Chapter Outline
Assessing the likelihood of acquired haemolytic anaemia 254
Assessment of the blood film and count in suspected acquired haemolytic anaemia 254
Immune haemolytic anaemias 255
Types of autoantibody 256
Methods of investigation 258
Drug-induced haemolytic anaemias of immunological origin 268
Drug-induced autoimmune haemolytic anaemias 269
Oxidant-induced haemolytic anaemia 270
Microangiopathic and mechanical haemolytic anaemias 271
Paroxysmal nocturnal haemoglobinuria 271
Acidified-serum lysis test (Ham test) 272
Acidified-serum lysis test with additional magnesium (modified Ham test) 273
Sucrose lysis test 274
Flow cytometric analysis of the glycosylphosphatidylinositol-linked proteins on red cells 274
Flow cytometric analysis of glycosylphosphatidylinositol-linked proteins on neutrophils 276
Paroxysmal nocturnal haemoglobinuria-like red cells 278
Summary of testing for paroxysmal nocturnal haemoglobinuria 278
Assessing the likelihood of acquired haemolytic anaemia
Haemolytic anaemia may be suspected from either clinical or laboratory abnormalities. Suggestive clinical features include anaemia, jaundice and splenomegaly. Other relevant clinical features that should be sought are a history of autoimmune disease, recent blood transfusion, recent infection, exposure to drugs or toxins, the presence of a cardiac prosthesis and risk of malaria. Previous clinical history and laboratory results will help to establish that the disorder is acquired. The basic laboratory investigations when a haemolytic anaemia is suspected are listed in Chapter 11 . In this chapter, tests are described that are more specific for the diagnosis of acquired haemolytic anaemia.
Assessment of the blood film and count in suspected acquired haemolytic anaemia
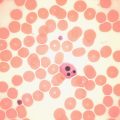
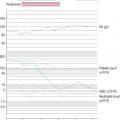
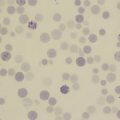
If haemolytic anaemia is suspected, a full blood count, reticulocyte count and blood film should always be performed. The blood count shows a reduced haemoglobin concentration (Hb) and, usually, an increased mean cell volume (MCV). The increased MCV is attributable to the fact that reticulocytes, which may constitute a significant proportion of total red cells, are larger than mature red cells. The abnormalities that may be detected in the blood film and their possible significance in acquired haemolytic anaemia are shown in Table 13-1 . Abnormalities detected in the blood film will direct further investigations. For example, a Heinz body preparation would be relevant if irregularly contracted cells were present, particularly if there appeared to be red cell inclusions. Similarly, a direct antiglobulin test (DAT) would be indicated if the blood film showed spherocytes. Various inherited forms of haemolytic anaemia enter into the differential diagnosis of suspected acquired haemolytic anaemia. Thus, spherocytes could be attributable to hereditary spherocytosis as well as to autoimmune or alloimmune haemolytic anaemia. Haemolysis with irregularly contracted cells could be attributable not only to oxidant exposure but also to an unstable haemoglobin, homozygosity for haemoglobin C or glucose-6-phosphate dehydrogenase (G6PD) deficiency.
| Morphological Abnormality Observed on Blood Film Examination | Type of Acquired Haemolytic Anaemia Suggested |
|---|---|
| Schistocytes | Fragmentation syndromes including microangiopathic haemolytic anaemia and mechanical haemolytic anaemia (but note that schistocytes can be due to dyserythropoiesis as well as haemolysis) |
| Spherocytes | Autoimmune, alloimmune or drug-induced immune haemolytic anaemia, paroxysmal cold haemoglobinuria, burns, Clostridium perfringens sepsis |
| Microspherocytes | Burns, fragmentation syndromes |
| Irregularly contracted cells | Oxidant damage, Zieve syndrome |
| Ghost cells, hemi-ghosts and suspicion of Heinz bodies | Acute oxidant damage |
| Marked red cell agglutination | Cold-antibody-induced haemolytic anaemia |
| Minor red cell agglutination | Warm autoimmune haemolytic anaemia, paroxysmal cold haemoglobinuria |
| Red cell agglutination plus erythrophagocytosis | Particularly characteristic of paroxysmal cold haemoglobinuria |
| Hypochromia, microcytosis and basophilic stippling | Lead poisoning |
| Erythrophagocytosis | Paroxysmal cold haemoglobinuria |
| Atypical lymphocytes | Cold-antibody-induced haemolytic anaemia associated with infectious mononucleosis or, less often, other infections |
| Lymphocytosis with mature small lymphocytes and smear cells | Autoimmune haemolytic anaemia associated with chronic lymphocytic leukaemia |
| Thrombocytopenia | Autoimmune haemolytic anaemia (Evans syndrome), thrombotic thrombocytopenic purpura, microangiopathic haemolytic anaemia associated with disseminated intravascular coagulation, paroxysmal nocturnal haemoglobinuria |
| Neutropenia | Paroxysmal nocturnal haemoglobinuria |
| No specific red cell features | Paroxysmal nocturnal haemoglobinuria |
Immune haemolytic anaemias
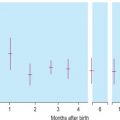
Acquired immune-mediated haemolytic anaemias are the result of autoantibodies to a patient’s own red cell antigens or alloantibodies in a patient’s circulation, either present in the plasma or completely bound to red cells. Alloantibodies may be present in a patient’s plasma and react with antigens on transfused donor red cells to cause haemolysis. Alloantibodies from maternal plasma may cause haemolytic disease of the newborn. Autoimmune haemolytic anaemia (AIHA) may be ‘idiopathic’ or secondary, associated mainly with lymphoproliferative disorders and autoimmune diseases, particularly systemic lupus erythematosus. AIHA may also follow atypical ( Mycoplasma pneumoniae ) pneumonia or infectious mononucleosis and other viral infections. Paroxysmal cold haemoglobinuria (PCH) also belongs to this group of disorders. Blood transfusion may induce red cell autoantibody formation. AIHA has been reported in pregnancy but is rare. Close observation throughout pregnancy has been recommended because immunoglobulin (Ig)G autoantibody can cross the placenta and can induce fetal haemolysis and haemolytic disease of the newborn. , AIHA has also been reported following allogeneic bone marrow transplantation and other haemopoietic stem cell transplantation in both adult and paediatric patients. Occasionally, drugs may give rise to a haemolytic anaemia of immunological origin that closely mimics idiopathic AIHA both clinically and serologically. This was a relatively common occurrence with α-methyldopa, a drug that is now used infrequently, but it also occurs occasionally with other drugs. A larger group of drugs give rise to an antibody that is directed primarily against the drug and only secondarily involves the red cells. This is an uncommon occurrence. Such drugs include penicillin, phenacetin, quinidine, quinine, the sodium salt of p -aminosalicylic acid, salicylazosulphapyridine and cephalosporins.
Types of autoantibody
The diagnosis of an AIHA requires evidence of anaemia and haemolysis and demonstration of autoantibodies attached to the patient’s red cells (i.e. a positive DAT, see p. 260). A positive DAT may also be caused by the presence of allo antibodies (e.g. owing to a delayed haemolytic transfusion reaction), so details of any transfusion in previous months must be sought.
Autoantibodies can often be demonstrated free in the serum of a patient suffering from an AIHA. The ease with which the antibodies can be detected depends on how much antibody is being produced, its affinity for the corresponding antigen on the red cell surface and the effect that temperature has on the adsorption of the antibody, as well as on the technique used to detect it. The autoantibodies associated with AIHA can be separated into two broad categories depending on how their interaction with antigen is affected by temperature: warm antibodies, which are able to combine with their corresponding red cell antigen readily at 37 °C; and cold antibodies, which cannot combine with antigen at 37 °C but form an increasingly stable combination with antigen as the temperature falls from 30–32 °C to 2–4 °C.
Cases of AIHA can similarly be separated into two broad categories according to the temperature characteristics of the associated autoantibodies: warm-type AIHA and the less frequent cold-type AIHA. , The relative frequencies of the two types are shown in Table13-2 . In unusual instances, both warm autoantibody and cold autoantibody are detected in the patient’s serum, and those cases are referred to as mixed-typed AIHA. ,
| Warm Autoantibodies (70–80%) |
|---|
| Idiopathic |
| Secondary |
| Malignancy: lymphoma, chronic lymphocytic leukaemia, ovarian dermoid cyst, Kaposi sarcoma |
| Autoimmune disorders: SLE, rheumatoid arthritis, ulcerative colitis |
| Infection: hepatitis C |
| Immunodeficiency: HIV infection, common variable immune deficiency, autoimmune lymphoproliferative disease |
| After allogeneic bone marrow or other haemopoietic stem cell transplantation |
| Cold Autoantibodies (10–15%) |
| Idiopathic |
| Secondary |
| Malignancy: lymphoma, chronic lymphocytic leukaemia, IgM gammopathy |
| Waldenström macroglobulinaemia |
| Infection: atypical or Mycoplasma pneumoniae infection, infectious mononucleosis |
| After allogeneic bone marrow or other haemopoietic stem cell transplantation |
| Paroxysmal Cold Haemoglobinuria (1–2%) |
| Idiopathic |
| Secondary |
| Viral infection, syphilis |
| Combined Warm and Cold Autoantibodies (Mixed Type AIHA) (6–8%) |
| Idiopathic |
| Secondary |
| SLE, lymphoma |
| Drug-induced AIHA |
Warm autoantibodies
The most common type of warm autoantibody is an IgG antibody, which behaves in vitro very similarly to an Rh alloantibody; indeed, many IgG autoantibodies have a mimicking Rh specificity.
Frequently, patients with warm-type AIHA have complement adsorbed onto their red cells and the red cells are therefore agglutinated by antisera specific for complement or a complement component such as C3d. In these cases, the complement is probably not being bound by an IgG antibody but is on the cell surface as the result of the action of small and otherwise undetected amounts of IgM autoantibody.
However, IgG can fix complement and sometimes patients with warm-type AIHA appear to have a positive DAT with complement components only on the red cell surface. Similar results (positive DAT with complement only) are seen in some patients with no evidence of increased red cell destruction, due to binding of circulating immune complexes to the red cells.
Warm autoantibodies free in the patient’s serum are best detected by means of the indirect antiglobulin test (IAT) or by the use of enzyme-treated (e.g. trypsinised or papainised) red cells. (Antibodies that agglutinate unmodified cells directly in vitro are seldom present.) Not infrequently, antibodies that agglutinate enzyme-treated cells, sometimes at high titres, are present in the sera of patients in whom the IAT using unmodified cells is negative ( Table 13-3 ). , Occasionally, too, they are present in the sera of patients in whom the DAT is negative.
Antibodies in serum that can be shown to lyse (rather than simply agglutinate) unmodified red cells at 37 °C in the presence of complement (warm haemolysins) are rarely demonstrable. If they are present, the patient is likely to suffer from extremely severe haemolysis. Antibodies in serum that lyse as well as agglutinate enzyme-treated cells but do not affect unmodified cells are, however, quite common. Their specificity is uncertain – they are not anti-Rh – and their presence is not necessarily associated with increased haemolysis in vivo.
Cold autoantibodies
Cold autoantibodies are nearly always IgM in type. In vivo the majority do not cause haemolysis, although a minority can cause chronic intravascular haemolysis, the intensity of which is characteristically influenced by the ambient temperature. The resultant clinical picture is generally referred to as the cold haemagglutinin syndrome or disease (CHAD). Haemolysis results from destruction of the red cells by complement that is bound to the red cell surface by the antigen–antibody reaction, which takes place in the blood vessels of the exposed skin where the temperature is 28–32 °C or less. The cold autoantibody in CHAD is monoclonal because this syndrome is the result of a low-grade lymphoproliferative disorder.
The red cells of patients suffering from CHAD characteristically give positive antiglobulin reactions only with anticomplement (anti-C′) sera. (The C′ notation is used to distinguish anticomplement antibodies from anti-C antibodies of the Rh system.) This is because of the presence of red cells that have irreversibly adsorbed sublytic amounts of complement; it is an indication of an antigen–antibody reaction that has taken place at a temperature below 37 °C. The complement component responsible for the reaction with anti-C′ sera is the C3dg derivative of C3 (see p. 448).
In vitro, a cold-type autoantibody will often lyse normal red cells at 20–30 °C in the presence of fresh human complement, especially if the cell–serum mixture is acidified to pH 6.5–7.0; it will usually lyse enzyme-treated red cells readily in unacidified serum and agglutination and lysis of these cells may still occur at 37 °C. Most of these cold-type autoantibodies have anti-I specificity (i.e. they react strongly with the vast majority of adult red cells and only weakly with cord-blood red cells). A minority are anti-i and react strongly with cord-blood cells and weakly with adult red cells. Rarely, the antibodies have anti-Pr or anti-M specificity and react with antigens on the red cell surface that are destroyed by enzyme treatment.
Combined warm and cold autoantibodies
In approximately 7% of cases with AIHA, warm IgG antibody and cold IgM autoantibody are simultaneously detected in the patient’s serum. , These cases are referred to as ‘combined warm and cold AIHA’ or mixed-type AIHA. The serological characteristics in these patients are the presence of IgM cold autoantibody with a high thermal amplitude (reacting at or above 30 °C) in association with a warm IgG autoantibody. In some cases, high-titre cold agglutinins (> 1024 at 4 °C) were reported, , and in others the cold agglutinin titre were reported as > 64 at 4 °C. , This can be further classified into idiopathic or secondary, the latter often associated with systemic lupus erythematosus or lymphoma. ,
Another quite distinct, but rarely encountered, type of cold antibody is the Donath–Landsteiner (D–L) antibody. This is IgG and has anti-P specificity. The clinical syndrome the antibody produces is PCH.
PCH is caused by a biphasic IgG autoantibody, usually with anti-P specificity, and is commonly seen as an acute condition in children. This antibody binds to the red cells in the cold but activates complement and causes haemolysis on rewarming to 37 °C. Cases may be idiopathic or secondary to acute viral infection in children. Other tests of value in the diagnosis of PCH are discussed on p. 266.
The DAT is positive for complement only. A negative antibody screen by the standard IAT at 37 °C is a common finding in a suspected case of PCH because of the low thermal amplitude of the autoantibody. If the antibody investigation is carried out at a lower temperature in PCH cases, panreactive cold antibodies may be detected because the majority of autoantibodies show anti-P specificity with thermal amplitude range up to 15–24 °C. Usually the antibody titre is low (< 64), even when investigated at 4 °C.
The clinical, haematological and serological aspects of the AIHAs have been summarised by Dacie and others.
AIHAs are classified as indicated in Table 13-2 . Some of the characteristics of IgG, IgM and IgA antibodies are listed in Table 13-4 .
| IgG | IgM | IgA | |
|---|---|---|---|
| Molecular weight (daltons) | 146 000 | 970 000 | 160 000 |
| Sedimentation constant (s) | 7 | 19 | 7 |
| Number of heavy-chain subclasses | 4 | 1 | 2 |
| Cross placenta | Yes | No | No |
| Cause activation of complement | Yes | Yes | No |
| Cause monocyte/macrophage attachment | Yes | No | No |
| Number of antigen-binding sites | 2 | 5 or 10 | 2 |
| Types of AIHA produced | Warm; PCH | Usually cold | Warm |
Methods of investigation
Many of the methods used in the investigation of a patient suspected of suffering from AIHA are described in Chapter 21 . Detailed description is given here of precautions to be taken when collecting blood samples from patients and of methods of particular value in the investigations.
Collection of samples of blood and serum
To determine the true thermal amplitude or titre of cold agglutinins requires that the blood sample is collected and maintained strictly at 37 °C until serum and cells are separated. This can be achieved by collecting venous blood (clotted and ethylenediaminetetra-acetic acid (EDTA)–anticoagulated samples) and keeping it warmed at 37 °C – ideally in an insulated thermos, but usually, in practice, by placing the sample tube in a beaker containing water at 37 °C.
The red cells are available for antibody elution and the serum can be examined for free antibody or other abnormalities. The clotted sample should then be centrifuged to separate the serum at 37 °C (e.g. in an ordinary centrifuge into the buckets of which has been placed water warmed to 37°–40 °C). The EDTA sample is used for the DAT and other tests involving the patient’s red cells. If the autoantibody in a particular case is known to be warm in type, the blood may be separated at room temperature; otherwise, as already indicated, separation should be carried out at 37 °C. When samples are sent by post, it is best to send separately: (1) serum (separated at 37 °C), and (2) whole blood added to acid–citrate–dextrose (ACD) or citrate–phosphate–dextrose (CPD) solution. Sterility must be maintained.
Storage of samples
Samples of a patient’s blood, while keeping quite well in ACD or CPD at 4 °C, are more difficult to preserve than normal red cells. In particular, if marked spherocytosis is present, considerable lysis develops on storage. However, satisfactory eluates can be made from washed red cells that have been frozen at –20 °C for weeks or months.
The patient’s serum should be stored at –20 °C or below in small (1–2 ml) volumes. If complement is to be titrated and the titration is not performed immediately, the serum should be frozen as soon as practicable at –70 °C or below.
Scheme for serological investigation of haemolytic anaemia suspected to be of immunological origin
It is important to consider which are the most useful tests to carry out and the order in which they should be done. A suggested scheme has been set out in the form of answers to questions. Whereas some information may be helpful in classifying the type of AIHA, the single most important practical consideration is to determine whether, in addition to an autoantibody, there is any underlying alloantibody present. This should be identified before transfusion is undertaken to avoid a delayed haemolytic transfusion reaction that would compound existing haemolysis.
- 1.
Are the patient’s red cells ‘coated’ by immunoglobulins or complement (indicating an antigen– antibody reaction)?
Perform a DAT using a polyspecific ‘broad-spectrum’ reagent, which contains both anti-IgG and anti-C′. (If the DAT is negative, it is unlikely, although not impossible, that the diagnosis is AIHA. See DAT-negative AIHA, p. 261).
- 2.
If the DAT is positive, are immunoglobulins or complement adsorbed to the red cells?
Repeat the DAT using monospecific sera (see p. 453) (i.e. anti-IgG and anti-C3d).
- 3.
If immunoglobulins are present on the red cells, is there antibody specificity?
Prepare eluates from the patient’s red cells. Test these later (see item 6).
- 4.
What is the patient’s blood group?
Determine the patient’s ABO, RhD and Kell type. The Rh phenotype is particularly important in warm-type AIHA; other antigens must be determined if alloantibodies are to be differentiated from autoantibodies (see p. 447).
- 5.
Is there free antibody in the serum? How does it react and at what temperatures and by what methods can it be demonstrated? Is there any underlying alloantibody present?
Screen the serum with two or three red cell suspensions suitable for routine pretransfusion antibody screening (see p. 480) looking for agglutination and lysis at 37 °C by the IAT (see p. 453). If positive, identify the antibody using an antibody identification panel.
- a.
If an alloantibody is identified, blood lacking the corresponding antigen must be selected for transfusion.
- b.
If no alloantibody is identified in the serum or plasma, it is safe to assume there is no alloantibody present unless the patient has been transfused in the last month; in the latter case, a red cell eluate is required because an alloantibody may be bound to the recently transfused cells and there may not be free antibody detectable in the serum/plasma.
- c.
If the autoantibody is panreacting (i.e. is reacting against all panel cells), antibody adsorption tests are needed to remove the autoantibody so as to identify any underlying alloantibody. If the patient has not had a transfusion within the previous 3 months, a ZZAP autoadsorption test is appropriate (see p. 263). If the patient has had a transfusion within the last 3 months, differential alloadsorption tests are needed. However, if the patient has had a transfusion within the last month, an eluate is required, irrespective of results of adsorption tests.
- 6.
If there is a warm autoantibody, what is the specificity of the autoantibody?
Test the serum also at 20 °C against antibody-screening cells to show whether cold or warm antibodies (or a mixture of the two) are present in the serum. Test the eluate against the antibody identification panel of red cells by IAT and by using enzyme-treated red cells (see p. 451). Titration of autoantibody may be useful in the presence of a strong alloantibody. Titrate the serum/plasma by the methods that have given positive results in the screening test using the same panel of red cells (see item 5a).
- 7.
If there is a cold antibody:
- a.
Has the antibody any specificity? Is it an autoantibody or an alloantibody? What is its titre?
- b.
What is the thermal range of the antibody? Test the serum/plasma against a panel of O cells, O cord cells and patient’s own cells at 20 °C. If an autoantibody is found, titrate at 4 °C with ABO-compatible adult (I) cells, cord blood (i) cells, the patient’s cells and adult (i) cells (if possible):
- i.
Determine the highest temperature at which autoagglutination of the patient’s whole blood takes place (see p. 266).
- ii.
Titrate the patient’s serum/plasma at 20 °C, 30 °C and 37 °C with pooled O adult cells, O cord cells, patient’s own cells and the panel of O cells. If there was any agglutination or lysis at 37 °C in the screening test (item 5), titrate with the appropriate cells at this temperature.
- iii.
If PCH is suspected, carry out the direct and two-stage indirect Donath–Landsteiner tests (see p. 266).
- i.
- a.
- 8.
Is there is a mixture of both warm autoantibody and cold autoantibody?
The diagnosis of mixed-type AIHA can only be made after appropriate characterisation of the serum autoantibodies. The serological characteristic in these cases is the presence of a cold IgM antibody with a high thermal amplitude (reacting at or above 30 °C) in association with a warm IgG autoantibody. ,
- 9.
Is a drug suspected as the cause of the haemolytic anaemia?
- a.
If a penicillin-induced haemolytic anaemia is suspected, test for antibodies using cells pre- incubated with penicillin (see p. 269).
- b.
If haemolysis induced by other drugs is suspected, add the drug in solution to a mixture of the patient’s serum, normal cells and fresh normal serum (see p. 270). Look for agglutination of normal and enzyme-treated cells and use the IAT.
- a.
- 10.
Are there any other serological abnormalities?
Consider carrying out the following tests: serum protein electrophoresis and quantitative estimation of immunoglobulins, estimation of complement, tests for antinuclear factor, a screening test for heterophile antibodies (infectious mononucleosis screening test) and a test for mycoplasma antibodies.
This suggested scheme summarises what may be done by way of serological investigation of a patient suspected of having AIHA. Close collaboration between clinician and laboratory helps in deciding what tests should be done in any particular case.
Detection of incomplete antibodies by means of the direct antiglobulin (coombs) test
Principle.
As already described, the DAT involves testing the patient’s cells without prior exposure to antibody in vitro. For the investigation of cases of AIHA, antiglobulin reagents specific for IgG, IgM, IgA, C3c and C3d can be used.
Precautions.
A blood sample in EDTA is preferred. (If a clotted sample is used, complement could be bound by normal incomplete cold antibody and give a false-positive result with anti-C3d.) Certain precautions are necessary when investigating a patient with possible AIHA. If a cold-reacting autoantibody is present, the patient’s red cells should be washed four times in a large volume of saline (throughout this chapter, ‘saline’ refers to 9 g/l NaCl buffered to pH 7.0), warmed to 37 °C to wash off cold antibodies and obtain a smooth suspension of cells. There is no risk of washing off adsorbed complement components. However, the washing process should be accomplished as quickly as possible and the test should be set up immediately afterward because bound warm antibody occasionally elutes from the cells when they are washed and false-negative results may be obtained. If for any reason the washing process has to be interrupted once it has begun, the cell suspension should be placed at 4 °C to slow down the dissociation of the antibody.
Method.
A spin tube technique, as described on p. 454, is recommended.
Make a 2–5% suspension of red cells that have been washed four times in saline. Add 1 volume (drop) of the cell suspension to 2 volumes (drops) of antiglobulin reagent. Centrifuge for 10–60 s. Refer to reagent manufacturer’s instructions for specific details.
Examine for agglutination after gently resuspending the button of cells. A concave mirror and good light help in macroscopic readings. If the result appears to be negative, confirm this microscopically.
Each DAT or batch of tests should be carefully controlled as previously described.
Check negative results with the polyspecific antihuman globulin (AHG) or anti-IgG reagents by the addition of IgG-sensitised cells and anti-C′ by the addition of complement- coated cells.
Direct antiglobulin test using column agglutination technology
A card of several microtubes enables multiple sample testing. The microtubes contain a solid-phase matrix and the antiglobulin reagent to which the patient’s red cells are added. During centrifugation, unagglutinated cells pass to the tip of the tube, but agglutinates fail to pass through the gel, which acts as a sieve. As the antiglobulin reagent is already present in the microtubes, no washing or addition of IgG-coated cells to negative tests is required. Refer to individual manufacturer’s instructions for details of methods for performing the tests.
Significance of positive direct antiglobulin test
A positive DAT plus anaemia does not necessarily mean that the patient has autoimmune haemolysis. , The causes of a positive test include the following:
- 1.
An autoantibody on the red cell surface with or without haemolytic anaemia
- 2.
An alloantibody on the red cell surface, as for example in haemolytic disease of the newborn or after an incompatible transfusion
- 3.
Antibodies provoked by drugs adsorbed to the red cell (see p. 269)
- 4.
Normal globulins adsorbed to the red cell surface as the result of damage by drugs (e.g. some cephalosporins)
- 5.
Complement components alone:
- a.
About 10–11% of patients with warm AIHA have red cells with a positive DAT as a result of C3 coating alone
- b.
Cold haemagglutinin disease/paroxysmal cold haemoglobinuria
- c.
Drug-dependent immune haemolytic anaemia (complement-induced lysis)
- d.
Adsorption of immune complexes to the red cell surface. This may be the mechanism of the (usually weak) reactions that are found in approximately 8% of hospital patients suffering from a wide variety of disorders (see below)
- a.
- 6.
Passive infusion of alloantibodies in donor plasma/derivatives that react with recipient’s red cells:
- a.
Transfusion of group O platelets with high-titre anti-A, -B to group A or B recipient
- b.
Administration of intravenous immunoglobulin, which may contain ABO or anti-D antibodies. In one study of patients treated with intravenous immunoglobulin after bone marrow transplantation, 49% of recipients developed a positive DAT and 25% had a positive antibody screen (passively transfused anti-A, -B, -D or -K) of short duration (2–5 days)
- a.
- 7.
Administration of anti-D for the treatment of autoimmune thrombocytopenia purpura
- 8.
Antibodies produced by passenger lymphocytes in solid organ transplant and bone marrow transplantation ,
- 9.
Nonspecific binding of immunoglobulins to red cells in patients with hypergammaglobulinaemia or multiple myeloma and in recipients of antilymphocyte globulin and antithymocyte globulin. Szymanski et al . used an AutoAnalyser and used Ficoll and polyvinylpyrrolidone (PVP) to enhance agglutination by an anti-IgG serum highly diluted (usually to 1 in 5000) in 0.5% bovine serum albumin. In this sensitive system, the strength of agglutination was positively correlated with the serum γ-globulin concentration, being subnormal in hypogammaglobulinaemia and supranormal in hypergammaglobulinaemia. Similar findings were observed in patients with multiple myeloma. Nonspecific binding of IgG to red cells was related to the level of monoclonal protein in the patient’s serum. Usually, in patients with hypergammaglobulinaemia in whom the DAT is positive, attempts to demonstrate antibodies in eluates fail (i.e. eluates are nonreactive). ,
- 10.
Cross-reacting antiphospholipid antibodies adsorbing nonspecifically onto red cell membrane and binding to phospholipid-dependent epitopes. Positive DAT as a result of antiphospholipid antibodies has been documented in patients with primary antiphospholipid syndrome and antiphospholipid syndrome with systemic lupus erythematosus. It has also been described in healthy blood donors.
- 11.
Incidental findings of positive DAT with no clear correlation between DAT and anaemia. A positive DAT is a common finding in patients with sickle cell disease because of abnormal amounts of IgG coating red cells. There was no correlation between the amount of IgG on the patient’s red cells and the severity of anaemia. There was an association demonstrated between an elevated blood urea nitrogen and a positive DAT. Elevated blood urea may alter the red cell membrane and enhance nonspecific IgG adsorption.
- 12.
Sensitization in vitro if a sample other than EDTA is used. If, for instance, clotted or defibrinated normal blood is allowed to stand in a refrigerator at 4 °C or even at room temperature, and the antiglobulin test is subsequently carried out, the reaction may be positive because of the adsorption of incomplete cold antibodies and complement from normal sera. Samples of blood taken into EDTA or ACD and subsequently chilled do not give this type of false-positive result because the anticoagulant inhibits the complement reaction.
- 13.
False-positive agglutination may occur with a silica gel derived from glass. Also, albeit rarely, the DAT has been positive with the blood of apparently perfectly healthy individuals (e.g. blood donors). Such occurrences have not been satisfactorily explained (see below).
Positive direct antiglobulin tests in normal subjects
The occurrence of a clearly positive DAT in an apparently healthy subject is a rare but well-known phenomenon. Worlledge reported a prevalence in blood donors of approximately 1 in 9000. In a later report, Gorst et al . estimated that the prevalence was approximately 1 in 14 000, with an increasing likelihood of a positive test with increasing age. Their report and subsequent reports , suggest that the finding of a positive DAT using an anti- IgG serum in an apparently healthy person is usually of little clinical significance and that, although overt AIHA may subsequently develop, this is infrequent. In some such individuals the DAT eventually becomes negative.
Positive direct antiglobulin tests in hospital patients
In contrast to the rarity of positive DATs in healthy people, positive tests are much more frequent in hospital patients. Worlledge reported that the red cells of 40 out of 489 blood samples (8.9%) submitted for routine tests were agglutinated by anti-C′ sera. Only one sample was agglutinated by an anti-IgG serum and this had been obtained from a patient being treated with α-methyldopa. Freedman reported a similar incidence: 7.8% positive tests with anti-C′ sera. Lau et al . used anti-IgG sera only. The tests were seldom positive (0.9% positive out of 4664 tests). The probable explanation for the relatively high incidence of positive tests with anti-C′ sera is that the reaction is between anti-C′ antibodies and immune complexes adsorbed to the red cells.
False-negative antiglobulin test results
There are several causes of false-negative test results:
- 1.
Failure to wash the red cells properly: the antisera may then be neutralised by immunoglobulins or complement in the surrounding serum or plasma (see p. 454)
- 2.
Excessive agitation at the reading stage: this may break up agglutinates, leading to a false-negative result
- 3.
The use of impotent antisera so that weakly sensitised cells are not detected
- 4.
The use of antisera lacking an antibody corresponding to the subclass of immunoglobulin responsible for the red cell sensitisation
- 5.
The presence of an antibody that is readily dissociable and is eluted in the washing process.
These phenomena are largely negated by the use of column agglutination technology.
Direct antiglobulin test-negative autoimmune haemolytic anaemia
Most hospital blood banks use polyspecific ‘broad- spectrum’ AHG reagents for screening for diagnosis of AIHA. These reagents contain antibody to human IgG and the C3d component of human complement and have little activity against IgA and IgM proteins. The prevalence of IgA-only warm AIHA has been reported as 0.2% to 2.7% and the diagnosis may be missed if such polyspecific AHG is used for the DAT screen. In approximately 2–6% of patients who present with the clinical and haematological features of AIHA, the DAT is negative on repeated testing. , ,
Low-affinity IgG autoantibodies dissociate from the red cells during the washing phase if a tube technique is used, resulting in a negative DAT. Alternatively, there may be few IgG molecules coating the red cells and this number may fall below the threshold of detection, which is 300 to 4000 molecules per red blood cell if a tube technique is used. In such cases, a positive DAT may be demonstrated by a more sensitive technique, such as a column agglutination method, an enzyme-linked immunoabsorbant assay or flow cytometry.
If polyspecific AHG is used and the DAT remains negative with clinical evidence of haemolysis, a more sensitive technique should be used for further investigation.
The DiaMed DAT gel card, which contains a set of monospecific AHG reagents (i.e. anti-IgG, -IgA, -IgM, -C3c, -C3d and an inert control) can be used ( www.diamed.com ). Because there is no washing phase, this permits the detection of low-affinity IgG, IgA and IgM antibodies. A gel card can also pick up the rare IgA-only AIHA. In warm-type AIHA the DAT may be positive with anti-IgG or anti-IgG plus anti-C3d. In cold-type AIHA the DAT may be positive with anti-IgM or anti-IgM plus anti-C3d and in mixed-type AIHA the DAT may be positive with anti-IgG, anti-IgM and anti-C3d.
Manual direct polybrene test
The following method is modified from that of Lalezari and Jiang. Polybrene ( www.sigmaaldrich.com) is a polyvalent cationic molecule, hexadimethrine bromide, which can overcome the electrostatic repulsive forces between adjacent red cells, bringing the cells closer together. When low levels of IgG are present on the red cell surface, antibody linkage of adjacent red cells is enhanced. The Polybrene is then neutralised using a negatively charged molecule such as trisodium citrate. Sensitised red cells remain agglutinated after neutralization of the Polybrene. Unsensitised red cells will disaggregate after neutralisation.
Reagents
- •
Polybrene stock. 10% Polybrene in 9 g/l NaCl, pH 6.9 (saline).
- •
Working Polybrene solution. Dilute the stock Polybrene solution 1 in 250 in saline.
- •
Resuspending solution. 60 ml of 0.2 mol/l trisodium citrate added to 40 ml of 50 g/l dextrose.
- •
Washing solution. 50 ml of 0.2 mol/l trisodium citrate in 950 ml of saline.
- •
Low-ionic medium. 50 g/l dextrose containing 2 g/l disodium EDTA. Adjust the pH of half the batch to 6.4. Store the remainder at the original pH (approx. 4.9); use this to repeat tests that are negative using a low-ionic medium at pH 6.4.
Method.
Ensure that all reagents are at room temperature.
Positive control.
Dilute an IgG anti-D in normal group AB serum. Find a dilution that gives a positive result with papainised cells but is negative by the IAT on standard testing with group O, D-positive red cells (a dilution of 1 in 10 000 is often suitable).
Negative control.
Normal group AB serum that fails to agglutinate papainised group O, D-positive red cells.
- 1.
Wash the cells four times in saline and make 3–5% suspensions of test and normal group O RhD red cells in saline.
- 2.
Set up three 75 × 10 mm tubes as shown in Table 13-5 . Leave at room temperature for 1 min.
Table 13-5
Setting up a direct manual Polybrene test
Test
Positive Control
Negative Control
AB serum (drops)
2
0
2
Dilute anti-D in AB serum (drops)
0
2
0
3–5% test cells (drops)
1
0
0
3–5% normal O RhD cells (drops)
0
1
1
Low ionic-strength medium
0.6 ml
0.6 ml
0.6 ml
- 3.
Add 1 drop of working Polybrene solution to each tube and mix gently. Leave for 15 s at room temperature.
- 4.
Centrifuge for 10 s at 1000 g. Decant, taking care to remove all the supernatant.
- 5.
Leave for 3–5 min at room temperature before adding 2 drops of resuspending solution and mixing gently. Within 10 s aggregates will dissociate, leaving true agglutination in the positive tubes.
- 6.
Read macroscopically after 10–60 s. Check all negative results microscopically and compare with the negative control.
- 7.
Repeat negative tests using low-ionic medium at the lower pH (about 4.9).
If the direct Polybrene test is negative, a supplementary antiglobulin test may be performed by washing the cells twice in the washing solution and testing with an anti-IgG antiglobulin reagent.
Determination of the blood group of a patient with autoimmune haemolytic anaemia
ABO grouping
No difficulty should be encountered in ABO grouping patients with warm-type AIHA using monoclonal reagents, but the presence of cold agglutinins may cause difficulties. The cells should in all cases be washed in warm (37 °C) saline. They should then be groupable without any problem; the reactions must, however, be controlled with normal AB serum. Reverse grouping should be performed strictly at 37 °C. Warm the known A 1 , B and O cells to 37 °C before adding them to the patient’s serum at 37 °C. Read the results macroscopically.
RhD grouping
When the DAT is positive, monoclonal anti-D reagents should be used; if cold agglutinins are present, perform the test at 37 °C. Appropriate controls should be included (see p. 475).
Demonstration of free antibodies in serum
The sera of patients suffering from AIHA often contain free autoantibodies. However, free autoantibody is also found in the absence of haemolysis. As a result of improved reagent sensitivity, any clinically significant IgG complement- binding antibodies will be detected by current antibody screening methods.
Identification by adsorption techniques of coexisting alloantibodies in the presence of warm autoantibodies
Adsorption techniques for the detection of alloantibodies present in the sera or eluates of patients with suspected or proved AIHA can be helpful in the following situations:
- 1.
In screening for coexisting alloantibodies in patients with AIHA who have been pregnant or previously transfused and are found to have a panreactive antibody in their serum
- 2.
In differentiating between autoantibodies and alloantibodies in the eluate of recently transfused patients with AIHA
- 3.
In investigating haemolytic transfusion reactions owing to red cell alloantibodies in patients with AIHA.
In some cases of AIHA, an underlying alloantibody may be detected by titrating the patient’s serum and eluate against a panel of phenotyped reagent red cells. However, a high-titre autoantibody may mask the alloantibody; hence the need for adsorption techniques, especially in the situations outlined earlier.
Use of ZZAP reagent in autoadsorption techniques
‘ZZAP’ reagent is a mixture of dithiothreitol and papain. It dissociates an autoantibody already coating the patient’s red cells and enzyme treats the cells, thus increasing the amount of autoantibody that can subsequently be adsorbed onto the patient’s cells in vitro.
Reagents
- •
Dithiothreitol (DTT). 0.2 mol/l.
- •
Papain . 1%.
- •
Phosphate-buffered saline (PBS). pH 6.8–7.2.
Prepare a suitable volume of ZZAP by making up the reagents in the following ratio: 0.2 mol/l DTT 5 volumes; and 1% papain 1 volume.
Check the pH and adjust to pH 6.0–6.5 using one drop at a time of 0.2 mol/l HCl or 0.2 mol/l NaOH.
Method
- 1.
Add 2 volumes of ZZAP to 1 volume of packed red cells that have been washed four times. Incubate at 37 °C for 30 min, mixing occasionally.
- 2.
After incubation, wash the cells four times in saline, packing hard after the last wash.
- 3.
Divide the cells into two equal volumes. To one volume, add an equal volume of the serum to be adsorbed. Incubate at 37 °C for 1 h.
- 4.
Centrifuge at 1000 g . Remove the serum and add to the remaining volume of cells.
- 5.
Repeat the adsorption procedure.
- 6.
Remove the adsorbed serum and store at − 20 °C or below for alloantibody screening or cross-matching, which may be performed by standard techniques.
Notes.
The autoadsorption techniques should only be used in the following circumstances:
- 1.
When the patient has not had a transfusion in the previous 3 months because the presence of transfused red cells may allow the adsorption of alloantibody as well as autoantibody
- 2.
When at least 2 to 3 ml of packed red cells are available from the patient
- 3.
When the autoantibodies present react well with enzyme-treated red cells. If they do not, heat elution should be substituted for ZZAP treatment. Heat elution may be performed by shaking the washed cells for 5 min in a 56 °C water bath and then washing the cells.
Alloadsorption using papainised R 1 R 1 , R 2 R 2 and rr cells
The method of alloadsorption using papainised R 1 R 1 , R 2 R 2 and rr cells may be used when autoadsorption is not appropriate, for instance, when the patient has had a transfusion in the previous 3 months or when less than 2–3 ml of the patient’s red cells are available.
- 1.
Select three group O antibody screening cells, which individually lack some of the blood-group antigens that commonly stimulate the production of clinically significant antibodies (e.g. c, e, C, E, K, Fy a , Fy b , Jk a , Jk b , S, s) ( Table 13-6 ).
Table 13-6
Testing an alloaDsorbed serum against a phenotyped panel of red cells
No.
Red Cell Phenotypes
Results of IAT
Rh
M
N
S
s
P 1
Lu a
Le a
Le b
K
Kp a
Fy a
Fy b
Jk a
Jk b
Serum A
Serum B
Serum C
1.
R 1 R 1
+
+
+
+
+
−
−
−
+
−
+
+
+
+
1 +
1 +
–
2.
R 1 R 1
+
−
−
+
−
+
−
+
−
−
+
+
+
+
1 +
3 +
–
3.
R 2 R 2
+
+
+
+
+
+
+
−
−
−
−
+
−
+
1 +
–
3 +
4.
R 1 R 2
+
+
+
−
+
−
−
+
−
−
−
+
+
−
1 +
4 +
1 +
5.
r′r
+
−
+
+
+
−
−
+
−
−
+
+
−
+
−
–
–
6.
r″r
+
+
+
−
+
−
−
+
−
−
+
−
+
+
2 +
2 +
2 +
7.
rr
+
+
−
+
+
−
−
−
+
−
+
+
+
−
2 +
2 +
–
8.
rr
+
−
+
+
+
−
+
−
−
−
+
−
+
−
1 +
2 +
(+)
9.
rr
−
+
−
+
+
−
+
−
−
+
+
+
+
+
2 +
2 +
–
10.
R 1 R 2
−
+
+
+
−
−
−
+
+
−
−
+
+
−
1 +
3 +
2 + 
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree