuse (lipoblastomatosis). Since lipomas generally do not occur in this age group, lipoblastoma should be considered highly in the differential diagnosis of any tumor with fatty imaging characteristics in a child.
Pathogenesis and Pathophysiology
Etiology is unknown.
Peak age: birth to age 3; less common in older children
Males > females
Histopathology
Variable mixture of mature adipocytes and immature fat cells (lipoblasts)
Variable myxoid background with plexiform vascular pattern suggestive of myxoid liposarcoma
Pronounced lobular pattern and lack of atypia distinguishes lipoblastoma from liposarcoma
Genetics
8q11-13 rearrangement in most cases
Fusion gene products: HAS2/PLAG1, COL1A2/PLAG1
Classification
Solitary (lipoblastoma) versus diffuse (lipoblastomatosis)
Diagnosis
See Chapter 2 for diagnostic work-up.
Clinical Features
Sites: extremities predominate
Typically small (2 to 5 cm), superficial mass
Lipoblastomatosis often involves muscle as well.
Radiologic Features
Fatty signal characteristics
Bright on T1-weighted MRI, dark on fat-suppressed sequences, identical to surrounding fat
Indistinguishable from lipoma, well-differentiated liposarcoma (atypical lipoma) by radiology
Treatment and Outcome
Lipoblastoma: marginal en bloc excision
Lipoblastomatosis: wide surgical excision
Recurrence rare in lipoblastoma; up to 22% in lipoblastomatosis
Table 11-2 Histological Lipoma Variants | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Histologic Lipoma Variants
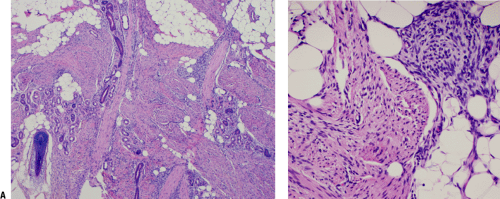
The histologic variants of lipoma are summarized in Table 11-2, and examples are shown in Figures 11-3 and 11-4.
Fibroblastic Benign Soft Tissue Tumors
Nodular Fasciitis
Nodular fasciitis is a tumor predominately of the upper extremity and neck region that is distinguished by its rapid growth and its tissue culture–like histology pattern.
Pathogenesis and Pathophysiology
Etiology: unknown, but history of trauma common
Epidemiology
Peak age: young adults, but may involve any age
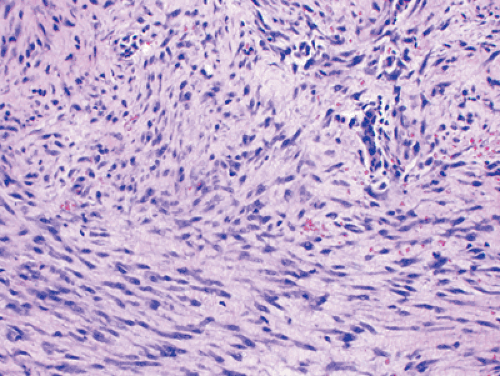
Histopathology (Fig. 11-5)
Plump, regular myofibroblasts
Frequent mitoses but not atypical mitoses
Tissue culture–like, “torn” or “feathery” appearance at low power
Prominent small vessels may resemble granulation tissue.
Nodular infiltrative pattern of organization
Extravasated red blood cells, chronic inflammatory cells, and even giant cells may be seen.
SMA and MSA positive
Desmin, cytokeratin, and S100 negative
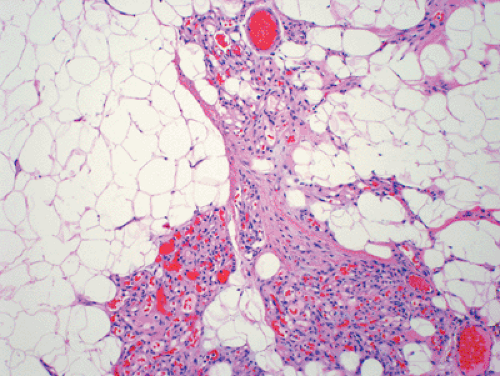 Figure 11-3 Angiolipoma composed of mature adipose tissue intermixed with numerous vascular channels. The vascularity is often more prominent in subcapsular areas. |
Genetics
Some clonality suggesting neoplastic nature demonstrated, but may represent artifact of culture conditions
Diagnosis
See Chapter 2 for diagnostic work-up.
Clinical Features
Subcutaneous >> intramuscular
Upper extremity, trunk, head and neck most common
Rapid growth is characteristic.
Clinical history usually <1 to 2 months
Pain and local tenderness common
Small size, usually <2 cm
Treatment and Outcome
Marginal excision
Rare recurrence should warrant reconsideration of diagnosis.
Proliferative Fasciitis and Myositis
These two processes are similar to nodular fasciitis in their rapid growth, predilection for the upper extremity, and plump myofibroblastic cells, but they are distinguished by the large ganglion-like cells that are also present. Proliferative fasciitis (PF) involves the fascia, while proliferative myositis (PM) involves the muscle.
Pathogenesis and Pathophysiology
Etiology is unknown, although a history of trauma may be elicited.
Peak age: middle-aged or older adults, older than nodular fasciitis
Much less common than nodular fasciitis
Histopathology
Two cellular types: plump myofibroblasts and ganglion-like cells
Plump myofibroblasts resemble those of nodular fasciitis.
Ganglion-like cells: large with one to three rounded nuclei, prominent nucleoli, and abundant cytoplasm
Numerous mitoses but not atypical mitoses
Infiltrative growth pattern (along fascial planes for PF and between muscle groups in PM)
Checkerboard pattern of infiltration between muscle fibers for PM
SMA and MSA positive
Desmin, cytokeratin, and S100 negative
Genetics
Similar to nodular fasciitis
Diagnosis
See Chapter 2 for diagnostic work-up.
Clinical Features
PF: upper extremity (especially forearm) > lower extremity > trunk
PM: trunk > shoulder girdle > upper arm > thigh
Rapid growth is characteristic.
Clinical history usually <1 or 2 months
Pain and local tenderness more common with PF
Small size, usually <5 cm
Radiologic Features
Nonspecific soft tissue mass
Treatment and Outcome
Marginal excision
Recurrence is rare.
Myositis Ossificans
Myositis ossificans is a benign reparative process characterized by bone formation within the soft tissues in response to trauma. On the one hand, it may simulate malignancy, but conversely, sarcomas that give a similar appearance may be mistaken for this benign, self-limited condition.
Pathogenesis and Pathophysiology
Trauma history elicited in up to 75% of patients; repetitive trauma in others
Peak age: young, physically active adults (rare in infants or elderly)
Males > females
Histopathology
Zonal proliferation with central fibroblasts and peripheral osteoblast-rimmed bone trabeculae
Progression from initially fibrous tissue to peripheral woven bone and then eventually lamellar bone
Peripheral ossification usually evident by 3 weeks
Mitoses frequent but no atypical mitoses
Diagnosis
See Chapter 2 for diagnostic work-up.
Clinical Features
Initial 1 to 2 weeks after injury: swollen, tender
From 2 to 6 weeks after injury: tenderness and pain resolve, and painless, very firm mass forms
Chronically, the mass becomes less prominent over time.
Any location in body susceptible to trauma
Most common locations: thigh, shoulder, buttock, elbow
Radiologic Features
Initial 1 to 2 weeks after injury: x-ray, computed tomography (CT), MRI shows soft tissue shadow, heterogeneous MRI signal with edema
From 2 to 6 weeks after injury: x-ray, CT best show peripheral rim of calcifications (Fig. 11-7)
Chronically, MRI eventually shows low-signal rim with fatty marrow signal centrally.
Treatment and Outcome
Observation is best, but marginal excision is appropriate if sufficiently symptomatic.
May recur if excised incompletely early in course
Elastofibroma
Elastofibroma (elastofibroma dorsi) is a unique process that occurs almost exclusively in a subscapular location in adults and is characterized by histologic evidence of elastic fibers.
Pathogenesis and Pathophysiology
Etiology is unknown, although repetitive trauma has been implicated.
Peak age in seventh and eighth decades (nearly always after age 50)
Females > males
Histopathology
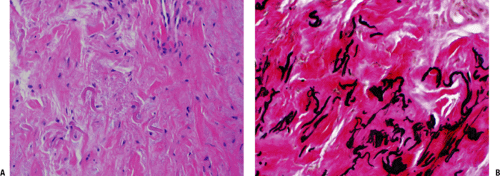
Low-cellularity collagenous tissue with intermixed elastic fibers (Fig. 11-8)
Immunohistochemistry positive for elastin
Genetics
Familial occurrence reported in Okinawa
Diagnosis
Clinical Features
Slowly growing mass, typically painless and nontender
May cause popping scapula or local discomfort
Classic location
Nearly exclusively subscapular, applied to chest wall at the lower portion of the scapula
Deep to latissimus dorsi and rhomboid major
Often attached to periosteum of ribs
Rare musculoskeletal sites: upper arm, hip
May be bilateral (especially subclinical) in up to one third
Radiologic Features
Fibrous and fatty elements create layered picture.
MRI may be highly suggestive (Fig. 11-9).
Fatty areas: bright areas on T1-weighted images, intermediate on T2-weighted images
Fibrous areas: similar to muscle
Diagnostic Work-up
Biopsy is generally recommended to confirm diagnosis, although the combination of classic location and radiologic appearance is highly suggestive.
Also see Chapter 2.
Treatment and Outcome
Marginal excision indicated for symptomatic patients but may be observed if asymptomatic and histologically proven
Rarely recurs after complete excision
Superficial Fibromatoses
The superficial fibromatoses include palmar fibromatosis (Dupuytren’s disease or contracture) and plantar fibromatosis (Ledderhose disease), both fibroblastic proliferations with infiltrative growth that are usually easily recognizable clinically and have a high rate of local recurrence if excised.
Pathogenesis and Pathophysiology
Etiology is multifactorial.
Familial component
Trauma
Associated diseases: epilepsy, diabetes, alcohol- induced liver disease
Peak age: adults with increasing frequency in advanced ages (rare before age 30)
Males >> females (3 to 4:1)
Ethnicity: highest incidence in northern Europe and in
those of northern European descent; rare in non-Caucasians
Pathophysiology is shown in Figure 11-10.
Diagnosis
Clinical Features
Palmar fibromatosis
Volar surface, 50% bilateral
Typical progression
Begins with firm painless nodule
Progresses to multiple nodules connected by tight cords (distinguished from pre-existing normal fascial bands)
Puckering of overlying skin
End-stage flexion contractures favoring ring and little fingers
Plantar fibromatosis
Plantar aponeurosis
Typical course
Begins with firm nodule adherent to skin
Often painful with shoe wear
Progressive enlargement may result.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree