Abnormal bleeding
This may result from:
1 Vascular disorders
2 Thrombocytopenia
3 Defective platelet function or
4 Defective coagulation.
The pattern of bleeding is relatively predictable depending on the aetiology. Vascular and platelet disorders tend to be associated with bleeding from mucous membranes and into the skin whereas in coagulation disorders the bleeding is often into joints or soft tissue (Table 25.1).
Table 25.1Clinical differences between diseases of platelets/vessel wall or of coagulation factors.
| Platelets/vessel wall diseases | Coagulation diseases | |
| Mucosal bleeding | Common | Rare |
| Petechiae | Common | Rare |
| Deep haematomas | Rare | Characteristic |
| Bleeding from skin cuts | Persistent | Minimal |
| Sex of patient | Equal | >80% male |
The first three categories are discussed in this chapter and the disorders of blood coagulation follow in Chapter 26.
The vascular disorders are a heterogeneous group of conditions characterized by easy bruising and spontaneous bleeding from the small vessels. The underlying abnormality is either in the vessels themselves or in the perivascular connective tissues. Most cases of bleeding caused by vascular defects alone are not severe. Frequently, the bleeding is mainly in the skin causing petechiae, ecchymoses or both (Fig. 25.1). In some disorders there is also bleeding from mucous membranes. In these conditions the standard screening tests are normal. The bleeding time is usually normal and the other tests of haemostasis are also normal. Vascular defects may be inherited or acquired.
Figure 25.1 (a) Hereditary haemorrhagic telangiectasia: the characteristic small vascular lesions are obvious on the lips and tongue. (b) Senile purpura. (c) Characteristic perifollicular petechiae in vitamin C deficiency (scurvy).
Inherited vascular disorders
Hereditary haemorrhagic telangiectasia
This uncommon disease is transmitted as an autosomal dominant trait. Various genetic defects underlie the disease, e.g. of the endothelial protein, endoglin. There are dilated microvascular swellings which appear during childhood and become more numerous in adult life. These telangiectasia develop in the skin, mucous membranes (Fig. 25.1a) and internal organs. Pulmonary, hepatic, splenic and cerebral arteriovenous shunts are seen in a minority of cases. Recurrent epistaxes are frequent and recurrent gastrointestinal tract haemorrhage may cause chronic iron deficiency anaemia. Treatment is with embolization, laser treatment, oestrogens, tranexamic acid and iron supplementation.
Connective tissue disorders
In the Ehlers–Danlos syndromes there are hereditary collagen abnormalities with purpura resulting from defective platelet aggregation, hyperextensibility of joints and hyperelastic friable skin. Pseudoxanthoma elasticum is associated with arterial haemorrhage and thrombosis. Patients may present with superficial bruising and purpura following minor trauma or after the application of a tourniquet. Bleeding and poor wound healing after surgery may be a problem.
Giant cavernous haemangioma
These congenital malformations occasionally cause chronic activation of coagulation leading to laboratory features of disseminated intravascular coagulation (DIC) and in some cases thrombocytopenia.
Acquired vascular defects
1 Simple easy bruising is a common benign disorder which occurs in otherwise healthy women, especially those of child-bearing age.
2 Senile purpura caused by atrophy of the supporting tissues of cutaneous blood vessels is seen mainly on dorsal aspects of the forearms and hands (Fig. 25.1b).
3 Purpura associated with infections, mainly of bacterial, viral or rickettsial origins may cause purpura from vascular damage by the organism with DIC or as a result of immune complex formation (e.g. measles, dengue fever or meningococcal septicaemia).
4 The Henoch–Schönlein syndrome is usually seen in children and often follows an acute upper respiratory tract infection. It is an immunoglobulin A (IgA)-mediated vasculitis. The characteristic purpuric rash accompanied by localized oedema and itching is usually most prominent on the buttocks and extensor surfaces of the lower legs and elbows (Fig. 25.2). Painful joint swelling, haematuria and abdominal pain may also occur. It is usually a self-limiting condition but occasional patients develop renal failure.
5 Scurvy. In vitamin C deficiency, defective collagen may cause perifollicular petechiae, bruising and mucosal haemorrhage (Fig. 25.1c).
6 Steroid purpura. The purpura, which is associated with long-term steroid therapy or Cushing’s syndrome, is caused by defective vascular supportive tissue.
Figure 25.2Henoch–Schönlein purpura: (a) unusually severe purpura on legs with bullous formation in a 6-year-old child; and (b) early urticarial lesions.
Tranexamic acid and aminocaproic acid are useful antifibrinolytic drugs that may reduce bleeding resulting from vascular disorders or thrombocytopenia but are relatively contraindicated in the presence of haematuria because they might lead to clots obstructing the renal tract.
Abnormal bleeding associated with thrombocytopenia or abnormal platelet function is characterized by spontaneous skin purpura (Fig. 25.3) and mucosal haemorrhage and prolonged bleeding after trauma (Table 25.1). The main causes of thrombocytopenia are listed in Tables 25.2 and 25.3.
Figure 25.3 (a) Typical purpura; and (b) massive subcutaneous haemorrhage in a patient with drug-induced thrombocytopenia.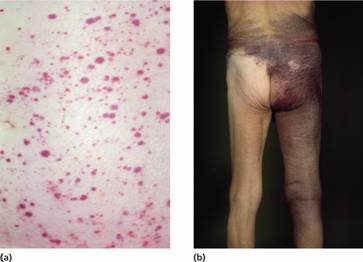
Table 25.2Causes of thrombocytopenia.
| Failure of platelet production |
| Selective megakaryocyte depression rare congenital defects (see text) drugs, chemicals, viral infections |
| Part of general bone marrow failure |
| cytotoxic drugs |
| radiotherapy |
| aplastic anaemia |
| leukaemia |
| myelodysplastic syndromes |
| myelofibrosis |
| marrow infiltration (e.g. carcinoma, lymphoma, Gaucher’s disease) |
| multiple myeloma |
| megaloblastic anaemia |
| HIV infection |
| Increased consumption of platelets |
| Immune |
| autoimmune |
| idiopathic |
| associated with systemic lupus erythematosus, chronic lymphocytic leukaemia or lymphoma; |
| infections: Helicobacter pylori, HIV, other viruses, malaria |
| drug-induced, e.g. heparin |
| post-transfusional purpura |
| Feto–maternal alloimmune thrombocytopenia |
| Disseminated intravascular coagulation |
| Thrombotic thrombocytopenic purpura |
| Abnormal distribution of platelets |
| Splenomegaly (e.g. liver disease) |
| Dilutional loss |
| Massive transfusion of stored blood to bleeding patients |
HIV, human immunodeficiency virus.
Table 25.3Thrombocytopenia as a result of drugs or toxins.
| Bone marrow suppression |
| Predictable (dose–related) |
| ionizing radiation, cytotoxic drugs, ethanol |
| Occasional |
| chloramphenicol, co-trimoxazole, idoxuridine, penicillamine, organic arsenicals, benzene, etc. |
| Immune mechanisms (proven or probable) |
| Analgesics, anti-inflammatory drugs gold salts |
| Antimicrobials |
| penicillins, rifamycin, sulphonamides, trimethoprim, para-aminosalicylate |
| Sedatives, anticonvulsants |
| diazepam, sodium valproate, carbamazepine |
| Diuretics |
| acetazolamide, chlorathiazides, frusemide |
| Antidiabetics |
| chlorpropamide, tolbutamide |
| Others |
| digitoxin, heparin, methyldopa, oxyprenolol, quinine, quinidine |
Failure of platelet production
This is the most common cause of thrombocytopenia and is usually part of a generalized bone marrow failure (Table 25.2). Selective megakaryocyte depression may result from drug toxicity or viral infection. Rarely, it is congenital as a result of mutation of the c-MPL thrombopoietin receptor, in association with absent radii, or in May–Hegglin anomaly with large inclusions in granulocytes, or in Wiskott–Aldrich syndrome (WAS) with eczema and immune deficiency. WAS is caused by mutation of the WASP gene, the protein being a regulator of signalling in haemopoietic cells. Diagnosis of these causes of thrombocytopenia is made from the clinical history, peripheral blood count, the blood film and bone marrow examination.
Increased destruction of platelets
Autoimmune (idiopathic) thrombocytopenic purpura
Autoimmune (idiopathic) thrombocytopenic purpura (ITP) may be divided into chronic and acute forms.
Chronic idiopathic thrombocytopenic purpura
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


