TREATMENT FOR PROLACTINOMAS
Part of “CHAPTER 13 – PROLACTIN AND ITS DISORDERS“
Treatment depends on whether the patient has hyperpro-lactinemia due to an underlying cause such as drugs or hypothyroidism, or due to a prolactinoma. If the evaluation suggests the presence of a microprolactinoma, three treatment options are available: medical therapy with a dopamine agonist, careful follow-up without treatment, and, rarely, surgery. All patients with macroadenomas should be treated.
MEDICAL THERAPY
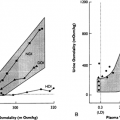
Almost all patients with hyperprolactinemia due to pituitary disease can be effectively treated medically with the dopamine agonist bromocriptine (see Chap. 21). Bromocriptine lowers serum prolactin in patients with pituitary tumors and all other causes of hyperprolactinemia. A review of early studies of bromocriptine therapy for more than 400 hyperprolactinemic patients showed that normoprolactinemia or return of ovulatory menses occurred in 80% to 90% of patients.45 Bromocriptine effectively decreases prolactin levels, normalizes reproductive function, and reverses galactorrhea. In this series, return of menstrual function was accompanied in some patients by prolactin levels that were significantly reduced but not normal. This suggests that the reduction of prolactin levels in some patients to slightly elevated levels may be sufficient for return of gonadal function. Bromocriptine is also useful in treating galactorrhea in patients with normoprolactinemic galactorrhea.
The onset of the effects of bromocriptine is rapid, usually occurring within 1 to 2 hours. The greatest decrease in prolactin levels occurs at the initiation of therapy; however, normalization may take weeks. The biologic half-life of bromocriptine is similar to its plasma half-life. Discontinuation of the drug is typically followed by a return of prolactin to elevated values. Bromocriptine decreases prolactin production and secretion, with a resultant reduction in lactotrope size and a subsequent decrease in tumor size.46
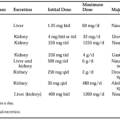
Therapy should be initiated slowly because side effects, including nausea, headache, dizziness, nasal congestion, and constipation, may occur. Gastrointestinal side effects may be minimized by starting with a very low dose (e.g., 1.25 mg, or one-half tablet) taken at night with a snack, and increasing the dose by 1.25 mg over 4- to 5-day intervals, as tolerated. This progression is continued until a dosage that normalizes prolac-tin levels is reached. The rate of dosage escalation is dictated by the clinical situation, such as the presence of mass effects. Side effects can usually be improved by continuing the medication at the same dosage or by temporarily reducing the dosage. If
patients stop taking the medication for a few days, therapy should be reinstituted at a lower dosage, because side effects may return. Rarely, long-term therapy may result in side effects, including painless cold-induced digital vasospasm, alcohol intolerance, dyskinesia, and psychiatric reactions, including fatigue, depression, and anxiety.
patients stop taking the medication for a few days, therapy should be reinstituted at a lower dosage, because side effects may return. Rarely, long-term therapy may result in side effects, including painless cold-induced digital vasospasm, alcohol intolerance, dyskinesia, and psychiatric reactions, including fatigue, depression, and anxiety.
To reduce the gastrointestinal side effects, bromocriptine has been administered intravaginally. Reductions in prolactin similar to that attained by oral bromocriptine have been achieved with the intravaginal route.47 Gastrointestinal side effects are less common, and therapy may be more effective with vaginally administered bromocriptine.48
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree