The vagina is a muscular, dilatable tube, approximately 7.5 cm in length, located posterior to the base of the bladder and urethra and anterior to the rectum.
The upper fourth of the posterior wall is separated from the rectum by a reflection of peritoneum called the pouch of Douglas.
The lymphatics in the upper portion of the vagina drain primarily via the lymphatics of the cervix; those in the lowest portion either drain cephalad to the cervical lymphatics or follow drainage patterns of the vulva into femoral and inguinal nodes. The anterior vaginal wall usually drains into the deep pelvic nodes, including the interiliac and parametrial nodes.
Vaginal cancers occur most commonly on the posterior wall of the upper third of the vagina. Plentl and Friedman (21) found that 51.7% of primary vaginal cancers occurred in the upper third of the vagina and 57.6% on the posterior wall.
Tumors originating in the vagina may spread along the vaginal wall to involve the cervix or vulva. However, if biopsies of the cervix or the vulva are positive at the time of initial diagnosis, the tumor cannot be considered a primary vaginal lesion.
Because of the absence of anatomic barriers, vaginal tumors readily extend into surrounding tissues, including the paracolpal and the parametrial tissues. Lesions on the anterior vaginal wall may penetrate the vesicovaginal septum; those on the posterior wall may eventually invade the rectovaginal septum.
The incidence of positive inguinal or pelvic nodes at diagnosis varies with stage and location of the primary tumor.
Because the lymphatic system of the vagina is complex, any nodal group may be involved, regardless of the location of the lesion (21). Involvement of inguinal nodes is most common when the lesion is located in the lower third of the vagina.
Distant metastases occur in approximately 23% of patients.
In squamous cell carcinoma, metastases to the lungs, liver, or supraclavicular nodes may occur, particularly in patients with advanced disease.
Abnormal vaginal bleeding (dysfunctional bleeding or postcoital spotting) is the presenting symptom in 50% to 75% of patients with primary vaginal tumors. Vaginal discharge is common.
Dysuria and pelvic pain are less frequent presenting complaints; they occur when tumor has spread to adjacent organs.
TABLE 38-1 Diagnostic Workup for Vaginal Tumors | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Diagnostic procedures for patients with vaginal tumors are shown in Table 38-1.
In addition to a complete history and physical examination, speculum examination and palpation of the vagina are essential. The speculum must be rotated as it is withdrawn so that anterior or posterior wall lesions, which occur frequently, are not overlooked.
Bimanual pelvic and rectal examinations in the office and under anesthesia are integral elements in the clinical evaluation.
Exfoliative cytology studies may detect early squamous cell lesions of the vagina, but not clearcell adenocarcinomas (CCAs), which often grow in submucosal locations.
Schiller’s test (with Lugol’s solution) and colposcopy are useful for directed biopsies in abnormal sites in the vagina.
A metastatic evaluation including cytoscopy and proctosigmoidoscopy should be performed on patients with pathologically confirmed invasive vaginal carcinoma beyond stage II.
In addition to the chest x-ray, intravenous pyelogram, and barium enema or air contrast (when indicated), computed tomography, and magnetic resonance imaging of pelvis and abdomen have been increasingly used in evaluation of these patients.
TABLE 38-2 Clinical Staging of Malignant Tumors of the Vagina | |||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||
Staging is best performed jointly by the gynecologic and radiation oncologists, with the patient under general anesthesia.
Multiple biopsies of the cervix are mandatory to rule out a cervical primary tumor. If there is a concomitant malignant lesion of the same histology in the cervix or if biopsies demonstrate a similar tumor, the lesion must be classified as a primary cervical carcinoma and staged accordingly.
Tumors are staged using the International Federation of Gynecology and Obstetrics (13) or American Joint Committee on Cancer staging system (Table 38-2 and Fig. 38-1) (1).
Epidermoid carcinoma accounts for approximately 90% of primary vaginal tumors, most of which are nonkeratinizing and moderately differentiated.
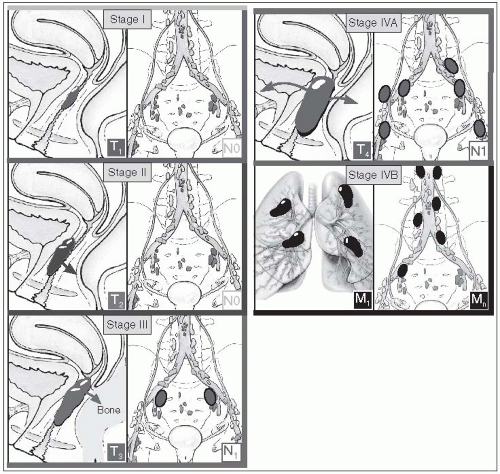
FIGURE 38-1 Clinical staging of cancer of the vagina. TNM markings on the drawings are the AJCC definitions (see Table 38-2). (Adapted from Rubin P, Hansen JT. TNM Staging Atlas. Philadelphia, PA: Lippincott Williams & Wilkins, 2007:419, with permission.)
Primary vaginal carcinoma in situ and invasive carcinoma of the vagina have been reported in a few patients previously treated for carcinoma of the uterine cervix (12); these vaginal lesions may be marginal recurrences of the cervical lesions.
Verrucous carcinoma is a distinctive variant of well-differentiated squamous cell carcinoma that rarely occurs in the vagina (22).
Adenocarcinomas comprise approximately 5% of primary vaginal tumors and are found more frequently in older women. They usually arise from the Bartholin or Skene submucosal glandular epithelium. CCA of the vagina may be found in young patients (24).
Adenoid cystic carcinoma of the vagina is rare. Until 1996, only 45 cases of adenoid cystic carcinoma of Bartholin’s gland were reported in the world literature.
Neuroendocrine small-cell carcinoma may occur in the vagina, either in pure form or associated with squamous or glandular elements. It tends to be aggressive, with a propensity for early spread.
Sarcomas (smooth muscle tumors) are the most common mesenchymal tumor of the vagina in adults.
Leiomyosarcomas comprise 68% of vaginal sarcomas in adults, whereas rhabdomyosarcomas comprise less than 2%. Rhabdomyosarcoma of the female genital tract represents approximately 90% of cases occurring in children under 5 years of age (9).
Malignant melanomas account for 2.8% to 5.0% of all vaginal neoplasias (23). Hematogenous and lymphatic dissemination frequently occur; the 5-year survival rate is less than 10%.
Malignant lymphoma may be localized to the female genital tract or occur as part of a widespread disease process (8).
Most primary malignant lymphomas involving the vagina are the diffuse large-cell type, but nodular lymphomas may also occur.
Characteristically, the mucosa is intact; a submucosal mass is frequently is seen.
Marker studies are useful in equivocal cases of lymphoma-like lesions.
The clinical stage of the tumor is the most significant prognostic factor, reflecting size and depth of penetration into the vaginal wall or surrounding tissues (5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








