- Increasing dietary allergies have been most apparent in children, with an estimated 5% demonstrating allergy to cow’s-milk protein.
- As dietary exposures in early life have broadened in the developed world, previously rare adverse reactions have become increasingly common.
- It is important to differentiate between the different forms of adverse reactions to foods, in particular between food intolerance and food allergy.
- There are two major classes of food allergic reaction: IgE-mediated and non-IgE-mediated. Within these classes, reactions may be divided clinically as localised or generalised.
- There is now increasing understanding of the mechanisms of oral tolerance to food antigens and of the importance of infectious exposures, particularly gut bacteria, in imprinting these in early life.
8.1 Introduction
In recent decades, dietary allergies have become increasingly common in privileged countries. This increase has been most apparent within the childhood population, with an estimated up to 5% of children demonstrating allergy to cow’s milk protein. In addition to this remarkable increase in frequency, there has been a change in patterns of presentation. As dietary exposures in early life have broadened for the children of the developed world, previously rare adverse reactions to antigens such as peanut and sesame seeds have become increasingly common.
There are significant geographical differences, dependent on patterns of dietary intake, including reports of anaphylaxis in response to birds’ nest soup in Singaporean infants. Early life exposures, which have changed substantially for developed-world children in the last 50 years, appear particularly important. Children born in disadvantaged conditions within the developing world have a much lower incidence of dietary allergies. Early life exposures appear to be a major determinant of allergic sensitisation, with genetic predisposition appearing to have an influence only after a certain threshold of improved material conditions is passed. Later in this chapter, the basic mechanisms of oral tolerance to dietary antigens underpinning such demographic change will be discussed. Because such tolerance is mediated by immunological mechanisms, there will be some overlap with concepts discussed in Chapter 17, on ‘Nutrition and Immune and Inflammatory Systems’.
First, it is important to differentiate between the different forms of adverse reactions to foods, particularly between food intolerance and food allergy. Only the latter is mediated by an immune response, whereas the former may be a consequence of a variety of non-immune mechanisms. There is often overlap in the symptoms displayed, and an accurate history is thus a vital component of the assessment of a patient suspected of adverse food reactions.
8.2 Food intolerance
This is by definition a reproducible adverse reaction to ingested food that is not mediated by immune hypersensitivity. This intolerance may be a response to the whole food, for example an aversion to its appearance, taste, or smell. It may be a consequence of an inability to process specific components of individual foods – the most common worldwide is lactose intolerance. Lactose is a disaccharide composed of glucose and galactose monosaccharides, which requires breakdown of the bond between the two component sugars by the intestinal enzyme lactase in order to allow their absorption. If lactase is deficient, the unabsorbed lactose passes down the gut and is fermented by gut bacteria, producing gas and acid by-products. This often causes uncomfortable abdominal distension and diarrhoea.
Humans are in fact the only mammal in which lactase persists into adult life, and such persistence has arisen by mutation since farming began. Many population groups, including those with ancestral origins in southern Europe and Africa, do not show lactase persistence and are thus lactose intolerant as adults. By contrast, in infancy low lactase expression is always abnormal, usually due to immune reactions in the intestine. Thus lactose intolerance in adults may be physiological, whereas in infants it is always pathological, and their food intolerance is caused by an underlying immune-mediated (allergic) mechanism.
Potentially more serious, and thankfully much rarer examples occur in infants with inborn errors of metabolism. In these disorders, lack of individual metabolic enzymes leads to damaging build-up of toxic metabolites of initially dietary origin. The best-known disorder is phenylketonuria, in which brain damage occurs if dietary phenylalanine is not excluded.
A third mechanism of food intolerance may occur when foodstuffs contain components with definite pharmacological effects, such as tyramine in cheeses and red wines. While most people are usually able to tolerate these, use of certain medications, such as monoamine oxidase inhibitors, may interfere with innate detoxication mechanisms and lead to potentially dangerous toxicity if these foods are consumed. Some people are sensitive to the histamines naturally occurring in strawberries, and rapidly develop rash or wheezing after eating them. Although these symptoms appear similar to immediate allergic reaction, they are mediated by non-immunological mechanisms and are thus due to food intolerance and not allergy.
Direct effects of foods are common, particularly those due to bacterial contamination. In most cases, this is sporadic, and clustering only occurs if large numbers of people eat the same contaminated food (e.g. wedding guests, airline passengers). However, the advent of modern food-handling practices increases the potential for very widespread transmission of such infections. This has occurred with recent outbreaks of life-threatening E. coli infections in Europe and North America. While considerable epidemiological detective work is necessary to trace the source of such epidemic food poisoning, there is usually little doubt of the involvement of food ingestion. This may not be so obvious if the foodstuff is contaminated by nonbacterial toxins or chemicals. In recent decades there have been epidemics of irreversible neural damage due to contamination of cooking oils in Spain and mercury poisoning in Japanese fishermen, and in neither case was it initially obvious that food contamination was to blame.
Detection of inborn errors of metabolism in early life is particularly important, as appropriate removal of dietary components in infancy can completely prevent serious brain damage. Recognition of the importance of early diagnosis led to the introduction of routine heel-prick testing of all newborn infants for phenylketonuria. Other rare disorders are not routinely tested for, and it is important to consider these diagnoses in any infants with early abnormal symptoms, including vomiting, poor feeding, enlarged liver and spleen, prolonged jaundice, failure to thrive, hypoglycaemia, floppiness, or impaired consciousness. The onset of such symptoms after weaning of a breast-fed infant to sucrose-containing foods may occur in hereditary fructose intolerance. Rapid diagnosis is the key, and delays usually occur because a metabolic cause is not included in the differential diagnosis of an unwell infant.
8.3 Food allergy
Allergies occur as a consequence of a breakdown in immunological tolerance. The immune system has continually to differentiate between myriad foreign molecules, recognising and responding to those which pose a threat to the organism – such as pathogens or their toxins – while remaining largely unresponsive (tolerant) to those necessary for survival and health – such as foods and the commensal bacterial flora in the intestine. Recent evidence suggests that the role of the bacterial flora in establishing immune tolerance is considerable, as discussed in Section 8.10.
Allergies are a varied group of conditions induced by inappropriate immune reactivity to foreign antigens; these are called allergens if they reproducibly cause symptoms on exposure. Food allergic responses by definition require an abnormal immunologically mediated reaction to ingested dietary antigens. However, there may well be overlap in the clinical manifestations of allergies and nonallergic food intolerance, and there is much potential for confusion if true allergy is mistaken for intolerance or vice versa. The nature of an allergic response is that initial sensitisation is required, and that the first exposure will not lead to obvious response, but that hypersensitivity reactions will occur on later challenge. Recent changes in the presentation of infant allergies suggest that such initial sensitisation may occur without such an obvious history. Indeed, even exclusively breastfed infants may sensitise to minute amounts of dietary antigen passing into their mother’s breast milk.
8.4 Types of food allergy
There are two major classes of food allergic reactions: IgE-mediated and non-IgE-mediated. The former are generally obvious, present soon after ingestion, and are thus relatively easy to investigate and diagnose (Box 8.1). They can be more violent than non-IgE-mediated reactions, and can cause death through anaphylaxis in severe cases. Non-IgE-mediated food allergies tend to present rather later and can be more subtle, but may be an important (and often unrecognised) cause of ill-health (see Table 8.1). The immunological basis of such reactions is discussed in more depth in Section 8.10.
Food-allergic reactions may also be divided clinically into those of quick onset (within minutes to an hour of food ingestion) and those of slow onset (taking hours or days). In general, quick-onset symptoms tend to be IgE-mediated and slow-onset symptoms non-IgE-mediated. However, this is by no means invariable, and many children with clear quick-onset responses to foods have a low or undetectable serum total IgE and absent food-specific IgE (radio allergosorbent test, RAST). This may be because there is local IgE response within the intestine that is not matched by systemic response. IgE responses may be compartmentalised, often being limited to the intestine and not occurring elsewhere. This may explain discordance between positive clinical responses and negative ‘allergy test’ results.
In a study of 120 children with multiple food allergies, we identified a significant increase of serum IgE in children who had early-onset symptoms compared to those with late-onset symptoms. What was notable was that the great majority (>90%) of those with early-onset symptoms additionally demonstrated late-onset symptoms. Both groups shared a pattern of immune deviation (including low IgG subclasses and IgA) consistent with reduced responses of the innate immune system to infectious exposures. This concords with data from several other countries, which link delayed immune maturation with early-life food allergies. These data suggest that there may be a consistent pattern of minor immunodeficiency associated with the process of sensitisation in early life, and that the manifestation of that sensitisation (quick- or slow-onset) may depend on whether a child has inherited a tendency to high IgE production. In other words, high IgE does not cause food allergy per se, but may determine how that allergy is expressed. Most of the early literature on food allergy focuses on IgE and quick-onset responses, which is understandable as it is so much more obvious to detect.
Table 8.1 Clinical manifestations in food-allergic responses.
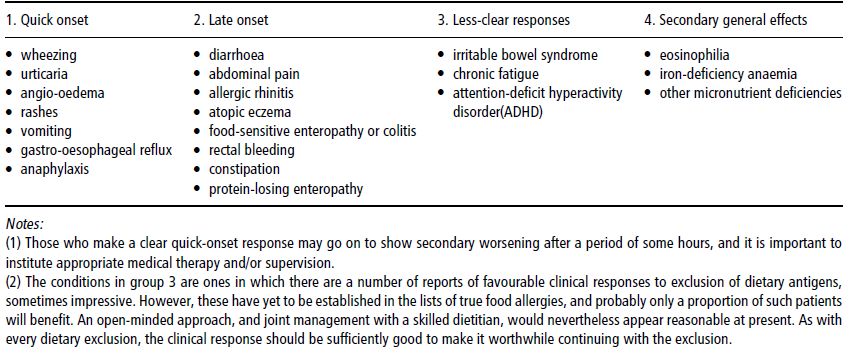
8.5 Patterns of food-allergic responses
Quick-onset symptoms
These often follow the ingestion of a single food, such as egg, peanut, or sesame. Within minutes, the sufferer may notice tingling of the tongue, and there may be a rapid development of skin rash, urticaria, or wheezing. Angioneurotic oedema, with swelling of the mucous membranes, can develop extremely fast, and the airway may become compromised. Anaphylactic shock may also occur, with dramatic systemic hypotension accompanying the airway obstruction.
Specific therapy for mild cases of immediate hypersensitivity would include antihistamines such as chlorpheniramine, together with inhaled bronchodilators as appropriate. It is notable that some patients can make a biphasic response, with a relatively modest initial reaction followed several hours later by a more profound and potentially life-threatening response, and thus care should be taken in the assessment to ensure that adequate instructions and therapy are administered before allowing the patient to go home. The presence of wheezing on examination should suggest caution, and a bronchodilator should certainly be prescribed, in many cases alongside a few days’ course of oral corticosteroids.
More severe reactions should be assessed very rapidly. Any evidence of airway obstruction or systemic hypotension warrants the immediate use of intramuscular adrenaline. If the patient has a preloaded adrenaline syringe pen, such as an EpiPen, this should be administered prior to urgent transfer to an appropriate medical setting, such as an Accident and Emergency department. There, it is likely that other measures, including oxygen, intravenous hydrocortisone, and intravenous or intramuscular chlorpheniramine, should be administered, and the requirement for inhaled bronchodilator therapy assessed. Supportive treatment for hypotension or cardiac dysrrhythmia may be required, and in the most severe cases the patient may need to be transferred to an intensive therapy unit.
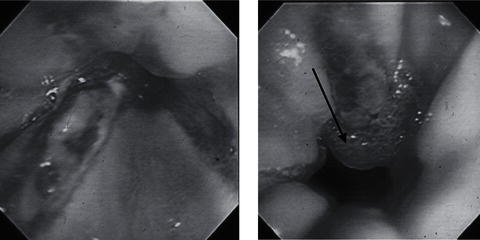
Figure 8.1Endoscopic appearances in food-allergic gastro-oesophageal reflux in infants. Both cases show endoscopic evidence of oesophagitis, with linear reddening of the mucosa and contactbleeding. The case on the right demonstrates an oesophageal ‘pearl’ (arrowed), which is found on histological assessment to contain multiple eosinophils. Both cases failed to resolve with conventional medical therapy, but normalised on exclusion diet.
In the follow-up of a patient who has had an immediate hypersensitive response to food antigens, a decision needs to be taken about the level of prophylaxis required, and whether or not to prescribe an adrenaline pen. Clearly the severity of the first response will inform this decision, and it is probably better to err on the side of caution if foods such as peanuts are implicated, because of their propensity for triggering particularly severe episodes. If there is doubt about the specific food involved, both skin-prick tests and specific IgE tests (RASTs) may be very helpful: these should be postponed for several weeks after an episode of anaphylaxis as they may be artefactually negative in the immediate aftermath of a severe reaction.
Late-onset symptoms
Symptoms may appear slowly and insidiously, and their true allergic nature may not be recognised (Table 8.1). These may include failure to thrive or chronic diarrhoea due to enteropathy or colitis, eczema, rhinitis, or rectal bleeding. As these are likely to be mediated by T cells in a delayed hypersensitive reaction, they may not be so clearly linked to food ingestion. More recently, the concept of food-allergic intestinal dysmotility has been suggested in paediatric patients, with dietary antigen (most commonly cow’s milk, soya, or wheat) inducing gastro-oesophageal reflux (Figures 8.1 and 8.2) or constipation (Figure 8.3). On gastrointestinal investigation of children with delayed responses, antigen-induced dysmotility or mucosal pathology such as small-intestinal enteropathy or colitis may often be found. However, it can be the case that both skin-prick tests and RASTs are negative but food elimination relieves all the symptoms and challenge with the food causes return of symptoms. If a child with severe eczema, failure to thrive, or intractable reflux has been transformed by an exclusion diet, it may be appropriate to defer such challenge until after a period of stability. Much more common is the problem of a patient with a genuine food-induced reaction who is refused appropriate treatment because the ‘investigations are negative’ – that is, specific IgE or skin-prick tests – and thus it ‘can’t be allergy’. Thankfully, recognition of non-IgE-mediated allergy is improving, although this does rely on clinical awareness of the diagnostic possibility.
Both types of reaction may occur individually or together: as mentioned above, a careful history will often uncover delayed in addition to immediate food reactions. The slow response is likely to be T cell-mediated, and the frequency of patients with low circulating immunoglobulins in the food-allergic population means that patients may have clinically important dietary responses without detectable antibodies.
Failure to detect specific antibodies does not rule out food allergy.
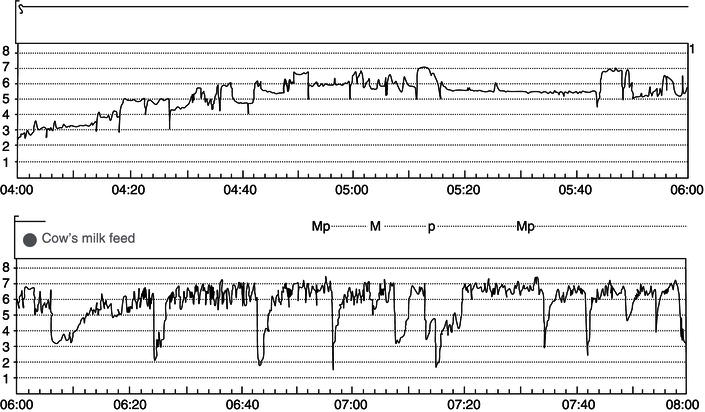
Figure 8.2 Evidence from a 24-hour pH study of the triggering of gastro-oesophageal reflux by cow’s milk in a 3-year-old child. Episodes of reflux are seen when the pH dips below 4. During the course of 24 hours, the reflux episodes only occurred after milk, and not after taking equal volumes of an amino acid formula.