Articular Cartilage Structure, Composition, and Repair
Peter J. Roughley
Thomas V. Smallman
Cartilage exists in the body as three types: hyaline cartilage, elastic cartilage, and fibrocartilage.
Hyaline cartilage: characterized by type II collagen and aggregating proteoglycan
Skeletal: articular cartilage, costal cartilage, and growth plate
Extraskeletal: larynx, trachea, bronchi, and nose
Elastic cartilage: characterized by preponderance of elastic fibers
Mainly in the ear and epiglottis
Fibrocartilage: characterized by type I collagen and lower proteoglycan content than hyaline cartilage
Skeletal: meniscus of the knee, annulus fibrosus of the intervertebral discs
This chapter focuses on articular cartilage, whose single cell, the chondrocyte, is charged with all aspects of maintaining the structure. Growth plate cartilage, meniscus, and intervertebral disc are covered in separate chapters.
The unique avascular and alymphatic nature of articular cartilage makes it very durable but with minimal capacity for repair. Its aneural structure makes it liable to injury in an overuse or post-traumatic situation, as pain is not necessarily perceived.
An understanding of the cartilage response to cumulative wear, trauma, inflammation, and infection will allow the clinician to rationally treat cartilage disorders.
Articular Cartilage
A fewjoints in the body are fibrous (cranial sutures, tibiofibular syndesmosis) or fibrocartilaginous (symphysis pubis). However, most of the joints in the body are synovial and consist of hyaline articular cartilage covering the surface of bones where they meet in mobile joints. In the healthy young individual, articular cartilage has a white, lustrous, and smooth appearance. It is composed of living cells of only one cell type, the articular chondrocyte, supporting and maintaining an extracellular matrix.
Table 20-1 Matrix and Cellular Features of Three Articular Cartilage Regions | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
Functions
To provide a smooth surface compatible with friction-less motion
To resist the compressive forces encountered across the joint under loading
This function is provided by the proteoglycan content.
Structure
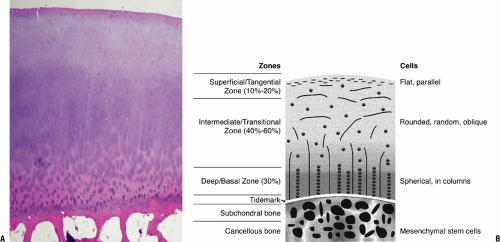
Morphologically, articular cartilage can be divided into three regions (Table 20-1), which can be distinguished by their differing orientation of type II collagen fibrils, orientation and cellular features of the chondrocytes, and histologic staining (Table 20-2).
Superficial collagen-rich tangential zone
Intermediate transitional zone
Deep/basal zone
Morphologic correlation of articular cartilage on Hema-toxylin and Eosin (H and E) stain (Fig. 20-1 A)
Eosin the acidic stain in the two part H and E stain; tends to stain most proteins red since most proteins are weak bases (negatively charged)
Hematoxylin, a basic stain, characteristically stains the nucleic acids of the nuclei of cells, and appears blue
This histologic correlate of staining in articular cartilage with these two standard stains distinguishes three regions:
Superficial zone, containing the negatively charged protein, collagen, picks up the eosin and stains red
Table 20-2 Histological Properties of Articular Cartilage
Histologic Stain
Fast green
Safranin O
Substance stained
Protein
Proteoglycans (polyanions)
Articular cartilage layer(s) stained
Tangential
Intermediate & deep
Bone/cartilage junction with denser collagen anchoring elements, as well as the subchondral bone also stains red
Intermediate and basal layers, rich in proteogly-cans, pick up the basic hematoxlyin stain, and thus appear blue
* Special stains (see Table 20-2)
More apparent visualization of these layers is apparent with a “fast green/Safranin O stain”
Fast green stains the collagen green and thus green will predominate in the superficial layer and the bone/cartilage junction
Safranin O, a cationic dye, bonds to the polyanions of the proteoglycan and imparts a red color to the intermediate and deep layers.
Composition (Table 20-3)
Mature articular cartilage contains about 5% of its volume as cells, the remainder being extracellular matrix.
There is normally no mineral, and organic material accounts for about 30% of the matrix, with the remainder being water.
About 60% of the organic material is collagen, 25% is proteoglycan, and the remainder is a variety of matrix proteins.
Nerve and Vascular Supply
Articular cartilage is characterized by having no nerves and no vascular system.
No nerves
Positive aspect: allows pain-free motion of the joints during normal use
Negative aspect: cartilage injury not perceived by the individual
No blood vessels
Nutrition and hydration for the tissue must arise from the synovial fluid by diffusion.
Clinical correlate: Cartilage exposed during surgery will rapidly dry, with resulting disruption of cell function, even leading to cell death, unless periodically bathed in fluid (every several minutes). The effect of drying on the matrix is not known.
No system for repair, as the usual microvascular source for cells in connective tissue repair is absent
Clinical correlate: Incisions in cartilage (e.g., during arthroscopy) do not heal.
Chondrocytes undergo anaerobic metabolism and survive for several days in the body following death.
Clinical correlate: allows some cell viability in fresh tissue bulk allografting
Table 20-3 Adult Articular Cartilage Composition | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Collagens
Types and Functions
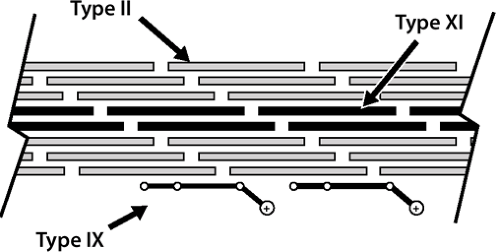
Collagens consist of three polypeptide chains that form a triple helix along at least part of their length.
They can be divided into fibrillar collagens (mainly types I, II, III, V, and XI) and nonfibrillar collagens (types IV, VI, VII, VIII, IX, and X).
The fibrillar collagens form the framework of connective tissues.
The fibrils consist of triple helical collagen molecules, arranged head to tail in linear arrays and side by side in a staggered manner (Fig. 20-2).
This staggered lateral arrangement gives the collagen fibril its characteristic cross-striated appearance when viewed in the electron microscope and contributes to its high tensile strength.
Nonfibrillar collagens serve both structural and non-structural functions.
Different connective tissues contain different collagen types, reflecting their varied functions.
Fibrillar collagens in cartilage: types II and XI collagen
Types II and XI collagen occur in the same fibrils (see Fig. 20-2).
Type II collagen: 90% to 95% of total collagen, 10% of weight of cartilage
Type XI collagen: 5% to 10% of total collagen
While fibrillar itself, serves to limit fibril diameter of type II
Nonfibrillar collagens in cartilage: type IX and X collagen
Type IX collagen
Resides on the surface of the fibrils
Facilitates interaction between the collagenous framework of the tissue and the interspersed proteoglycan
Type X collagen
Plays an integral role in the mineralization process in the growth plate
Site-specific immunostaining demonstrates localization that varies in noncalcified articular cartilage; animal work suggests that the presence of type X collagen may provide increased structural strength to normal articular cartilage.
In osteoarthritic and rheumatoid cartilage that is morphologically abnormal, there is expression of type X collagen; its role in normal articular cartilage is under investigation but has not yet been determined with certainty.
Fibrocartilage contains type I collagen as its predominant fibrillar collagen, in common with most other connective tissues.
Collagen Turnover
Physiologic conditions
Slow turnover: half-life of years
Net balance over time between formation and degradation
Disease states
Shift to more rapid turnover disrupts the balance.
If the rate of degradation exceeds formation, then loss of collagen and proteoglycan ensues and degeneration follows.
Proteoglycans
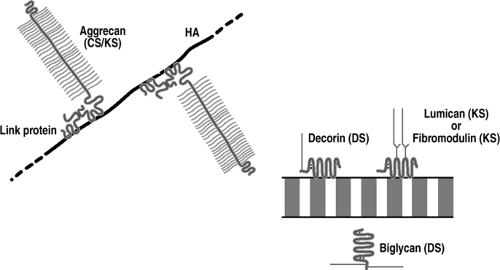
Proteoglycans are present in the extracellular matrix of all connective tissues, with the structure varying according to tissue.
They consist of a central protein core to which sulfated glycosaminoglycans (chondroitin sulfate, dermatan sul-fate, or keratan sulfate) are covalently attached.
In articular cartilage, it is the proteoglycans that serve the major role in accomplishing the primary function of the tissue in resisting compressive loads.
Aggregating Proteoglycans (Fig. 20-3)
Hyaline and elastic cartilages contain predominantly ag-grecan, one of the aggregating proteoglycans, which, by definition, aggregate or interact with hyaluronic acid.
Fibrocartilages do not contain as high an aggrecan content.
Structure
Many aggrecan molecules link to a central molecule of hyaluronic acid by a link protein that is devoid of sulfated glycosaminoglycans.
Aggrecan molecule
Long core protein with two types of glycosaminoglycan chains, chondroitin sulfate (100 per molecule) and keratan sulfate (60 per molecule), molecular weight 2,500,000 daltons, 90 percent carbohydrate
Aggrecan molecules account for 25% of the dry weight of cartilage.
Function
Proteoglycan aggregates provide the tissue with its turgid nature that resists compression.
Nonaggregating Proteoglycans (see Fig. 20-3)
All cartilages, in common with all soft tissues, also contain nonaggegating proteoglycans, which interact with collagen fibrils rather than hyaluronic acid, and function to stabilize the matrix.
These are decorin, biglycan, fibromodulin, and lumican.
They are much smaller than aggrecan and possess only a few dermatan sulfate (decorin and biglycan) or keratan sulfate (fibromodulin and lumican) chains.
They mediate the interactions between adjacent collagen fibrils, or with other matrix components.
Cartilage also contains perlecan, a heparan sulfate proteoglycan normally associated with basement membrane, whose function is unknown.
The types of cartilage proteoglycans are summarized in Table 20-4.
Biomechanics and Response to loading
The health of chondrocytes is closely related to joint loading and motion. Survival of the chondrocytes depends on adequate nutrition, and the passive diffusion of nutrients from the synovial fluid is aided by joint loading and motion. In general, dynamic (cyclic) loading is beneficial to matrix synthesis, whereas static loading is detrimental, causing a decrease in the synthesis of aggrecan and link proteins.
Cyclic Joint Loading
Promotes chondrocyte nutrition and function, stimulating the production and maintenance of the matrix
Cyclic loading clinical correlate: contributes to the beneficial effects of continuous passive motion (CPM)
Joint immobilization clinical correlate: Absence of this beneficial nutritional effect contributes to the cartilage atrophy observed upon prolonged joint underuse or immobilization.
Aggregating proteoglycans provide the articular cartilage with its resilience to compression, as compressive forces are counterbalanced by the focal increase in proteoglycan swelling potential (Fig. 20-4).
Serves to protect the chondrocytes from adverse forces
Compressibility is a function of the high hydrostatic pressure of cartilage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree