28.1
Introduction
The clinical significance of osteoporosis is in its outcome of fracture. Fracture is not a benign condition, particularly in the aging population where it occurs most frequently, and it is associated with increased risk of subsequent fracture, significant morbidity and premature mortality. With the increase in numbers of people surviving into older age, the prevalence of fracture is increasing worldwide such that osteoporosis and fractures are a major public health concern. However, there is a significant treatment gap and the majority of people with fractures do not receive appropriate treatment despite the demonstrated efficacy of available antiosteoporosis medications. The reasons for this are complex and multifactorial, including the overemphasis on rare treatment side effects and the fact that many people and their treating physicians may not perceive that they are at high fracture risk.
In the last 10 years or so there has been increasing emphasis on individualized absolute fracture risk rather than relative risk. There are several widely used fracture risk calculators, including the FRAX, the Garvan risk calculator, and the QFracture calculator. The most widely used tool internationally, FRAX, provides a 10-year risk of hip and “major” (hip, wrist humerus, or spine) fractures while the Garvan fracture risk calculator provides a 5- and 10-year risk of hip and all other low-trauma fractures. The QFracture risk calculator provides yearly risk up to 10 years for hip and “major” fracture. These calculators provide an individual estimate of fracture risk based on several clinical risk factors, including prior fracture, with or without bone density. Despite their validation and use in clinical practice, treatment uptake remains poor, around 30% in those who are treatment eligible. Notably, none of these calculators takes into account the time since previous fragility fracture. As this is one of the most important predictors of imminent fracture risk, this risk will be underestimated for patients who experienced a recent fracture. Indeed a focus on a 10-year risk may not seem relevant or have less immediacy than other health concerns facing the elderly subject.
Thus in recent years, there has been a shift in research focus to consideration of imminent fracture risk, in other words, the risk of fracture over the next 1–2 years. Interestingly and perhaps not surprisingly, the risk factors for imminent fracture risk are similar to those of prior studies that focused on subsequent fracture risk with a recent prior fracture being the greatest risk factor for fracture within the next 1–2 years. Falls risk has also been highlighted in a number of studies, including where there has been no prior fracture.
This chapter will therefore focus on imminent fracture risk both in those with and without a prior fracture but focusing on the former where there is most evidence. However, as imminent or subsequent fracture is only one of several adverse outcomes post fracture, this chapter will also focus on disability and premature mortality post fracture.
28.2
Imminent fracture risk
28.2.1
Imminent fracture risk after a prior fracture
It is now well recognized that one of the greatest risks for fracture is having a prior fracture. Indeed this appears to be the case not only for “typical” low-trauma fractures, such as hip, forearm, and humerus fractures but also occurs for virtually any fracture type. Following a nonvertebral fracture, the risk of subsequent fracture increases approximately twofold. Following a vertebral fracture, either clinical or radiographic, the risk may be increased up to fourfold for a subsequent vertebral fracture. However, the timing following the initial fracture is important and crucial for the prediction of imminent fracture risk; the greatest risk occurs close in time to the initial fracture.
28.2.1.1
Timing of fracture
The nonuniformity of risk of subsequent fracture after an initial fracture is not a new concept with the highest fracture risk clustering in time close to the initial fracture having being demonstrated in multiple studies . In the Dubbo Osteoporosis Epidemiology Study, 27% of women and 21% of men experienced a recurrent fracture over a median of 3.3 years (IQR: 1.1–7.0) for women and 2.1 years (IQR: 0.6–5.4) for men; 41% of these recurrent fractures in women and 52% of the recurrent fractures in men occurred in the first 2 years following the initial fracture. Based on life table analysis, the excess refracture risk was elevated for the first 5 years post initial fracture and then decreased progressively over the following years, becoming no longer significant beyond 10 years following the initial osteoporotic fracture . Similar findings were demonstrated in a study from The Netherlands with the relative risk of a subsequent fracture being 5.3, 2.8, and 1.4 at 1, 2–5, and 6–10 years post fracture .
The last few years have seen multiple studies examining the risk of fracture in the first 1–2 years post initial fracture, the period that defines the term “imminent fracture risk.” These studies are in broad agreement that the greatest predictor of imminent fracture risk is a prior fracture. Even within this time line the greatest refracture risk occurs in the first year post initial fracture, and in some studies in the first few months post fracture . In a recent study from Sweden of 242,108 women over the age of 50 years, the risk of subsequent fracture was highest in the first month post fracture and was then steady between 4 and 24 months with a cumulative fracture risk of 7% at 12 months and 12% at 24 months . In another large study of 377,561 slightly older female Medicare beneficiaries aged 65 years and over, these percentages were slightly higher with an overall 10% subsequent fracture incidence at 12 months and 18% at 24 months. By 5 years the cumulative incidence was 31%, again highlighting the high early risk .
Examining these numbers in a slightly different way, it has been well documented that compared with the nonfractured population, following an incident fracture of virtually any type, the risk of a second fracture increases approximately twofold and up to fourfold for a vertebral fracture following an initial clinical vertebral fracture . In the Reykjavik population-based cohort study of almost 19,000 women and men, the relative risk of a second major osteoporotic fracture (including only hip, clinical vertebral, humerus, and forearm) following the first major osteoporotic fracture was 2.7-fold (95% CI, 2.4–3.0) for the first year. The relative risk declined sharply over the subsequent years although was still significantly increased by 10 years at 1.4-fold (95%, CI 1.2–1.6). This corresponded to 20% of individuals refracturing within the first year post fracture .
The reason for the immediacy in high subsequent fracture risk following fracture is still not completely understood. Some authors have postulated immobilization with muscle loss, risk of falling, and deterioration in health, all of which may play a role . However, there are several factors that have been shown to modify this increased imminent fracture risk, including the type of initial fracture, age, and other individual patient characteristics, including falls risk.
28.2.1.2
Type of initial fracture
Virtually any fracture increases subsequent fracture risk in the next 2 years. However, the type of initial fracture modifies the magnitude of this association.
28.2.1.2.1
Initial vertebral fracture
As mentioned earlier, both clinical and radiographic vertebral fracture appear to herald the greatest risk of a subsequent fracture with a fourfold increased risk of subsequent vertebral fracture and closer to twofold for other nonvertebral fracture types . In the recent Medicare beneficiary study of women aged 65 years and older, the percentage of people with any type of fracture at 1 year post initial fracture was on average 10% with the highest prevalence of 14% for those with an initial clinical vertebral fracture . This percentage has been found to be as high as 19.2% for a subsequent radiographically diagnosed vertebral fracture following an initial radiographic vertebral fracture .
As vertebral fractures are generally the primary endpoint for randomized controlled trials (RCT), the data on radiographic vertebral fractures can be quite accurately determined in the placebo groups. Thus the 19.2% 1-year risk quoted previously was approximately fourfold higher than for radiographic vertebral fractures of indeterminate age . The severity of vertebral fracture also affects the risk of subsequent vertebral fracture with the more severe fractures resulting in a higher relative risk of imminent fracture. However, even mild vertebral fractures (grade 1) result in increased risk of subsequent vertebral fractures; in an analysis of 3358 women with osteoporosis in the placebo arms of two strontium ranelate trials, 25% of women with incident mild vertebral fractures sustained another vertebral fracture in the subsequent 2 years .
Nonvertebral fracture risk is also increased after initial vertebral fracture although the risk is not as high as that for imminent vertebral fracture ranging from 1.8- to 2.7-fold depending on the characteristics of the population under study, including age and gender . Radiographic vertebral fractures are also associated with risk of new nonvertebral fractures with the risk increasing based on number and severity of the vertebral deformities .
28.2.1.2.2
Initial nonvertebral fracture
While some studies suggest that the risk for imminent fracture 12 months after the initial nonvertebral fracture is similar for all initial fracture types , others point to higher imminent fracture risk following more major fractures or those fractures more associated with osteoporosis . Some of these differences may relate to the age structure of the population studied and the specific fracture types included.
However, there is consistency among studies that all proximal fractures and almost all distal fractures, with some discrepancies related to ankle fractures, have been associated with increased imminent fracture risk. None of the studies consider fractures of the fingers, toes, face, or skull, but the types of fractures included go well beyond the so-called typical osteoporotic fractures of the hip, humerus, and wrist. Fractures that portend a subsequent imminent fracture risk include rib, clavicle, pelvis, radius/ulnar, distal femur, patella, tibia/fibula. While many of the older studies had previously demonstrated the increased subsequent fracture risk following an initial hip, humerus, or wrist fracture, it has only been in the last 5 years or so that there have been large enough studies conducted to examine other individual fracture types . In general, the imminent fracture risk varies from 1.5- to 2.5-fold depending on the study of population age, fracture locations, and length of follow-up time, with the greatest risk in the first year post fracture .
The role of ankle fracture as a risk for subsequent imminent fracture is still surrounded by some controversy. In some studies, ankle fracture was associated with subsequent fracture in men but not women , while other studies did find an increased risk of subsequent fracture following ankle fracture in women . In the Global Longitudinal Study of Osteoporosis in Women (GLOW) study, ankle fractures in women were associated with subsequent fractures at “any” bone site, but not specifically for hip or vertebral fractures . In a study of 265 ankle fractures, Roux et al. found that they were weak predictors of subsequent fracture, with a 2-year risk of subsequent fracture risk of 3.2% compared with 9.0% for wrist fractures. In that study, ankle fracture was a significant risk factor for imminent fracture only if preceded by a previous fragility fracture or high FRAX score .
Importantly, a hip fracture is commonly seen as the subsequent fracture type. In women over the age of 65 years, hip fracture was the single most common second fracture within the first year . Indeed within 2 years of the initial fracture, the risk of subsequent hip fracture was 4.8% when all women over 65 years were considered together , although these rates did vary by age with lower rates in the younger age-groups and higher rates in the older age-groups (see later). Previous studies had well demonstrated the increased risk of subsequent hip fracture following initial wrist or hip fracture with hip fracture incidence in the first year post initial hip fracture ranging from 2.3% to 5.1%. These more recent studies extend these findings to other types of initial nonvertebral fracture.
28.2.1.3
Number of initial fractures
As well as the site of the prior fracture, it is not surprising that the number of prior fractures also influences imminent fracture risk. In the GLOW study while one fracture was associated with a 1.8-fold increased risk of any imminent fracture within 2 years of follow-up, two prior fractures were associated with a 3.0-fold increased risk and three or more prior fractures with a 4.8-fold increased risk . In another recent study of 2400 women and men aged 50+ years, having multiple baseline fractures increased 2-year imminent fracture risk by 1.8-fold compared to those with only one baseline fracture .
28.2.1.4
Relationship with age
Similar to the risk of an initial fracture, the risk of imminent subsequent fracture risk increases with age. In a study from Tromsø, Norway, the proportion of women with a subsequent fracture within 5 years following the initial fracture rose from 13% in those aged 50–59 years to 24% in those >80 years. In men the corresponding proportions were 10% and 18% . A similarly increased absolute risk of subsequent fracture with age has been reported in other cohorts, including subsequent fracture risk in the 1–2 years post initial fracture . Importantly, despite the increased risk with age, the relative risk of an imminent fracture, if anything, was higher in the younger age-groups than the older. In the Tromsø study the risk of subsequent fracture was between 1.7- and 2.0-fold higher than the risk of initial fracture for younger individuals and between 1.3- and 1.4-fold higher than the risk of initial fracture for older individuals. In the GLOW study where age was examined for different fracture types, the overall trend was similar with the greatest relative risk for imminent fracture occurring in the younger age-groups .
When considering age as a risk for subsequent fracture, the follow-up time and analysis methods need to be carefully considered. Part of the reason for the greater relative risk in the younger age-groups is the increased mortality in the older age-groups so that the subject dies before having time to sustain a subsequent fracture, that is, competing risk of mortality. This particularly affects fracture risk when considered over the longer term and less so for imminent fracture risk . In the Reykjavik study of major osteoporotic fractures in over 18,000 men and women, the immediate risk of a subsequent fracture was similarly high across all age-groups but the relative risk declined over time with a much greater decline in the older age-groups. By 5 years post initial fracture, the relative risk for subsequent fracture remained significant in the 60- and 70-year age-groups but was no longer significant in those aged over 80 years . These differences can be particularly pronounced for hip fracture with high mortality rates particularly in the elderly . Importantly, osteoporotic fractures are themselves associated with increased mortality (see subsequent section on mortality) and thus part of the mortality post fracture may not really be “competing with” but should be considered as part of the outcome post fracture .
28.2.1.5
Effect of gender
There are fewer studies of subsequent fracture in men than women . However, in those studies that have compared subsequent fracture risk between men and women, despite a lower initial fracture risk in men, the risk of a subsequent fracture was similar between the genders . In the Dubbo Osteoporosis Epidemiology Study, the absolute risk of a subsequent fracture following an initial osteoporotic fracture was similar for women and men at every age-group and approximately equal to that of an initial fracture risk for a woman 10 years older or a man 20 years older . For example, a woman or man aged 60–69 years had a subsequent fracture risk that was similar to an initial fracture risk of a woman aged 70–79 or of a man aged 80+ years. Thus, overall, the relative risk of a subsequent fracture was twofold higher for women and more than threefold higher for men. In the Tromsø study the relative risk of a subsequent fracture was higher in men than women (2.0; 95% CI, 1.6–2.4 compared with 1.3; 95% CI, 1.2–1.5), reflecting similar absolute fracture rates . Similar subsequent fracture incidence rates between men and women were reported in the nation-wide Danish registry study over a 10-year follow-up period and in a recent Medicare beneficiary study where first year post fracture absolute risks of recurrent fracture were similar between men and women, except among women aged over 85 years . The higher risk for these very elderly women may be in part due to the increased mortality in men compared with women, particularly in the older age-groups.
28.2.1.6
Role of falls risk
It has been recognized for many years that risk of falling is a strong risk for fracture. This is reflected in the Garvan fracture risk calculator that includes the number of falls in the last year as one of the five clinical risk factors used in its nomogram . Indeed a revised version of FRAX is likely to include this factor (it was not included in the original FRAX as many of the cohorts included in the calculations did not measure falls risk). Not surprisingly, in those studies that have examined risk factors for imminent fracture risk, risk of falling has also been found to be an important independent predictor .
Using a multivariable frailty model, a recent study from the Canadian Multicentre Osteoporosis Study (CaMos) cohort found that among 3228 high-risk women, the number of falls in the last year was one of four independent risk factors for imminent nonvertebral fracture over the subsequent 2 years . The other independent factors included low-trauma fracture in the previous 12 months, low bone density, and poor physical component score on the SF 36. In that study, having had 1 fall resulted 1.5-fold increased risk of imminent fracture with that risk increasing to 1.9-fold with 2 or more falls in the last year. This risk increase was of a similar magnitude to previous fracture. These findings and effect size regarding falls were similar to those in the SOF study although in the latter study only ≥2 falls was a significant factor . It is important to realize that the magnitude of the risk does depend on the study participants and design. In a large study of female Medicare beneficiaries where multiple risk factors were included in a predictive model of imminent fracture risk in the 12 months post fracture, prior fall was associated with a smaller 25% increased risk of imminent fracture .
Examining this issue by looking at falls per se resulted in a similar conclusion. Having a fall within 3 months after a fracture was found to be common, occurring in 18.5% of women and 6.5% of men. Moreover, in these 277 subjects, 12% of these falls resulted in fracture .
28.2.1.7
Role of bone mineral density and other comorbidities
Although low bone mineral density (BMD) is one of the best predictors of initial fractures, its role in predicting subsequent fracture is less clear . This is probably because prior fracture is such a strong determinant of subsequent fracture and because a large proportion of fragility fractures occur in women and men with nonosteoporotic ( T -score>−2.5) bone density levels . In the Dubbo Osteoporosis Epidemiology Study, 54% of initial fractures and 45% of subsequent fracture occurred in individuals with osteopenic or normal bone density . Similar results were found in the Canadian Multicentre Osteoporosis Study (CaMos) where women and men with osteopenia contributed to over 40% of all subsequent fractures .
There have only been a couple of cohort studies specifically examining risk factors for imminent fracture risk. These have found that lower bone density is a significant independent predictor of imminent fracture risk. In the Study of Osteoporotic Fractures (SOF), of 2499 women aged >65 years, a total hip T -score<−3.0 (compared with T -score>−3.0) was associated with a 1.6- to 2.3-fold increased risk of either hip or nonvertebral fracture in the 12 months post initial fracture, with the higher hazards ratios occurring with the lower bone density values . Similar results were apparent in the CaMos. Of 3228 women aged ≥65 years, lower BMD was one of four independent risk factors for 2-year imminent fracture risk. Hazards ratios ranged from 1.3 for women with osteopenia ( T -score<−1.0 and>−2.5) to 3.5 for those with the lowest bone density ( T -score<−3.5) .
In the Dubbo Osteoporosis Epidemiology Study, risk of subsequent fracture was examined for normal osteopenic and osteoporotic bone density. For each level of bone density, relative risk of subsequent fracture was increased >2.0-fold compared with initial fracture risk. For women, this risk increased to 3.2-fold for those with osteoporosis while for men the risk remained more constant over the decreasing levels of bone density. When examined according to type of fracture [hip, vertebral or nonhip nonvertebral (NHNV)], the relative risks for subsequent fracture were generally higher for those with osteoporosis, as were absolute fracture rates .
As well as prior fracture, age, low bone density and falls, other independent risk factors for imminent fracture risk that have been identified in the SOF and CaMos include other measures of poor physical function such as low gait speed <1.0 m/s), use of arms for chair stands or poor tandem stands, and low mini mental state examination (<23) for hip fracture . For nonhip fracture, poor physical function measures, such as low gait speed (in SOF) or low SF physical component summary score (CaMos), were also risk factors, albeit with lower hazards ratios. Smoking and stroke or Parkinson’s disease were also found to be borderline risks in the SOF study .
28.2.1.8
Role of medication
Medications also play a role in increasing imminent fracture risk. The role of corticosteroids in this respect has been well documented. In a study of 244,235 corticosteroid users and matched controls, rate of fracture in the corticosteroid group overall was 2.0/100 person-years compared with 1.3/100 person-years in the control group. After adjusting for confounding factors, the relative risk of fracture in the corticosteroid group compared with the control group was 1.33 overall but rose to 1.6-fold higher for hip fractures and 2.6-fold higher for vertebral fractures. The risk of fracture increased within the first 3 months of corticosteroid use (incidence 1.6/100 person-years in the year prior to starting corticosteroid rising to 2.0/100 person-years in the 3 months after starting). The increased risk was also dose dependent and decreased rapidly after stopping corticosteroids .
In a recent study of 138,526 Medicare beneficiaries, initiation of drugs known to increase fracture, prescribed to subjects who had just had a fracture resulted in an increased risk of a second fracture. The drug classes implicated were selective serotonin reuptake inhibitors, tricyclic antidepressants, antipsychotics, proton pump inhibitors, and nonbenzodiazepine hypnotics. Interestingly, discontinuing therapy at the time of fracture was only beneficial for selective serotonin uptake inhibitors but not for the other high-risk drug classes .
28.2.1.9
Secular trends
There have been a number of studies examining changes in incidence rates of hip fractures over the years, with most data pointing toward a declining rate in Western countries but an increasing rate in most Asian countries such as China , Japan , and South Korea . Notably, this increasing hip fracture incidence was not observed in Taiwan where the rate also decreased after 2005 . The reason behind the secular decline in hip fracture incidence in Western countries is not clear but it may be due to increasing rates of obesity with higher bone density, and potentially improved health services. However, it is less clear if this pattern is mirrored the incidence pattern of subsequent fracture.
The secular trend of hip or major fracture following an initial hip fracture has been reported in two studies using electronic health-care databases from Norway and the United Kingdom. In contrast to the declining incidence rate of initial hip fracture, subsequent hip or major fracture rates were stable or increased . By contrast in an older US study , subsequent hip fracture rates appeared to decline although this trend did not reach statistical significance.
The secular trend of subsequent fracture following any initial low-trauma fracture was investigated in the Dubbo Osteoporosis Epidemiology Study using two separate birth cohorts over two nonoverlapping decades: 1989–99 and 2000–10. This was performed to try to capture both environmental and cohort-specific factors. Despite a decline in initial fracture rates over those two decades, consistent with other Western data, the absolute rate of subsequent fracture did not change in either women or men. The decline in initial fracture rates appeared to be related to a higher proportion of obesity and thus an overall increase in bone density, but despite advances in medical care, there was no improvement in absolute subsequent fracture rates .
28.2.2
Imminent fracture risk without a prior fracture
Although there have been many studies examining initial fracture risk factors over the longer term, there have been very few studies examining fracture risk over the next 1–2 years. One recent case–control study using insurance data of people with osteoporosis aged 50 years and over without a fracture in the preceding 2 years identified several risks for imminent fracture. These included previous falls and risk for falls (such as wheelchair use, mobility impairment, psychoactive medication), increasing age, poorer health status, and specific comorbidities, including Alzheimer’s and central nervous system diseases and psychosis .
Thus, in summary, an initial fracture is the strongest risk factor for subsequent imminent fracture risk. Virtually all types of initial fracture predict an increased risk of imminent subsequent fracture with an increased risk magnitude of approximately twofold and higher for initial and subsequent vertebral fracture. Other important risk factors include increasing age, increased falls risk, lower bone density although the risk increases for every bone density strata level, certain high-risk medications and some comorbidities, particularly those affecting the cognitive and central nervous system. Importantly, the absolute fracture risk in men is similar to that of women, despite their lower risk of initial fractures and there does not appear to be any suggestion of secular decline in subsequent fracture risk despite the declining risk of initial fractures. The importance of this high risk of fracture within the first 1–2 years post initial fracture cannot be overstated as this is the crucial time for intervention where that second fracture with potential adverse long-term sequelae could be prevented.
28.3
Disability and quality of life following osteoporotic fracture
Osteoporotic fractures are associated with significant morbidity and disability particularly in the developed countries. In a study of the worldwide burden of noncommunicable diseases, osteoporosis contributed to 0.83% of the total worldwide burden, while in Europe it contributed to 1.73%. Importantly, this exceeded the burden of any cancer, except lung cancer in Europe . The burden of osteoporotic fracture can be quantified by the disability-adjusted life year (DALY) lost, which represents the number of years lost due to premature mortality or disability. In Europe, osteoporotic fractures accounted for a total of 1,180,000 DALYs in 2010, and this number was expected to increase by 25% in 2015 . Despite this significant contribution of osteoporotic fracture to disability and mortality, treatment rates are declining, and the treatment gap in Europe was estimated to be over 50% for both women and men .
28.3.1
Quality of life following different types of osteoporotic fracture
28.3.1.1
Hip fracture
Hip fracture is the most severe osteoporotic fracture, being associated with over 20% mortality risk in the first 12 months. The survivors are affected by immediate and significant physical disability and loss of independence, which further has a detrimental effect on health-related quality of life (HR-QOL). In a recent systematic review, only between 40% and 60% of hip fracture patients were likely to recover their prefracture level of mobility . Up to 70% of patients recover their prefracture level for basic activities of daily living such as eating, bathing, and getting dressed. However, less than half of the patients recover their ability to perform more complex activities such as meal preparation, community participation, or taking medication. Prefracture functional status was one of the main predictors of physical recovery. Those highly independent prior to hip fracture were most likely to recover their self-care function by 6 months following fracture. By contrast, the recovery rates were significantly lower for aged care or nursing homes residents. In a large retrospective study of over 60,000 nursing home residents with hip fracture only one in five (20%) survived and regained their prefracture function at 6 months following fracture .
Physical limitations that occur immediately following hip fracture are associated with a significant decline in quality of life. In a large cohort study of patients with hip fracture followed for 1 year, the decline in HR-QoL measured by EuroQol 5 Dimensions Score (EQ-5D) mirrored the changes in physical function measured by the Oxford Hip Score (OHS) . The steepest decline of both EQ-5D and OHS occurred in the first 4 weeks, followed by a relative rapid recovery up to 4 months, and little-to-no recovery thereafter. At 1 year following hip fracture, there was still a significant 0.22 (95% CI, 0.17–0.26) deficit in HR-QoL compared to baseline. When interpreting these numbers, the HR-QoL scale varies from 0 to 1 where 1 is perfect health and 0 is death. A similar trend of recovery in the quality of life after hip fracture was reported in a Dutch cohort. In this cohort, both physical and mental scores declined during the first 3 months and recovered between 3 and 12 months, but only mental score recovered to prefracture level at 12 months . Interestingly, in this study, the largest decline in the quality of life was observed in patients younger than 80 and those with a higher prefracture mobility score. However, most likely the steeper decline in somewhat “healthier” patients was due to their higher physical function at baseline. Opposite results were reported in another study, which reported lower rates of recovery for those with lower levels of physical function prior to hip fracture (i.e., care needs prior to fracture) . The number and severity of comorbidities and in particular the presence of dementia at the time of hip fracture are also predictive of a steeper decline in the quality of life .
It is important to consider the high mortality post hip fracture when considering studies of quality of life. If the high mortality following hip fracture is not accounted for in the quality of life assessment, the result could give an overly optimistic picture. This concept is described in a recent comparative study of models of HR-QoL with inclusion and exclusion of participants who died after hip fracture. It was estimated that the exclusion of individuals who died during the follow-up yielded up to a 0.175 (95% 0.025–0.325) increase in HR-QOL . This is a highly significant addition, being more than double the minimum clinical significant difference of 0.074 .
Importantly, it appeared that osteoporosis treatment could have a positive effect not only on reducing the risk of subsequent fracture but also on functional recovery following hip fracture . In a 2-year prospective study of 520 hip fracture patients, osteoporosis treatment, including bisphosphonates, Selective Estrogen Receptor Modulators (SERMS), 1–34 Parathyroid Hormone (PTH), denosumab, calcitonin, and strontium ranelate, particularly when initiated prior to the fracture, was associated with a significant reduction in the rate of subsequent fracture, functional, and quality of life recovery rates .
28.3.1.2
Vertebral fracture
Vertebral fractures represent the most common type of osteoporotic fracture, with symptomatic clinical fractures contributing to about a third of all fractures observed in the community . It is second in severity after hip fracture, being associated with significant risk of subsequent fracture, morbidity and premature mortality . As previously shown, the risk of any subsequent fracture is increased by twofold, while the risk of a second vertebral fracture is over fourfold following a vertebral fracture .
Clinical vertebral fracture is also associated with significant decline in HR-QOL in the acute post fracture period. The International Costs and Utilities Related to Osteoporotic Fractures (ICUROS), an observational multinational study reported the HR-QOL over 18 months following three major osteoporotic fractures, including vertebral fractures from 11 countries . Vertebral fractures were associated with a substantial decline (approximately 0.67) in the HR-QOL at first interview (within 2 weeks) compared to prefracture scores [HR-QOL 2 weeks: 0.17 (0.13–0.20) and prefracture 0.83 (0.81–0.85)]. HR-QOL recovered rapidly, regaining 70% of prefracture value (0.60) in the first 4 months, followed by a plateau. Prefracture functional status was not completely regained at 18 months [HR-QOL 0.70 (0.29) compared to 0.83 (0.23) prefracture] . The main predictors of functional decline post vertebral fracture were prefracture HR-QOL, hospitalization for vertebral fracture as well as the presence of a prior fracture . In the GLOW, vertebral fractures compared to all other fractures, including hip fractures, were associated with the most significant decline in self-care activities, pain/discomfort, as well as the largest drop in general health status .
Prevalent radiographic vertebral fractures may also be associated with impaired HR-QOL, but the evidence is less clear. In a recent Italian study, undiagnosed vertebral fractures that were present in one in four women without back pain were associated with a significant impairment in the quality of life assessment . In a systematic review and metaanalysis of 16 studies, including 14 cross-sectional, one case–control, and one using baseline data from an RCT, prevalent vertebral fracture also impacted quality of life but this was not thought to be over and above the presence of osteoporosis per se . Impaired quality of life was observed in nine studies, and after pooling all the results vertebral fracture was associated with a half SD lower HR-QOL compared to those without vertebral fracture. Sensitivity analyses indicated that the impaired HR-QOL was beyond that expected by aging process and was not mediated by the presence of pain. Mental function impairment was found in 4 out of the 16 studies analyzed. After pooling all 16 studies the standardized mean difference of HR-QOL was significantly lower for those with vertebral fractures [0.20 (0.06–0.34); P =.005]. However, it is still possible that aging may play a role in this difference, as a sensitivity analysis restricted to age-matched case–controls reported no difference in mental scores between the fracture and nonfractured groups .
Vertebral fractures, more than other osteoporotic fractures, are associated not only with functional decline but also with complex psychological issues stemming from postural changes. Multiple vertebral fractures lead to postural changes such as height loss, kyphosis, and abdominal protrusion. These physical changes can lead to serious psychological conditions such as anxiety, depression, and low self-esteem, all of which are poorly managed clinically. Over time, these conditions aggravate leading to inactivity, social isolations, and loss of independence. A recent qualitative study documented the experience of 10 women with vertebral fracture. The participants described life in turmoil and chaos, inability to find stability, and fear of isolation. Authors have identified five major themes associated with vertebral fractures, including struggling to understand a deceiving body , breakthrough pain fueling fear , fearing a trajectory into isolation , concerns of dependency , and fearing an uncertain future .
As discussed for hip fracture, treatment with antiresorptive medication may lead to an improvement in the quality of life in individuals with vertebral fracture. In the European Forteo Observational Study, an observational study of quality of life in women with severe osteoporosis from eight European countries; treatment with teriparatide for 18 months substantially improved HR-QOL (measured by EQ-5D). Importantly, this effect was maintained in the following 18 months when patients received other osteoporosis treatments . The improvement in HR-QOL was highest for those with prior vertebral fracture and no incident fracture. HR-QOL was temporarily attenuated, as expected by the presence of incident fracture. However, even in these groups with incident fracture, HR-QOL reached an overall improvement over the baseline measurement. These findings suggest that treatment may reverse the adverse effects of vertebral fracture on the quality of life. However, this study is limited by its observational design. Future RCTs with detailed quality of life measurements throughout the follow-up are needed to fully answer the efficacy of treatment on quality of life.
28.3.1.3
Nonhip nonvertebral fracture
NHNV fractures represent half of all fragility fractures and contribute to a large proportion of the burden of subsequent fractures and excess mortality in the community . Accumulating evidence shows that all NHNV, except perhaps ankle fractures, are associated with increased risk of subsequent fractures and that proximal fracture sites (i.e., humerus, pelvis, femur, tibia/fibula) are also associated with increased mortality risk.
The impact of NHNV fractures on mobility and quality of life is not reported as well as that for hip and vertebral fracture. In the GLOW cohort, major NHNV fractures, including pelvis, upper and lower leg, upper arm, shoulder, knee, and elbow, were associated with a significant decline in HR-QOL from 0.70 at baseline to 0.66 at 1 year, which was similar to the magnitude of decline observed for hip fracture (0.64–0.60) . There was also an increase in the number of women reporting difficulties with self-care following major NHNV fracture (+6% for self-care and +10% for activities). In this cohort minor NHNV fractures, including wrist, hand, ankle, foot, rib, and clavicle, were also associated with a decline in HR-QOL (0.72–0.70 in the first year post fracture). In another prospective cohort, including only minor fractures, frailty predicted the decline in both physical and mental HR-QOL scores in these types of fractures . Individuals classified as frailest compared to fittest, according to the Canadian Study of Health and Aging Clinical Frailty Scale tool, had significantly lower physical HR-QOL scores at both 3 months (49.3±3.7 vs 60.9±2.0) and 6 months (48.7±3.8 vs 61.1±1.8) and lower mental HR-QOL scores at 3 months (59.5±4.4 vs 69.6±1.9) .
The pattern of the decline in quality of life over 18 months following several individual NHNV fractures such as distal forearm, humerus, and ankle fractures was reported in the Australian arm of ICUROS . Patients with NHNV fractures had higher prefracture HR-QOL compared to those with hip or vertebral fractures. Those with wrist fractures had the highest prefracture HR-QOL scores (0.90) followed by those with fractures of the ankle (0.86) and humerus (0.82). HR-QOL declined for all fractures in the first 4 months: ankle 61%, humerus 59%, and wrist 36%. Following this immediate phase, HR-QOL started to improve. By 12 months, there was still some deficit for patients with fractures of the ankle 8.1%, humerus 4.9%, and wrist 2.2%. However, by 18 months, all NHNV fracture HR-QOL scores returned to prefracture HR-QOL levels . Similar results for wrist fractures were reported in the global ICUROS. Female gender and age over 80 were reported as independent predictors for the functional decline at 6 months following distal forearm fracture in a Spanish study .
28.3.2
Institutionalization
One of the most devastating consequences of osteoporotic fracture is loss of independence and admission to nursing home. The risk of institutionalization following hip fracture is well recognized and reported to affect up to 30% of the patients in the first year post fracture. The main predictors of institutionalizations following hip fracture are older age, poor prefracture functional status, and the presence of cognitive impairment or dementia . Male gender was also reported as an independent predictor in several but not all studies. Importantly, in one study the burden of institutionalization for hip fracture was as high as that following stroke and higher than that for myocardial infarction or pneumonia .
The risk of institutionalization following nonhip fracture is far less well documented than for hip fracture. However, two recent large studies of health administrative databases have raised the awareness of risk of nursing home admission for all major nonhip fractures . In a German health insurance administrative database, the rates of transfer to nursing homes in the first 6 months were evaluated for fractures of the hip, clinical spine, humerus, distal forearm, pelvis, and lower extremities. Patients with pelvic fractures had similar rates of institutionalization as those with hip fractures (15/100 patients in women and 11/100 patients in men for hip fractures and 14/100 patients in women and 9/100 patients in men for pelvis fractures), followed closely by spine fracture (11/100 patients in women and 8/100 patients in men). The lowest risk of institutionalization was reported for distal radius fracture (4/100 patients in women and 1/100 patients in men). Predictors of institutionalization were increasing age, higher number of comorbidities and female gender . Similarly, high rates of institutionalization following nonhip fractures were also reported in a Canadian comprehensive health-care database from the province of Manitoba over 20 years. However, in this study, institutionalization was higher for men than women. In comparison to matched controls without fracture, the relative risk of institutionalization was highest following hip fracture (4.9 for men and 2.8 for women), followed by fractures of the vertebrae (3.1 for men and 2.2 for women), humerus (2.4 for men and 1.6 for women), and wrist (2.1 for men and 1.4 for women). Another important finding from this study was the increasing rates of fracture institutionalizations over the 20 years for all fracture types and in both genders. The authors postulated that the increase in the rate of nursing home transfers over the time could be due to an increase in the number of associated chronic conditions over time, perhaps also due to increasing longevity .
Thus in summary, all fractures are associated with significant impairment in quality of life and increased risk of institutionalization. While both of these outcomes are worse for hip and vertebral fractures, NHNV fractures are also associated with disability post fracture. This is an important concept, albeit generally not well recognized, given the large burden (over 50% of all fractures) of NHNV fractures in the elderly. Prefracture status is often not recovered for the major fractures, and even for the more minor fractures it can take up to 18 months to return to prefracture levels of functioning.
28.4
Risk of mortality following osteoporotic fractures
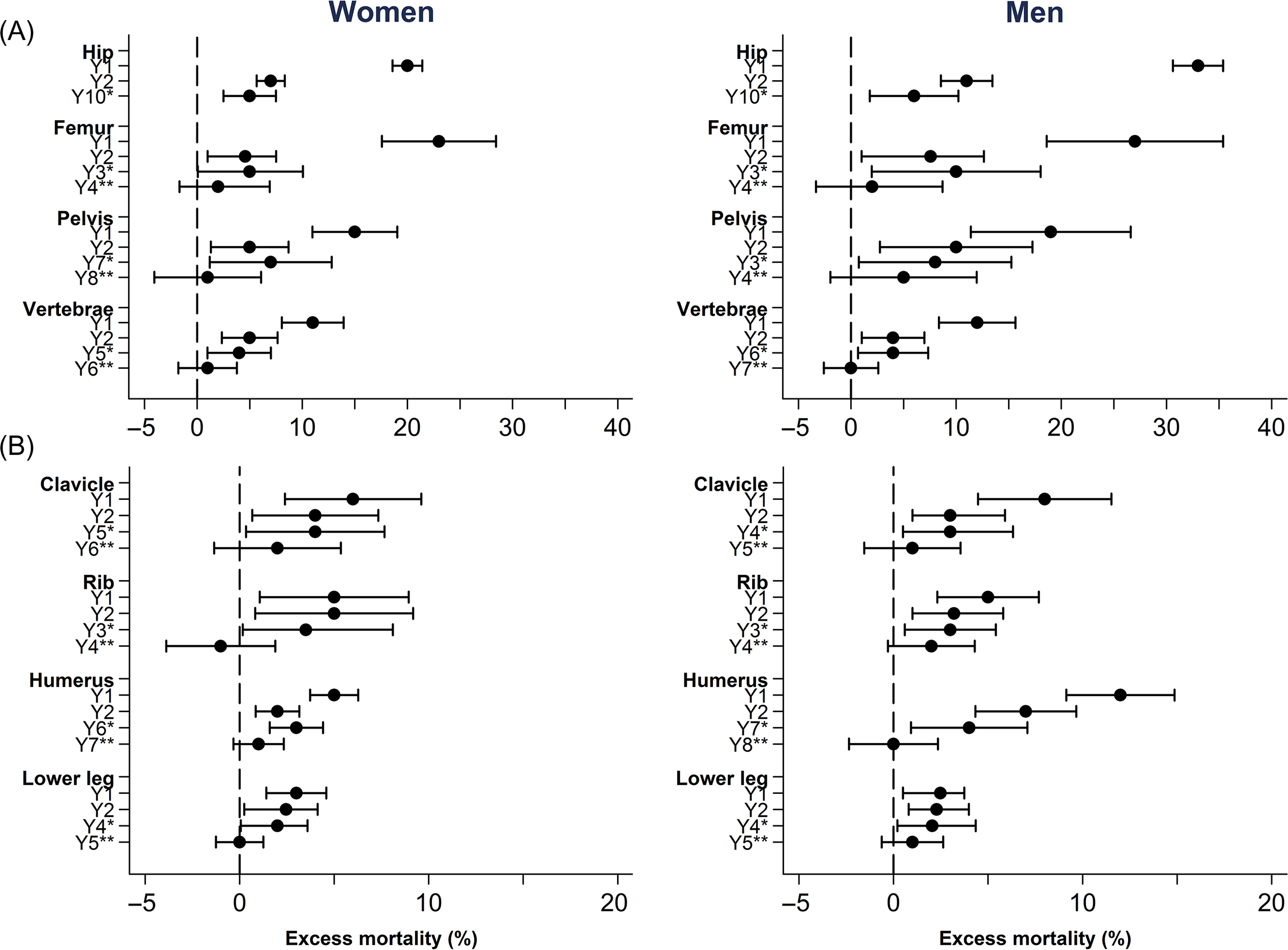
Increased mortality risk following hip and vertebral fractures is well recognized with increasing evidence that other major fractures, particularly at the proximal sites (e.g., humerus, distal femur, pelvis), are also associated with increased mortality risk. Minor fractures, such as those at the distal sites (e.g., forearm, ankle), have also been associated with increased mortality in some but not all studies . Importantly, the pattern of postfracture mortality is not constant with time, being highest immediately after the fracture, followed by a decline toward the background population mortality, except for hip and perhaps vertebral fractures, for which excess mortality persists for at least 10 years .
Overall, the magnitude of the fracture mortality association ranges between 15% and over twofold above the age- and gender-expected population mortality risk, depending predominantly on the type of initial osteoporotic fracture and length of time post fracture .
The mechanism for the increased mortality risk is most likely multifactorial. The number and severity of comorbidities at the time of fracture may play a role in postfracture mortality; however, the evidence is not consistent among studies . Several risk factors for fracture such as low bone mass, bone loss , muscle weakness , and sarcopenia have also been found to be associated with mortality risk independent of fracture and thus could also contribute to postfracture mortality risk .
28.4.1
Mortality risk according to fracture type
28.4.1.1
Hip fracture
Hip fractures are associated with the highest mortality rates among all osteoporotic fractures . The magnitude of hip fracture mortality depends on the time from the fracture and age. Up to 30% of individuals with hip fracture are estimated to die in the first 2 years post fracture . This equates to an excess mortality of over twofold above the expected general population mortality . Two recent metaanalyses quantified long-term excess mortality following hip fracture. The first one reported yearly excess mortality from 22 cohorts in women and 17 in men . Using a life table approach, investigators estimated an annual posthip fracture excess mortality of 8%, 11%, 18%, and 22% at 1, 2, 5, and 10 years for women with hip fracture at age 80 compared to women without fracture. In men the estimated annual posthip fracture excess mortality was even higher: 18%, 22%, 26%, and 20% for 80-year-old men with hip fracture compared to those without fracture. The second metaanalysis reported long-term mortality risk following hip fracture from 8 cohorts from Europe and the United States, controlling for lifestyle factors and comorbidities. Mortality risk was highest during the first year [2.78 (95% CI, 2.12–3.64)] and then declined [1.89 (95% CI, 1.50–2.37)] between 1 and 4 years but remained elevated beyond 8 years [1.79 (95% CI, 1.57–2.05)]. Importantly, the presence of co-morbidities had an additive effect on mortality risk .
Although hip fracture occurs predominantly in the older age-groups, younger individuals have higher excess mortality compared with their nonfractured peers than older individuals. For example, in the Dubbo Osteoporosis Epidemiology Study, younger women (<75 years) with hip fracture had an over eightfold increased mortality risk compared to a twofold increased risk for those older than 75 . Similar data on higher excess mortality in younger women with hip fracture versus older women has also been reported in other studies, even after adjusting for comorbidities and other risk factors.
Other predictors of hip fracture mortality are gender and race. Absolute mortality following hip fracture is higher in men than women , but this difference is attenuated after taking into account the gender differences in background mortality risk . Ethnicity appears also to play a role in hip fracture mortality, although the cause of this disparity is not clearly understood. In an earlier study of the US Medicare claims database, Black women and men had higher excess mortality immediately after hip fracture compared to White women and men. Furthermore, the difference was not explained by differences in age or number and severity of comorbidities . A higher mortality for Black women as well as women of “other ethnicities” (mainly of Arab descent) compared to White women were also reported in a more recent study from the UK Clinical Practice Research Datalink (CPRD) database .
The role of comorbidities in hip fracture mortality has been widely reported, with conflicting findings. While some studies have suggested that comorbidities accounted for up to 50% of short-term mortality , others did not find that comorbidities contributed significantly to any of the posthip fracture mortality.
Nevertheless, the prefracture functional status plays an important role in the excess mortality risk following hip fracture. A poor score on the American Society of Anaesthesiologists grading, worse cognitive function, general health, and ambulatory status, were all significant predictors of mortality risk immediately after fracture .
Several studies have reported causes of death obtained from death certificates. In a large Swedish study, during the first year following hip fracture, women and men were more likely to die of cardiovascular disease (more than threefold), cancer (more than fourfold in women and 1.9-fold in men), and pneumonia (3.4-fold for women and 4.7-fold for men). After the first year, the causes of death were similar for fracture and non fracture subjects, except for pneumonia, which was still elevated in men with hip fracture . However, it needs to be remembered that death certificate reporting is not very reliable and other studies have not found any differences between hip and nonhip fracture populations .
28.4.1.2
Vertebral fracture
Vertebral fractures are the most common fracture type, representing approximately a third of all fractures, but pose a challenge to study as only one-third (at most) present clinically and even many symptomatic patients do not require hospitalization . Thus vertebral fractures have been far less well studied than hip fractures. However, there have been several population-based studies and a randomized controlled study that examined mortality post vertebral fracture . All of these have demonstrated an increased mortality risk, ranging between 42% and over threefold compared to no fracture. The excess mortality was on average lower than that for hip fracture in several studies, but with overlapping 95% CIs.
Similar to hip fractures, excess mortality following vertebral fractures varies with time, being highest in the immediate interval post fracture. The excess mortality then gradually decreases but remains elevated for up to 3–10 years depending on the study and gender of participants. In the Danish National Database, the highest mortality risk was observed in the first year for both women and men and persisted for 5 years in women and 6 years in men . In the European Vertebral Osteoporosis Study, the survival curves for vertebral fractures diverged from those of the age-matched general population for 3 years in men and up to 10 years in women .
The magnitude of mortality risk following vertebral fracture also varies by age and gender. Although absolute mortality relative to expected mortality increases with age, similar to hip fractures, the highest excess mortality following vertebral fracture is observed in younger age-groups. In the Dubbo Osteoporosis Epidemiology Study, individuals who experienced a symptomatic vertebral fracture below 75 years of age had significantly higher excess mortality compared to those who had their first vertebral fracture after 75 years for both women [age-adjusted SMR 3.8 (2.5–5.8) and 1.5 (1.1–1.8)] and men [age-adjusted SMR 4.2 (2.4–7.3) and 1.9 (1.4–2.6)] . Similarly, absolute mortality risk following vertebral fracture has consistently been found to be higher in men than women. However, this gender difference disappears after accounting for the higher population mortality rates in men.
The effect of radiographic vertebral fractures on mortality risk is less well studied. In the initial and follow-up studies from the Dubbo Osteoporosis Epidemiology Study, radiographic vertebral fractures were associated with a similar increased mortality risk as symptomatic fractures . In another study from the Dubbo Osteoporosis Epidemiology Study, radiographic vertebral fractures were associated with high risk of incident symptomatic vertebral fracture, which increased mortality risk . Certainly the presence of multiple vertebral fractures has been found to be associated with increased mortality risk in several studies . The role of a single vertebral deformity on mortality is less clear with contradictory findings , and any effect may be mediated through increasing risk of new clinical vertebral fractures.
Vertebral fractures, by contrast with other osteoporotic fractures, are associated with pulmonary conditions due to kyphosis, which can contribute directly to excess mortality associated with this type of fracture. Severe kyphosis is a well-known risk factor for pulmonary disease due to a reduction in respiratory reserve and restrictive lung disease. In the SOF, women with vertebral fracture had an increased risk of mortality due to chronic obstructive pulmonary disease and pneumonia, even after adjusting for smoking . Vertebral fracture has also been associated in several studies with cancer, even after the exclusion of metastatic fractures . In the Malmo population the incidence of cancer in women with vertebral fracture was significantly higher than in the general population .
Notably, it has been shown that kyphoplasty may be associated with better survival rates than either no treatment or vertebroplasty . In a recent study, vertebral fractures treated nonoperatively had the highest mortality risk, followed by vertebroplasty and kyphoplasty. After adjustment for covariates, including age, gender, and comorbidities, those treated by kyphoplasty had approximately 20% lower mortality risk than vertebroplasty [0.80 (95% CI, 0.77–0.84). In addition, kyphoplasty was associated with shorter hospital stays, and decreased likelihood of complications such as pneumonia and decubitus ulcer .
28.4.1.3
Nonhip nonvertebral fracture
NHNV fractures are the most common group of osteoporotic fractures, representing over half of all fractures occurring in the community . However, despite their frequency, there are very few studies on their adverse outcomes. Increased mortality risk associated with major NHNV fracture (a group of fractures, including pelvis, distal femur, multiple ribs, and humerus) was first demonstrated in the Dubbo Osteoporosis Epidemiology Study over a 5-year follow-up . Major fractures were associated with 2.0- to 2.2-fold increased mortality risk for both women and men, while minor fractures (forearm, wrist, metacarpal, ankle, and metatarsal) were not associated with mortality risk. Subsequently, a long-term follow-up study (>18 years) from the same cohort reconfirmed the excess mortality associated with major fracture and also demonstrated increased mortality for minor fractures in the older (>75 years) individuals, who had a 37%–82% mortality risk increase . Notably, given that NHNV fractures represented half of all incident fractures in the cohort, they were responsible for over 40% of all deaths and contributed to a third of all the excess mortality. Similarly, high mortality risk associated with major fracture was reported in a hospital database study from Maastricht . In the Canadian Multicentre Osteoporosis Study, all NHNV fractures were associated with 38% significantly higher mortality risk increase after adjusting for all risk factors in women but did not reach statistical significance in men . The fracture burden in the population was estimated using population impact number (PIN) representing the number of deaths attributable to fracture in the population, and case impact number (CIN) representing the number of deaths attributable to fracture among all deaths in the population. In this study, NHNV as a group contributed to one death for every 777 women (PIN). Conversely, 1 death out of every 15 deaths (CIN) was attributable to this group of fractures. These numbers were greater than PIN and CIN for the combined hip and vertebral fractures. The overall impact was greater than that for smoking on coronary heart disease– or lung cancer–related deaths in British male physicians .
There have been few large epidemiological studies that have reported mortality risk following individual types of NHNV osteoporotic fractures. Significant mortality risk has consistently been associated with fracture at proximal sites such as the pelvis, humerus, ribs, and femur. However, evidence for increased excess mortality following fractures at distal sites such as the forearm and ankle has been less consistent, while fractures of the hands and feet have not been found to be associated with excess mortality . Interestingly in a recent study from the Danish National Database, clavicle and proximal but not distal tibia/fibula fractures were also found to be associated with increased mortality ( Fig. 28.1 ) .