DIAGNOSIS
Part of “CHAPTER 17 – HYPOPITUITARISM“
GENERAL PRINCIPLES
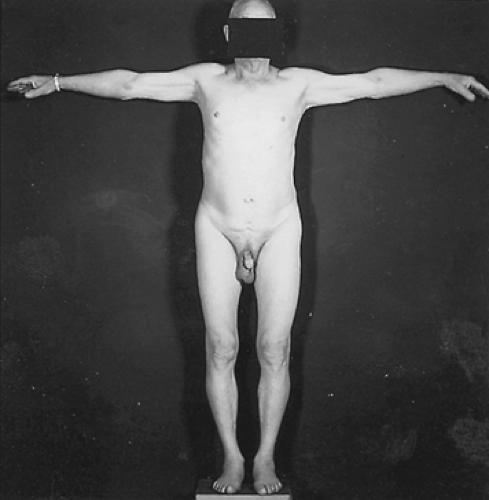
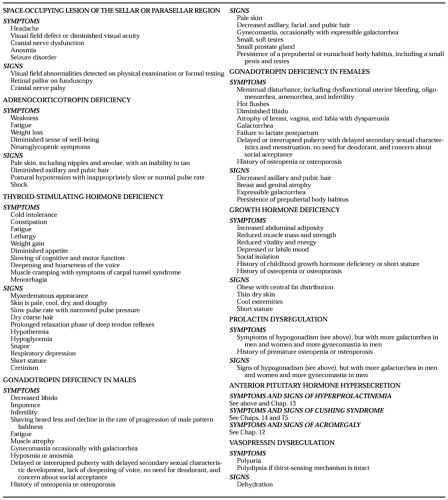
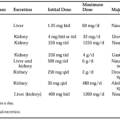
The history and physical examination (Fig. 17-1; see Table 17-1 and Table 17-2) will usually help in the selection of subsequent laboratory studies. Some hormonal deficiencies or even a mass lesion may be inapparent from the history and physical examination alone and can be detected only by an appropriate laboratory and radiologic survey. The laboratory evaluation for
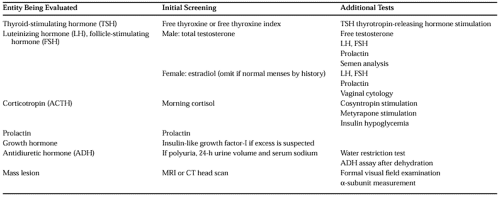
hypopituitarism can be divided into initial screening tests and supplemental tests that should be considered if the initial results are abnormal (Table 17-3).
hypopituitarism can be divided into initial screening tests and supplemental tests that should be considered if the initial results are abnormal (Table 17-3).
The most effective initial approach to detecting adrenal or gonadal hypofunction is to assay the target gland hormones, even if the underlying defect is thought to be at the pituitary level. The serum concentrations of the target gland hormones are less variable than pituitary hormone levels and are generally more useful for differentiating subnormal from normal target gland function. If any of these target hormone values are diminished, the serum levels of the corresponding pituitary hormones should be measured. Because primary hypothyroidism is commonly seen in clinical practice, and because serum TSH is a very sensitive test used to diagnose primary hypothyroidism, many clinicians are in the habit of measuring TSH to diagnose hypothyroidism. However, if secondary hypothyroidism is suspected, the target gland hormone (free thyroxine [FT4]) should be measured. Evaluation of GH deficiency in adults is typically not undertaken
unless definite pituitary pathology is documented. Serum prolactin is usually measured as part of any evaluation for hypogonadism or hypopituitarism.
unless definite pituitary pathology is documented. Serum prolactin is usually measured as part of any evaluation for hypogonadism or hypopituitarism.
If a target gland hormone is definitely deficient, and the corresponding pituitary hormone concentration is clearly elevated, the diagnosis is primary target-gland failure. If, however, the pituitary hormone value is subnormal, this is consistent with deficiency at the level of the pituitary or hypothalamus. In the presence of frank target gland failure, a normal pituitary hormone concentration in the serum may represent biologically hypoactive hormone.20
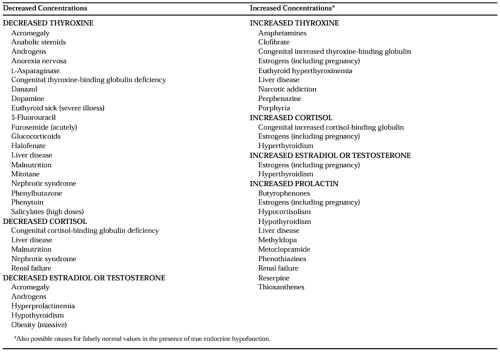
The tests recommended in Table 17-3 usually provide good discrimination between normal and abnormal endocrine states, but false-positive and false-negative results are seen, often in conjunction with certain medications and diseases. Table 17-4 lists the factors
that can lower hormone values and cause false-positive diagnoses, and those that raise the hormone values and could obscure a true-positive result. Four general mechanisms account for most of this interference. First, the target gland hormones of the thyroid, adrenal gland, and gonads circulate partially bound to specific carrier proteins; any medication or disease that changes the hepatic synthesis of a carrier protein also changes the concentration of total hormone, even if the hormonally active free fraction remains constant throughout. Second, hypersecretion or hyposecretion of one pituitary hormone may cause a change in the concentration of another pituitary hormone. The latter abnormality disappears when the former is corrected by appropriate therapy. The suppression of gonadotropins by hyperprolactinemia is one example. Another is the increase of serum TSH concentration that occasionally can be seen in untreated primary or secondary hypoadrenalism.21 Third, diseases that affect urinary excretion (e.g., uremia, nephrotic syndrome) or alter hepatic degradation (e.g., various liver diseases, hypothyroidism)—as well as severe, stressful illness—may alter hormone concentrations. The euthyroid sick syndrome, common in intensive care units or among other similarly stressed patients, mimics the laboratory findings of secondary hypothyroidism.22 Fourth, some medications are a potential source of error. Phenytoin and high doses of salicylates can bind to the hormonal binding sites on thyroxine (T4) binding proteins; this results in a decrease in total T4 concentration, but the FT4 determination remains unaltered. The information summarized in Table 17-4 can alert the physician to most cases of potential misinterpretation. However, if the clinical picture and the test results do not initially seem to agree, the prudent course is to review both carefully before rejecting either.
that can lower hormone values and cause false-positive diagnoses, and those that raise the hormone values and could obscure a true-positive result. Four general mechanisms account for most of this interference. First, the target gland hormones of the thyroid, adrenal gland, and gonads circulate partially bound to specific carrier proteins; any medication or disease that changes the hepatic synthesis of a carrier protein also changes the concentration of total hormone, even if the hormonally active free fraction remains constant throughout. Second, hypersecretion or hyposecretion of one pituitary hormone may cause a change in the concentration of another pituitary hormone. The latter abnormality disappears when the former is corrected by appropriate therapy. The suppression of gonadotropins by hyperprolactinemia is one example. Another is the increase of serum TSH concentration that occasionally can be seen in untreated primary or secondary hypoadrenalism.21 Third, diseases that affect urinary excretion (e.g., uremia, nephrotic syndrome) or alter hepatic degradation (e.g., various liver diseases, hypothyroidism)—as well as severe, stressful illness—may alter hormone concentrations. The euthyroid sick syndrome, common in intensive care units or among other similarly stressed patients, mimics the laboratory findings of secondary hypothyroidism.22 Fourth, some medications are a potential source of error. Phenytoin and high doses of salicylates can bind to the hormonal binding sites on thyroxine (T4) binding proteins; this results in a decrease in total T4 concentration, but the FT4 determination remains unaltered. The information summarized in Table 17-4 can alert the physician to most cases of potential misinterpretation. However, if the clinical picture and the test results do not initially seem to agree, the prudent course is to review both carefully before rejecting either.
All patients with hypopituitarism should have an MRI or CT scan (see Chap. 20). In many cases, an MRI study is preferable, because it provides better anatomic detail, may detect a microadenoma that is not visible on a CT scan, is better able to demonstrate whether a mass lesion is impinging on the chiasm, and can better differentiate an aneurysm from other mass lesions. However, an MRI is more expensive than a CT scan, and in some clinical situations a CT scan is sufficient (e.g., if the only purpose is to rule out a large tumor that would be easily seen with either technique). With current methods, some small pituitary tumors cannot be detected by either imaging method. Absence of a visible mass does not definitively rule out a tumor, and periodic follow-up examinations may be indicated. When MRI or CT is performed, it should be a “dedicated” study with thin sections through the sellar and suprasellar area, performed with and without contrast.1,23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree