B-CELL DISEASES
Chronic lymphocytic leukaemia
Chronic lymphocytic leukaemia (CLL) is the most common of the chronic lymphoid leukaemias and has a peak incidence between 60 and 80 years of age. The aetiology is unknown but there are geographical variations in incidence. It is the most common of the leukaemias in the Western world but rare in the Far East. In contrast to other forms of leukaemia there is no higher incidence after previous chemotherapy or radiotherapy. There is a sevenfold increased risk of CLL in the close relatives of patients which indicates a genetic predisposition.
The tumour cell appears to be a relatively mature B cell with weak surface expression of immunoglobulin (IgM or IgD). The cells accumulate in the blood, bone marrow, liver, spleen and lymph nodes as a result of increased production and prolonged lifespan with impaired apoptosis. Small lymphocytic lymphoma (SLL) (see Chapter 20) is the tissue equivalent of CLL. The lymphoma cells have the same immunophenotype and cytogenetics but in SLL there is solid tissue disease and fewer than 5 × 109/L circulating monoclonal B cells.
Monoclonal B-cell lymphocytosis Clonal B cells with the same phenotype as CLL are found at low levels in the blood of many older patients. Indeed, this monoclonal B-cell lymphocytosis (MBL) has been demonstrated in 3% of patients over the age of 50 years and it is believed that all cases of clinical CLL progress from this state. Similar genetic changes to these found in CLL may be present. If CLL is to be diagnosed there must be a monoclonal B-cell count of >5 × 109/L or tissue involvement outside the bone marrow.
Clinical features
1 The disease occurs in older subjects with only 15% of cases before 50 years of age. The male: female ratio is 2: 1.
2 Most cases are diagnosed when a routine blood test is performed. With increasing routine medical check-ups, this proportion is rising to > 80%.
3 Symmetrical enlargement of cervical, axillary or inguinal lymph nodes is the most frequent clinical sign (Fig. 18.1). The nodes are usually discrete and non-tender. Tonsillar enlargement may be a feature.
4 Features of anaemia may be present. Patients with thrombocytopenia may show bruising or purpura.
5 Splenomegaly and, less commonly, hepatomegaly are common in later stages.
6 Immunosuppression may be a significant problem resulting from hypogammaglobulinaemia and cellular immune dysfunction. Early in the disease course bacterial infections predominate but with advanced disease viral and fungal infections such as herpes zoster are also seen (Fig. 18.2).
Figure 18.1 Chronic lymphocytic leukaemia: bilateral cervical lymphadenopathy in a 67-year-old woman. Haemoglobin 12.5g/dL; white blood count 150 × 109/L (lymphocytes 146 × 109/L); platelets 120 × 109/L.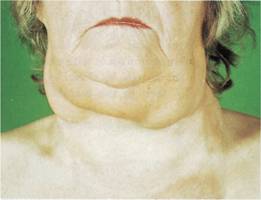
Figure 18.2 Chronic lymphocytic leukaemia: herpes zoster infection in a 68-year-old female.
Laboratory findings
1 Lymphocytosis. The absolute clonal B cell lymphocyte count is >5 × 109/L and may be up to 300 × 109/L or more. Between 70 and 99% of white cells in the blood film appear as small lymphocytes. Smudge or smear cells are also present (Fig. 18.3).
2 Immunophenotyping of the lymphocytes shows them to be B cells (surface CD19+), weakly expressing surface immunoglobulin (IgM or IgD). This is shown to be monoclonal because of expression of only one form of light chain (κ or λ; Table 18.2). Characteristically, the cells are also surface CD5+ and CD23+ but are CD79b− and FMC7− (Fig. 18.4).
3 Normochromic normocytic anaemia is present in later stages as a result of marrow infiltration or hypersplenism. Autoimmune haemolysis may also occur (see below). Thrombocytopenia occurs in many patients.
4 Bone marrow aspiration shows lymphocytic replacement of normal marrow elements. Lymphocytes comprise 25–95% of all the cells. Trephine biopsy reveals nodular, diffuse or interstitial involvement by lymphocytes (Fig. 18.5).
5 Reduced concentrations of serum immunoglobulins are found and this becomes more marked with advanced disease. Rarely, a paraprotein is present.
6 Autoimmunity directed against cells of the haemopoietic system is common. Autoimmune haemolytic anaemia is most frequent but immune thrombocytopenia (see p. 334), neutropenia and red cell aplasia are also seen.
Figure 18.3 Chronic lymphocytic leukaemia: peripheral blood film showing lymphocytes with thin rims of cytoplasm, coarse condensed nuclear chromatin and rare nucleoli. Typical smudge cells are present.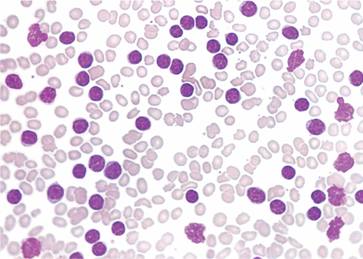
Table 18.2 Immunophenotype of the chronic B-cell leukaemias/lymphomas (all cases CD 19 +).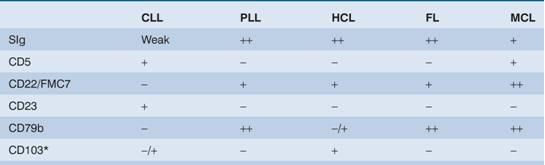
CLL, chronic lymphocytic leukaemia; FL, follicular lymphoma; HCL, hairy cell leukaemia; MCL, mantle cell lymphoma; PLL, prolymphocytic leukaemia.
* CD103 is positive only in HCL.
Figure 18.4 Immunophenotypic analysis of chronic lymphocytic leukaemia by flow cytometric cell (FACS) analysis. In this case, the cells are CD5+, CD19+, CD20+, CD23+, CD79b+, lambda light chain+.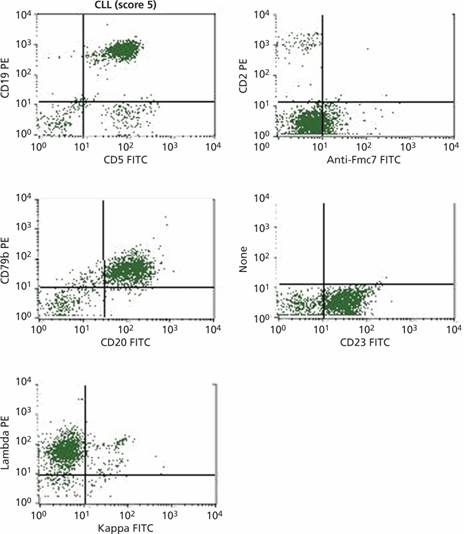
Figure 18.5 Chronic lymphocytic leukaemia: trephine biopsies showing: (a) a marked diffuse increase in marrow lymphocytes (closely packed cells with small dense nuclei); (b) a nodular pattern of lymphocyte accumulation (in a different patient); and (c) interstitial infiltration.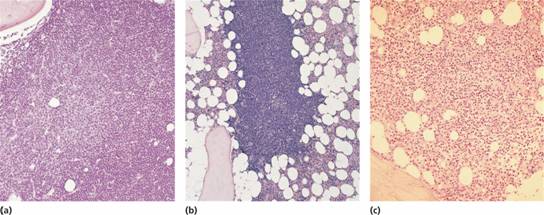
Prognostic markers
Cytogenetics
The most common chromosome abnormalities are deletion of 13q14, trisomy 12, deletions at 11q23 (affecting the ATM gene), structural abnormalities of 17p involving the p53 gene and 6q21 deletion. These abnormalities carry prognostic significance (Table 18.3). The 13q14 deletion leads to loss of microRNAs which normally control expression of proteins that regulate B-cell survival (see p. 160).
Table 18.3 Prognostic factors in chronic lymphocytic leukaemia.
| Good | Bad | |
| Stage | Binet A (Rai 0–I) | Binet B, C (Rai II–IV) |
| Sex | Female | Male |
| Lymphocyte doubling time | Slow | Rapid |



