The contemporary practice of breast surgery requires an in-depth understanding of breast anatomy and imaging. Ultrasound of the breast has emerged over the past decade as an essential component of the evaluation of patients with breast disease and as an important tool in the operating room (OR).
Surgeons are natural imagers since they are use to thinking 3-dimensionally. Once they understand how ultrasound machines create images, what the images mean, and how the images correlate with benign and malignant breast conditions, they become “sonographic clinicians.” Surgeons synthesize the patient’s history with their physical, mammographic, ultrasound, and magnetic resonance imaging (MRI) findings into a clearer understanding of the probable diagnosis and a future course of action. In the OR, ultrasound is an important tool to facilitate wire-localization excisional biopsies or partial mastectomies. Ultrasound can be used to localize nonpalpable benign or malignant lesions in the OR or map the location of a cancer prior to starting a mastectomy.
There are literally thousands of drawings of the breast, its blood supply, lymphatic drainage, and regional nerves that can be found in anatomy books and textbooks on breast disease. The breast is composed of 15 to 20 lobes in most women. Within each lobe are numerous lobules and small ducts that join to form larger ducts, which then progress to form a single major lobar duct. The major lobar ducts come together beneath the nipple and widen as the lactiferous sinus (Figs. 30-1 and 30-2).
Figure 30-1
There are 3 zones within the breast. The premammary (PM) or subcutaneous fat zone contains Cooper ligaments (CL), and in some cases, a small number of peripheral ducts and lobules. The mammary zone (MZ) contains all of the central ducts and most of the peripheral ducts and lobules. The retromammary zone (RM) is the deepest of the 3 zones and contains only fat and ligaments. The anterior mammary fascia (AMF) and the retromammary fascia (RMF) encase the mammary zone. The lactiferous sinus (LS) is the dilated end of a main lobar duct. (Redrawn with permission from Stavros AT. Breast Ultrasound. Philadelphia, PA: Lippincott Williams, & Wilkins; 2004.)
In general, the central lobar ducts course away from the nipple in a radial pattern (Fig. 30-3). However, these ducts may be tortuous. Lobes vary in size and overlap each other. The central lobar ducts lie nearer the chest wall than the skin of the breast. Arising from the central lobar ducts are rows of lobules that are circumferential.1 Most of the lobules are oriented anteriorly or anterolaterally (Fig. 30-1).
The terminal ductolobular unit (TDLU) is the functional unit of the breast (Fig. 30-1). It is composed of a lobule and its terminal duct. Most lobules arise from smaller, more peripheral branch ducts. However, they may arise from larger central ducts, but rarely from the lactiferous sinus portion of main lobar ducts.2 Most ductal carcinomas are thought to arise within the TDLU or more centrally from an intraductal papilloma.
The breast is roughly elliptical in shape with an extension toward the axilla called the tail of Spence. The length and volume of the tail of Spence is variable, and its resection must not be missed during the performance of a mastectomy. The nipple is usually somewhat medial and inferior to the center of the breast. This asymmetry of the breast means that more lobular volume is in the upper outer quadrant with less lobular volume in the lower quadrants (Fig. 30-3). The greater number of breast cancers in the upper outer quadrant is at least partially due to the greater lobular volume in that quadrant plus the slower involution of tissue in that quadrant with aging.
The breast is a modified sweat gland that lies between 2 layers of the superficial fascia: a superficial layer beneath the dermis and a deep layer overlying the pectoralis fascia and chest wall (Fig. 30-2). There are 3 major zones within the breast: the premammary, mammary, and retromammary zones (Fig. 30-1).1 Most TDLUs lie within the mammary zone, but (importantly) a few TDLUs may extend into the Cooper ligaments and thus lie in the premammary (subcutaneous fat) zone.
The areola and nipple are covered by pigmented skin. The areola also contains sweat glands that lubricate it during lactation. The epithelium of the nipple skin (squamous) transitions through the outer ducts of the nipple to the epithelium of the lactiferous sinus and ductal system as 1 to 2 cell layers stuck to a thinner “basal membrane.” That basal membrane is then stuck onto myoepithelial cells, loose connective tissue, and fat.2
Ductal growth is stimulated by estrogen production. Full lobular development requires both estrogen and progesterone stimulation. Initial breast development begins with estrogen stimulation during the onset of puberty (around 11-14 years of age). Lobular proliferation and maturation do not occur until progesterone production stabilizes in late the teens or early 20s. Under age 20, connective tissue is the major component of the breast, representing over 50% of the total breast organ volume.
Pregnancy causes significant changes in the breast. In the first trimester, there is marked estrogenic stimulation of the breasts. During the second and third trimesters, there is a proliferation in both number and size of the TDLUs with an increase in the number of ductules (acini). Ultimately, nearly all of the fibrous tissue is replaced by glandular tissue during pregnancy.
After each pregnancy and lactation period, there is a regression of the lobules. The number of ductules within each TDLU decreases and the number of lobules also decreases. The volume of epithelial cells peaks at age 30 years, when it can be 30% of the total breast volume. Thereafter, it rapidly falls off. The percentage of fat in the breast increases from around 30% of the breast volume at age 30 to 65% at 75 years.2
There is a process of involution that takes several years after menopause. Very few mature lobules remain in the breast. Hormone replacement therapy (HRT) will alter the process of involution. Combined estrogen-progesterone HRT may cause postmenopausal persistence or development of mature lobules. Estrogen-alone HRT will not result in persistence of fully developed lobules, but may slow their regression.1 With normal involution of the breast, the volume of epithelial cells falls off after peaking at age 30 years (30%) to around 10% at 50 years and 5% at 75 years. It is replaced primarily by fat.2
The lymphatics of the breast drain primarily to the axilla and much less frequently to the internal mammary lymph nodes. Documented cases of drainage to the opposite axilla are quite rare. Most quadrants of the breast drain first superficially in a rich layer of lymphatics just superficial to the anterior mammary fascia, which flows to the periareolar plexus and then to the axilla. Injection of blue dye and/or a radioisotope in the subareolar region has proven to be a very accurate way to perform sentinel lymph node biopsies.
The axillary lymph nodes are classified by regions. Level I nodes are lateral and inferior to the pectoralis minor muscle. Level II nodes are deep to the pectoralis minor, while level III nodes lie medial and superior to the pectoralis minor. It is felt that lymphatic drainage can only reach the supraclavicular nodes after first passing through subclavian or deep jugular chains.
Intramammary lymph nodes are most common in the axillary segment or far lateral aspects of the breast.1 They can also occur in the far medial aspect of the breast or any quadrant. Intramammary lymph nodes can be sentinel nodes and are occasionally found to be the only positive lymph node with invasive cancers.
The blood supply to the breast is very rich. Medially, there are perforating branches of the internal mammary arteries. Additional blood supply comes from intercostal perforators and by lateral thoracic and thoracoabdominal branches of the axillary artery. A network of small arteries also connects the skin with the glandular portion of the breast via branches running with some Cooper ligaments.
The venous drainage of the breast is more variable than the arterial inflow. Much of the venous drainage of the breast parallels the lymphatic drainage with superficial branches that are not accompanied by arteries. The deeper arteries supplying the breast are accompanied by veins. Preserving more subcutaneous fat during mastectomy helps to insure flap viability by preserving the subcutaneous plexus of veins and small arteries that supply the skin of the breast.
Table 30-1 lists the generally accepted indications for breast ultrasound. In the United States, ultrasound is not yet indicated as a screening procedure for the detection of nonpalpable breast cancers. Mammography cannot distinguish between solid breast lesions and cyst. Ultrasound can differentiate these. Ultrasound identifies characteristics of a lesion that suggest whether it is benign or malignant. The evaluation and diagnosis of mammographically and/or MRI indeterminate lesions (both palpable and nonpalpable) is one of the most important uses of breast ultrasound.
| Palpable breast mass |
| Mammographically indeterminate lesion |
| Second-look ultrasound for MRI indeterminate lesion |
| Radiographically dense breast |
| Axillary lymph nodes |
| Pregnancy and lactation |
| Oncologic follow-up |
| After mastectomy |
| After breast-conserving surgery |
| Postoperative follow-up |
| Hematomas |
| Seromas |
| Prostheses |
| Ultrasound-guided interventions |
| Cyst aspirations |
| Biopsy of solid lesions |
| Preoperative needle localization |
| Axillary lymph node fine-needle aspiration |
| Peritumoral injection for sentinel lymph node biopsy |
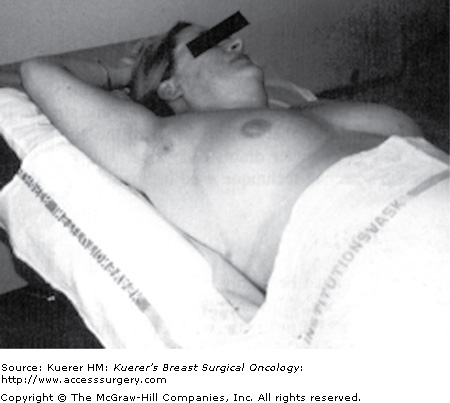
The patient is positioned for an ultrasound examination the same way she (he) is for a physical examination: supine with the ipsilateral hand behind the head (Fig. 30-4). This position allows the breast to be thinned to the greatest extent possible and the tissue planes of the breast are pulled parallel with the skin.
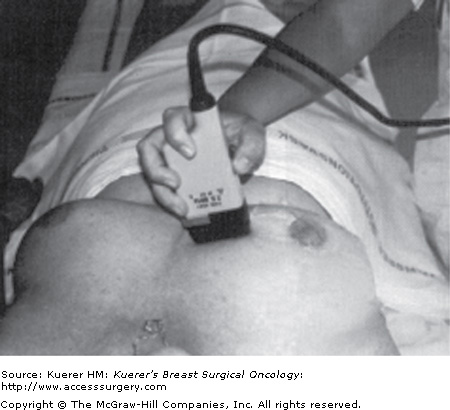
The patient is rolled medially (obliquely) to a degree that minimizes breast thickness in the quadrant being scanned. Lesions in the lateral quadrants require the greatest degree of oblique positioning, while lesions in the medial quadrants may be best scanned with the patient in a straight supine position (Fig. 30-5).
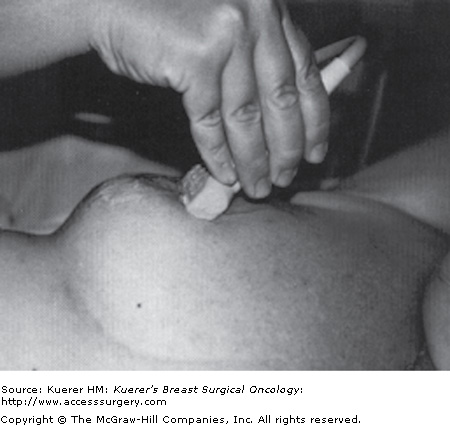
Imaging the nipple–areolar complex and its underlying ducts requires special maneuvering of the transducer because of the dense connective tissue in this area. The nipple–areolar complex may cause strong posterior shadowing as a result of the attenuation of the ultrasound beam. To avoid the shadowing problem, place the transducer adjacent to the nipple and angle the ultrasound beam into the retroareolar region (Fig. 30-6).
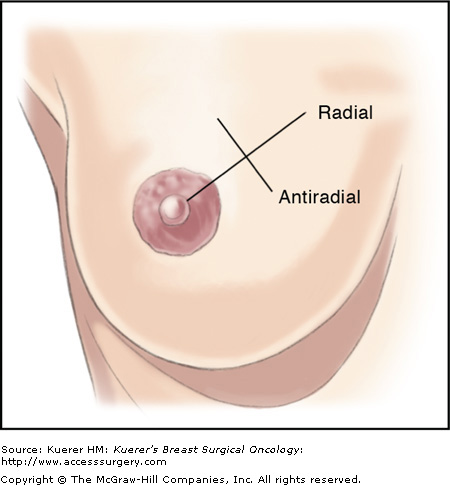
Most breast ultrasound examinations performed by surgeons target a specific clinical and/or mammographic finding. Such examinations are usually limited to the general area of abnormality. Solid and cystic lesions of the breast should be scanned in 2 planes (usually the radial and antiradial) (Fig. 30-7). The location should be documented using a clock notation, identifying both the hour location and the distance from the nipple.
When describing an ultrasound image, it is important for surgeons to use a standardized nomenclature. The following key words are essential for describing ultrasound images:
- Hyperechoic: A shade of gray that is bright white or brighter than surrounding structures; for example, Cooper ligaments of the breast are hyperechoic compared to the subcutaneous fat.
- Hypoechoic: A shade of gray that is dark or less bright than surrounding structures; for example, the subcutaneous fat of the breast is always hypoechoic.
- Anechoic: Without internal echoes (black); for example, a simple cyst is anechoic (black) because it has no internal echoes.
- Echogenic: A bright white appearance when scanning with a darker background; for example, microcalcifications in a cancer (which is usually hypoechoic) are very bright white dots.
- Homogeneous: Uniform shades of gray throughout a lesion; for example, the internal echoes of a fibroadenoma are usually homogeneous.
- Heterogeneous: Nonuniform shades of gray throughout a lesion; for example, the internal echoes of most cancers are heterogeneous.
The anatomic components of the breast and surrounding structures display characteristic sonographic features. These components include skin, subcutaneous fat, Cooper ligaments, superficial fascia, anterior mammary fascia, parenchyma, nipple–areolar region, retromammary fascia, retromammary space, pectoralis muscles, ribs, pleura, and intramammary and axillary lymph nodes (Fig. 30-2). Subcutaneous, retromammary, and intramammary fat are hypoechoic compared to glandular tissue.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree