63.1
Insufficiency fracture
The world population is aging with its many manifestations, not least in the sale of diapers. Recently in Japan, for the very first time ever, the sale of adult diapers outdid that of baby diapers ! As the average age of the population rises, the prevalence of osteoporosis, which affects at least one in four women and one in eight men aged more than 65 years, will increase. Osteoporosis per se is a clinically innocuous disease with no direct clinical symptoms. It is the occurrence of osteoporotic fracture that makes osteoporosis a serious medical condition. All the preventative measures, investigations, and treatment of osteoporosis have but one goal and that is to prevent osteoporotic fracture.
Osteoporotic fractures occur preferentially in the vertebral bodies, the proximal femur, and the distal radius, but minimal trauma fractures of all bones (with the exception of fingers, toes, face, and skull) are likely osteoporotic, especially in association with low bone mass or osteoporosis by bone mineral density (BMD). Fractures of these bones are uncommon before 60 years of age but are increasingly prevalent thereafter. These particular bone areas, especially the vertebral body and distal radius, are susceptible to osteoporosis as they tend to depend more on trabecular rather than cortical bone for their strength. Although osteoporosis leads to loss of both cortical as well as trabecular bone strength, trabecular bone is preferentially affected early, especially in younger women at the time of menopause. Vertebral body fracture is the most common and usually the first osteoporotic fracture to occur .
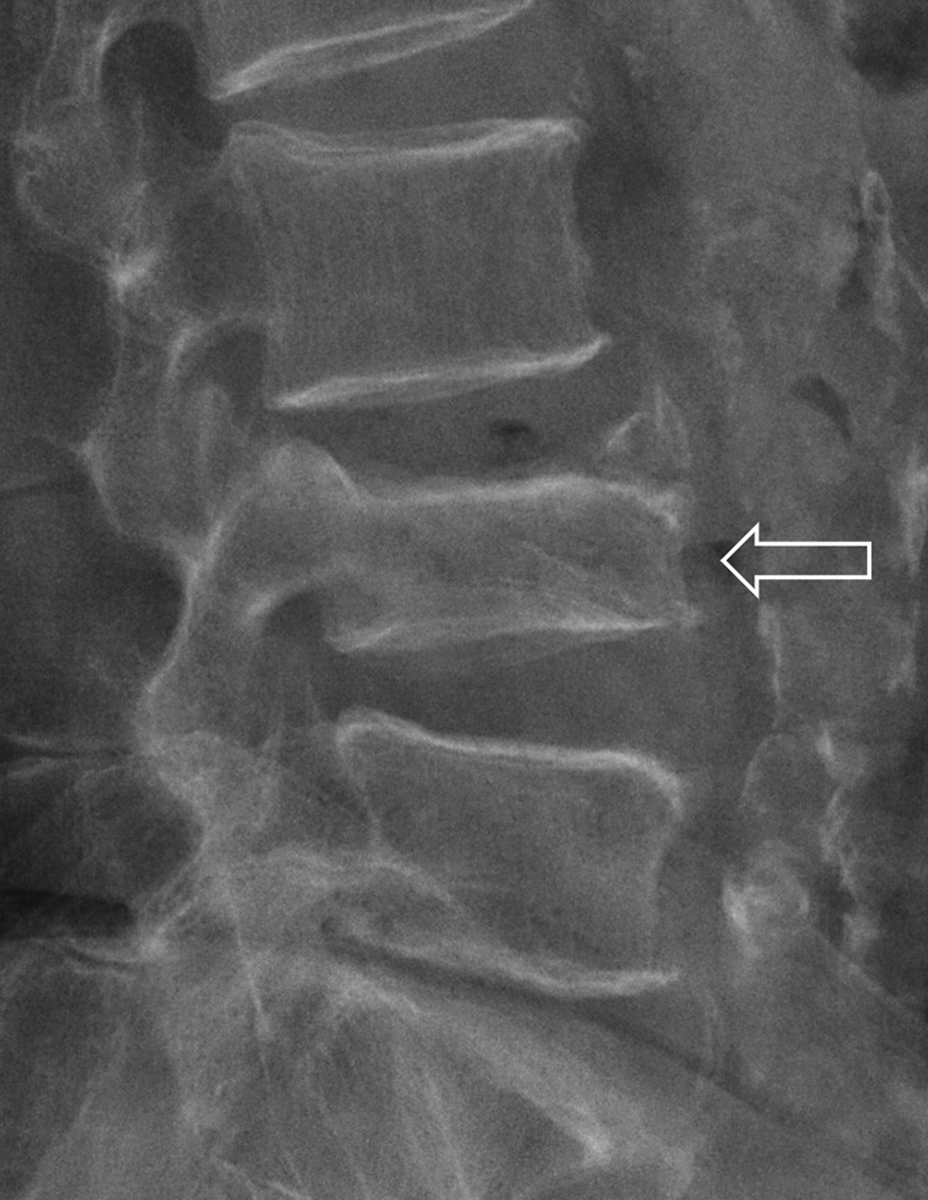
Osteoporotic vertebral fracture is classified as an insufficiency fracture. There are four types of adult bone fracture: (1) traumatic fracture , when the trauma force exceeds the strength of the bone; (2) pathological fracture , when a focal bone lesion, typically a tumor, but occasionally infection, focally weakens bone causing it to fracture with relatively minor or no trauma; (3) stress (or fatigue) fracture , seen mainly in high-performance athletes, when normal quality bone fractures incrementally as a result of repeated excessive physical stress; and (4) insufficiency fracture , when diffusely weakened bone fractures with relatively mild or no trauma ( Fig. 63.1 ). Insufficiency fracture is also called a fragility fracture. By far, the most common cause of insufficiency fracture is osteoporosis. Less common causes include osteogenesis imperfecta, radiation osteonecrosis, renal osteodystrophy, and osteomalacia . When necessary, a clinical history can usually isolate these less common nonosteoporotic causes of insufficiency fracture. Atypical subtrochanteric femoral fracture is another type of insufficiency fracture, which usually is due to adynamic bone disease, but specific pathophysiology of these fractures remains elusive at the current time .

An insufficiency fracture, therefore, is a fracture that occurs with relatively mild or no trauma. The working definition of “relatively mild trauma” is a fall from a standing height or less . A fall from a standing height or less would not be expected to result in fracture of a normal vertebral body, proximal femur, or distal radius. If a bone fracture occurs following a regular fall from a standing height or less, the affected bone is weak, and osteoporosis is the most likely cause. Therefore an insufficiency fracture usually provides clear unambiguous evidence of osteoporosis.
63.1.1
Why it is important to diagnose osteoporotic vertebral fracture?
Diagnosing an osteoporotic vertebral fracture is important for three main reasons. First, it provides a source for the patient’s symptoms. Second, it provides a marker of reduced bone strength, and third, it helps predict future osteoporotic fracture and is required to evaluate comprehensively a patient’s future fracture risk.
63.1.1.1
Patient’s symptoms
As back pain is so common in elderly patients, most insufficiency fractures of the vertebral body go unrecognized clinically as symptoms are attributed to degenerative spinal disease. This is especially so since osteoporotic vertebral fractures typically occur during normal day-to-day activities such as bending, walking, or lifting relatively light objects. Three-quarters of patients with osteoporotic vertebral fracture do not seek medical attention , and even up to two-thirds of these fractures may not result in particularly severe symptoms . Clinical assessment of osteoporotic vertebral fractures is generally poor, and reliance is made on imaging studies for diagnosis.
In addition to pain, osteoporotic vertebral fractures result in immobility, hypostatic chest infection, restrictive lung disease, abdominal protuberance and discomfort, muscle loss, inability to cope with daily activities, and social isolation . Multiple vertebral fractures can result in loss of height, exaggerated thoracic kyphosis, poor self-image, and loss of self-esteem. As well as increased morbidity, increased mortality is also associated with vertebral fracture. For example, subjects with incident fracture have a threefold increased mortality risk over the ensuring 4 years compared to nonfractured counterparts, particularly due to pulmonary disease and cancer .
63.1.1.2
Marker of reduced bone strength
Most patients with an insufficiency fracture, including insufficiency fracture of the vertebral body, will have normal or osteopenic BMD if measured using dual-energy X-ray absorptiometry (DXA) . Even though the prevalence of osteoporosis increases with age in older patients, most patients older than 65 years will still have normal or osteopenic BMD by DXA . DXA examination measures areal bone density. While bone density is a critical aspect of bone strength, other factors such as bone macro- and microarchitecture as well as bone turnover and matrix also contribute to bone strength . Therefore DXA is measuring just one aspect, albeit a very important aspect, of bone strength. As a result, the association between DXA–BMD and fracture risk is not absolute though both prevalent and incident vertebral fracture rates are clearly higher in those with lower BMD.
With increasing age, not only does bone mass tend to decrease but the other components of bone such as the bone architecture, microstructure, collagen composition, bone perfusion, and marrow composition also tend to deteriorate making bone more liable to fracture. Further, estrogen deficiency at menopause is a principal pathophysiologic cause of microarchitectural deterioration of cancellous bone (with trabecular perforation) due to excessive bone resorption . As a result, the bone of an elderly person with normal bone density is not as strong as a young patient with normal bone density .
As bone density decreases irrespective of patient age, fracture risk undoubtedly increases. The fracture risk of patients with osteoporosis on DXA is greater than those with osteopenia (low bone mass) which in turn is greater than those with normal bone density. In other words, patients with normal bone density or osteopenia on DXA still have a risk of fracture, but this risk is not as great as in patients with osteoporosis. Overall, however, since more elderly patients have normal BMD or low bone mass on DXA rather than osteoporosis, most patients with insufficiency fracture tend not to have osteoporosis on DXA.
A comparable analogy is the likelihood of a golfer hitting a hole-in-one. A golfer with a low-handicap is more likely to score a hole-in-one compared to an average or high-handicap golfer. However, because the number of average or high-handicap golfers outnumbers the number of low-handicap golfers, most holes-in-one are scored by average or high-handicap golfers. Similarly, those with osteoporosis on DXA are more likely to sustain an insufficiency fracture than those with normal bone density or osteopenia, but most insufficiency fractures occur in patients with a normal or low bone mass on DXA as these patients are more common. This also holds true for nonvertebral insufficiency fractures.
Since the advent of DXA in the late 1980s, almost too much emphasis has been placed on BMD and too little emphasis on the presence of an insufficiency fracture for diagnosing osteoporosis. You may hear it said that a patient with an insufficiency fracture does not have osteoporosis because the DXA T -score is between 0 and <2.5. This is simply not true. The presence of an insufficiency fracture far outweighs the information provided by DXA regarding bone strength. The presence of an insufficiency fracture indicates weakened bone (nearly always due to osteoporosis) irrespective of the DXA result. In other words, an insufficiency fracture provides more specific, direct evidence that the bone is weak than areal BMD. Antiosteoporotic treatment can be started based on recognizing an insufficiency fracture irrespective of the DXA result. The National Osteoporosis Foundation (NOF) recommends pharmacologic treatment for patients with a diagnosis of osteoporosis, history of a vertebral or hip fracture, or specific Fracture Risk Assessment Tool (FRAX) score thresholds . Furthermore, osteoporosis can be defined by both T -score ≤−2.5, hip fracture regardless of BMD, or vertebral or other nonvertebral fracture in the setting of low bone mass ( T -score ≤−1.0) . DXA examination is needed in patients with minimal trauma fractures to confirm the diagnosis. It is also the single most important determinant of fracture risk in patients with no prior fracture . Also, in patients with an insufficiency fracture on antiosteoporotic medication, DXA provides a monitor of treatment compliance.
How can you be sure that a vertebral fracture is an insufficiency fracture and not the result of previous trauma? It is usually not possible to distinguish a traumatic fracture from an insufficiency fracture on imaging grounds. Enquiring about moderate or severe trauma incurred at the likely time of fracture will usually allow distinction between these two entities. The incident precipitating a traumatic vertebral body fracture can usually, though not always, be recalled by the patient upon specific questioning. Osteoporotic insufficiency fracture occurs with minor or no trauma. The only caveat is to ensure that the patient is not an epileptic, as severe paravertebral muscle spasms during grand mal seizures can induce vertebral body fractures, often on the upper thoracic spine, in the absence of trauma, particularly in younger men .
63.1.1.3
Harbinger of future osteoporotic fracture
An isolated osteoporotic vertebral fracture is usually the first osteoporotic fracture to occur and usually predates the occurrence of proximal femoral, radial, sacral, or pelvic osteoporotic fractures . In this sense, recognition and appropriate management following an osteoporotic vertebral fracture can prevent or delay the occurrence of subsequent osteoporotic fracture. Over an 8-year period, subjects with prevalent (i.e., preexisting) vertebral fractures have a fivefold increased risk of further vertebral fracture and a threefold increased risk of proximal femoral fracture . Similarly, during a 4-year period following an incident (i.e., new) vertebral fracture, postmenopausal women are four times more likely to develop a further vertebral fracture and twice as likely to develop a proximal femoral fracture than those without an incident vertebral fracture . The overall risk of further vertebral fracture is 20% in the year following incident fracture with relative risk being four times greater in those with severe rather than mild fractures and three times greater in those with multiple (>3) rather than single vertebral fractures . The clinical importance of osteoporotic fracture is recognized by the World Health Organization that defines “severe osteoporosis” as T -score −2.5 plus the presence of an osteoporotic fracture. Recognition is important not least because subjects with a vertebral fracture and a T -score of <2.5 appear to be those most likely to benefit from timely osteoporotic drug therapy. The presence of an isolated vertebral fracture may, through alteration of spinal biodynamics, precipitate additional adjacent vertebral fractures. Such fractures will further increase spinal kyphosis leading to even more vertebral fractures in a process known as “vertebral fracture cascade” ( Fig. 63.2 ). In addition to identifying actual vertebral fracture, the number and severity of vertebral fractures present is also an important marker to note. Histological degradation of iliac crest specimens correlated closely with the graded radiographic severity of vertebral fractures, indicating that the greater the severity of vertebral fracture, the greater the severity of bony architectural deterioration .

63.2
Means of identifying vertebral fracture
Vertebral fractures can be diagnosed clinically with imaging confirmation. Radiography is the most common imaging modality employed, though increasingly vertebral fracture assessment (VFA) by DXA is being used. Both the use of radiography and VFA has been suggested by the NOF, International Osteoporosis Foundation (IOF), and International Society of Clinical Densitometry (ISCD) for targeted screening of appropriate patients to identify patients who have vertebral fractures. Computed tomography (CT) and magnetic resonance imaging (MRI) are other modalities used to diagnose vertebral fractures. Ultrasound has currently no role in the detection of vertebral fractures as the spine is not accessible to a complete ultrasound examination.
63.2.1
Diagnosis of vertebral fractures
Only about one-quarter of vertebral fractures are recognized as a distinct clinical event with acute back pain and muscle spasm as the most common presenting symptoms . The underlying reasons for the lack of acute symptomatology in the vast majority of patients remain unclear. Probably the most effective clinical discriminator of an incident vertebral fracture is a measured height loss of >2 cm or a recalled height loss of >4 cm. A measured height loss of >2 cm has a 35% sensitivity and 94% specificity for incident vertebral fractures , while a recalled height loss of >4 cm has a threefold increased likelihood of identifying a vertebral fracture .
63.2.2
Spinal radiography
Radiography, as the most widely available and least expensive bone imaging modality, can allow one to identify vertebral fracture with a high degree of accuracy. For optimal radiographic assessment a standardized high-quality image is essential. The radiographic protocol should include the C7–S1 vertebrae with finely collimated, properly positioned lateral and anteroposterior (AP) views with the X-ray beam centered at T7 and L3 for the thoracic and lumbar spines, respectively, and a focus—film distance of 100 cm ( Fig. 63.3 ). The C7–T3 vertebral bodies, however, are often not clearly seen on lateral spine radiographs due to superimposition of the scapulae and shoulders, but fortunately, isolated osteoporotic fractures are rare in this region. On the lateral projection, the spine should be parallel to the film so that the vertebral end plates at the level of the central X-ray beam are superimposed and seen as a single dense, well-defined cortical line. As a result of the divergent X-ray beam, the end plates more distant from the centering point will appear concave (“bean can” effect) on lateral projections especially and must not be mistaken for vertebral fracture. This is an expected scenario in patients with degenerative scoliosis, which occurs commonly in the elderly lumbar spine. Usually, a lateral spinal projection will suffice, although a frontal (AP) projection is occasionally useful to (1) determine the anatomical level of a vertebral fracture, particularly in the thoracic spine and (2) to more fully evaluate vertebral configuration in the presence of scoliosis. The AP projection is particularly useful for the thoracic spine where vertebral body outline is not so consistently seen as the lumbar region. One should be aware that mild vertebral fractures may be overlooked on a frontal projection of the thoracic spine. The typical effective dose of ionizing radiation from a lateral and AP thoracic spine projection are 0.3/0.4 mSv, respectively, and 0.3/0.7 mSv for the lumbar region . This full radiographic series is about 25 times greater than a 16-hour return transatlantic flight, which would amount to 0.07 mSv background radiation .

63.2.3
Vertebral fracture assessment by dual-energy X-ray absorptiometry
A new application of DXA machines, incorporating fan beam technology and appropriate software, beyond bone densitometry, is the acquisition of modest resolution lateral thoracic and lumbar spine images to help identify vertebral fractures . Imaging vertebral fractures using DXA is known as “VFA” ( Fig. 63.4 ). VFA can be performed at the same time as bone densitometry with a lateral and frontal image of the spine being obtained in less than a minute. The obvious advantages of VFA over radiography are the convenience, reduced parallax, less radiation, and lower cost .

VFA allows vertebral fractures to be identified with comparable accuracy to radiography, especially for moderate and severe fractures and in doing so, VFA can identify patients with osteoporosis not recognizable by densitometry . Also combining prevalent vertebral fracture status with BMD enhances fracture risk prediction of other vertebral and nonvertebral fractures. This added information can be incorporated into the FRAX model.
The ISCD, NOF, and IOF have published guidelines on when to perform VFA (or spinal radiography) as an accompaniment to densitometry , though, generally, the threshold for performing VFA is reducing .
Since VFA is a digital technique, morphometric vertebral fracture analysis (MXA) is possible. The vertebral body is automatically or manually demarcated by four or six reference points and vertebral body height, height ratios, and average height calculated automatically. Although MXA is routinely undertaken on VFA, this alone is not recommended for fracture diagnosis. The Genant visual semiquantitative (SQ) method is the recommended method to diagnose fractures incorporating vertebral height and contour analysis, such as end plate fracture . MXA can be used to gauge fracture severity . SQ determination of moderate and severe vertebral fractures on VFA compares well with radiography though only moderate correlation exists for mild vertebral fracture . As image quality improves, VFA will be used more widely to identify vertebral fractures.
63.2.4
Computed tomography
Volumetric CT datasets allow detailed analysis of vertebral body morphology enabling accurate identification of vertebral fracture and, in particular, recognition of end plate and/or cortical fractures ( Fig. 63.5 ). Modern low-dose CT systems can produce high-quality CT spine examinations using a dose not much greater than spinal radiography . CT systems equipped with iterative reconstructive technology (ICT) have the ability to reduce dose to less than one-quarter of standard multidetector CT (MDCT) examinations and can acquire fully reliable quantitative CT densitometry data . The effective dose for low-dose lumbar spine CT with iterative reconstruction is 2.1±0.9 mSv while providing comparable diagnostic performance for lumbar spine fractures as standard CT with iterative reconstructive (effective dose 4.9±2.3 mSv) . The major limitations to the more widespread use of CT in vertebral fracture identification and assessment are cost and access to CT time. No doubt, with wider availability, CT will be used increasingly for the fast exclusion of suspected, or closer inspection of known, vertebral fractures . Dual-energy CT examination, using a virtual noncalcium technique, can successfully detect bone marrow edema allowing differentiation of acute from chronic fracture . Automated CT-based systems, which measure bone density and analyze bone texture as well as identify vertebral fracture, are being developed to help in fracture prediction .

63.2.5
Magnetic resonance imaging
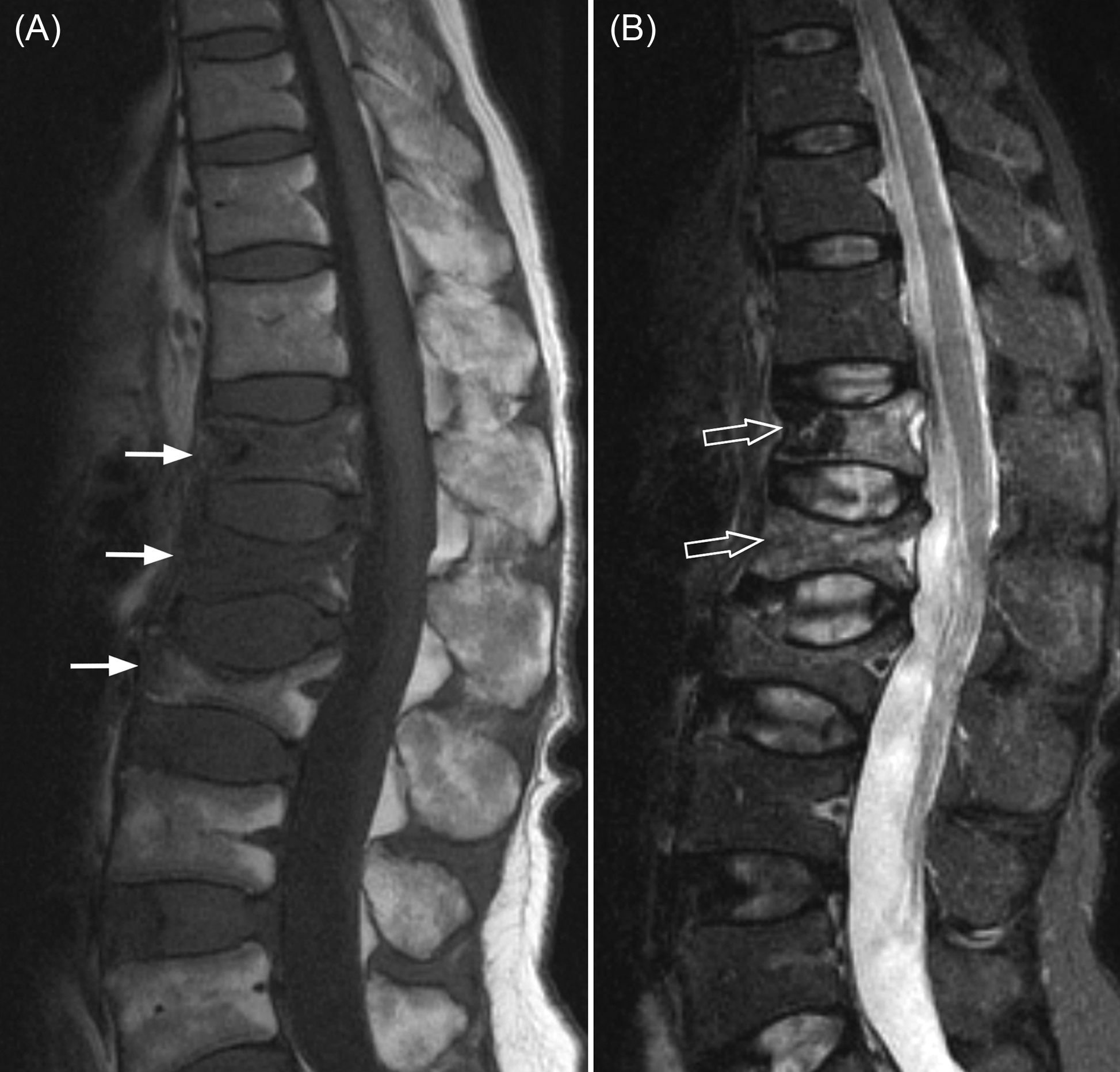
The spine is the most common site for both skeletal metastases and osteoporotic fractures. Even in patients with a known primary malignancy, one in three vertebral fractures will be osteoporotic and not metastatic in origin. MRI, because of its ability to visualize the bone marrow, is the most useful investigation for differentiating osteoporotic from neoplastic fracture ( Fig. 63.6 ). Applying specific imaging criteria, it is nearly always possible to distinguish reliably between osteoporotic and neoplastic vertebral fracture on imaging grounds without having to undertake percutaneous biopsy ( Table 63.1 ). MRI is also sensitive for distinguishing acute/subacute vertebral fractures from chronic vertebral fractures ( Fig. 63.7 ). This is clinically relevant as only acute/subacute vertebral fractures will benefit most from percutaneous vertebroplasty. MRI can also be used to determine fracture nonunion .
| 1. | Preservation of some marrow fat signal within marrow*** |
| 2. | No involvement of pedicles or posterior elements*** |
| 3. | Fluid or gas within vertebral body** |
| 4. | Visible fracture line** |
| 5. | Lack of discrete soft tissue mass*** |
| 6. | Small or absent paravertebral soft tissue swelling** |
| 7. | Absence of epidural mass** |
| 8. | Fracture not of cervical or upper thoracic (T1–T5) vertebral bodies*** |
| 9. | Posterior located triangular fracture fragment* |
| 10. | Nonconvex posterior cortical border* |
| 11. | Evidence of metastases elsewhere in spine* |
| 12. | Near complete fatty marrow of adjacent vertebrae* |
| 13. | Radiographic evidence of osteopenia* |
| 14. | Preservation of trabeculae within fractured vertebral body on CT*** |

63.3
Imaging criteria for identification of vertebral fracture
Vertebral fractures are compressive in nature and are associated with a decrease, in anterior, middle, or posterior vertebral height. As nearly all vertebral fractures are diagnosed on imaging studies, the diagnosis of vertebral fracture clearly depends on the sensitivity of that imaging study to detect changes consistent with vertebral fracture. MRI, because of its ability to visualize morphology and marrow edema, is able to detect acute or subacute vertebral fracture with greater sensitivity than any other imaging technique. However, because of cost and lack of availability, it is clearly not applicable to use MRI to routinely detect vertebral fracture in clinical practice.
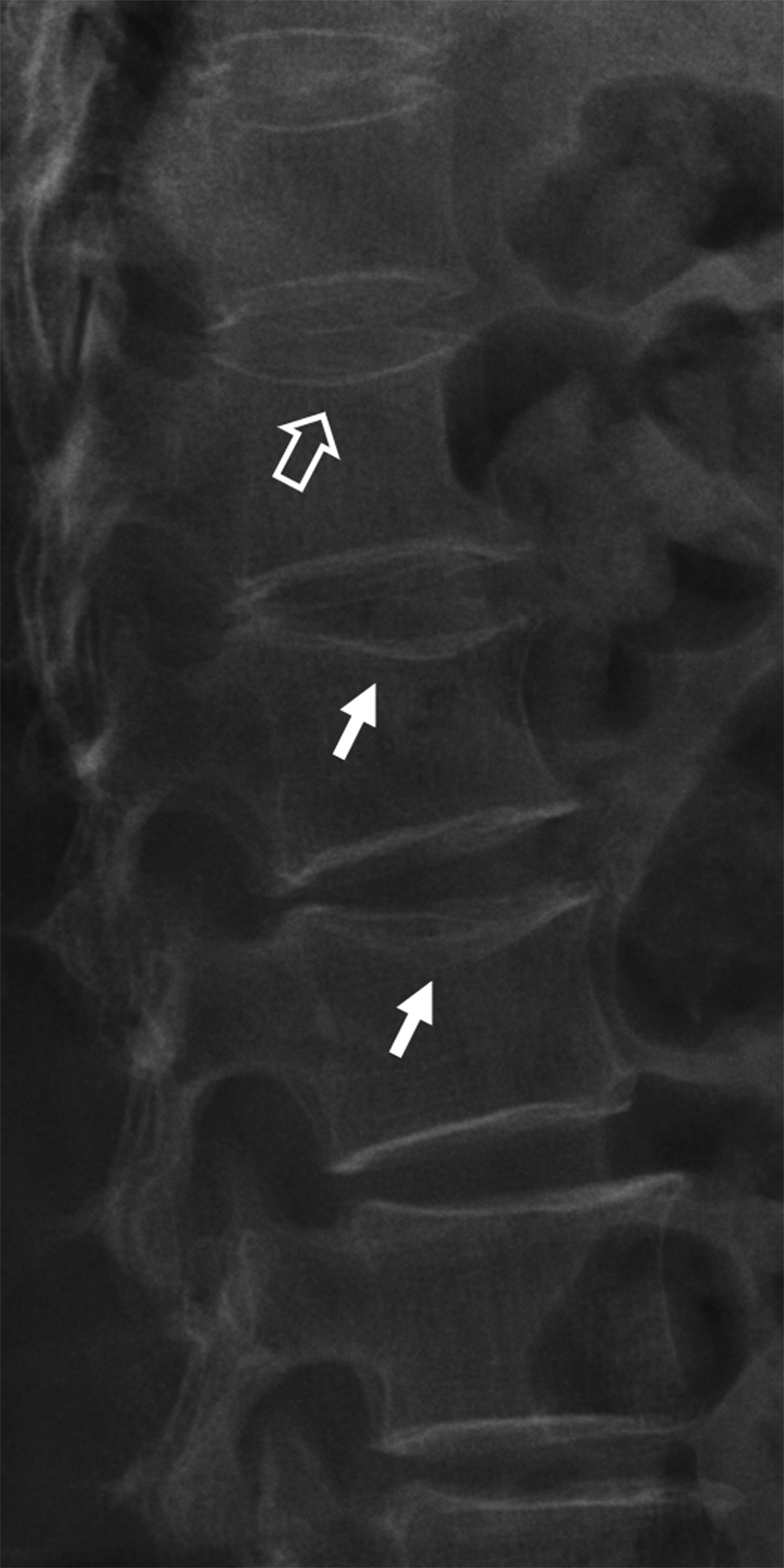
Most vertebral fractures are diagnosed on radiography . The two key diagnostic features are (1) reduction in vertebral height ( Fig. 63.8 ) and/or (2) fracture of the vertebral end plates or vertebral cortical margin ( Fig. 63.9 ). When diagnosing or assessing any vertebral fracture, sequential radiographs or imaging studies are extremely helpful and should be viewed when possible to assess serial change in vertebral body height or morphometry ( Fig. 63.10 ).


63.3.1
Reduction in vertebral body height
Most fractures are diagnosed based on loss of vertebral height assessed by radiography, DXA, CT, or MRI. Although there is no universally accepted definition of what height loss constitutes a vertebral fracture, the most generally accepted working definition is that proposed by Genant et al. a vertebral fracture is diagnosed when vertebral body height is reduced by >20% of the expected vertebral height for that vertebral level, based on the visual subjective judgment of an experienced reader . Less frequently, a height loss of >15% of expected vertebral body height is used .
The expected height of a vertebral body can be compared visually with normal-appearing vertebrae cephalad and caudad to the fractured vertebrae. The normality of any vertebral body with respect to height should be based on the interpretation of an experienced reader. The adjacent vertebrae cannot be assumed to be of normal height since vertebral fractures of varying severity often appear in continuity, and reduced vertebral body height up to 20% can occur in the absence of a fracture. It does require an experienced observer to determine that any vertebral body height is within normal, within a particular clinical setting.
The rationale for the 20% cutoff is that normal physiological wedging of the vertebral bodies occurs in the anterior aspects of the mid-thoracic vertebrae or the upper lumbar vertebrae or the posterior aspects of the lower lumbar vertebrae. In addition, a more diffuse reduction in vertebral height [short vertebral height (SVH)] is a feature of moderate-to-severe discovertebral degeneration in the absence of osteoporosis . Applying the 20% cutoff helps minimize overdiagnosis of vertebral fracture.
So, using height criteria alone, vertebral body height needs to be reduced by at least 20% compared to expect vertebral body height before a fracture is diagnosed. A vertebral body with 20%–25% reduction in height is deemed a mild fracture, 25%–40% a moderate–severity fracture, and >40% reduction in height a severe fracture ( Fig. 63.11 ). Reporting on the severity of vertebral fracture is clinically pertinent because patients with more severe fractures have greater deterioration in bone strength and are more likely to develop subsequent fractures . Also, patients with more than one fracture, those with fractures in both the thoracic and lumbar spine, and those with more than one type of fracture configuration (wedge, biconcave, crush), are also most likely to develop further vertebral fracture so these features should also be noted ( Fig. 63.12 ) .