The larynx is divided into three regions: the supraglottic (epiglottis, false vocal cords, ventricles, aryepiglottic folds, arytenoids), glottic (true vocal cords, anterior commissure), and subglottic (located below the vocal cords) (5) (Fig. 19-1).
The lateral line of demarcation between the glottis and the supraglottic larynx clinically is the apex of the ventricle. The demarcation between the glottis and the subglottis is ill defined, but the subglottis is considered to begin 5 mm below the free margin of the vocal cord and to end at the inferior border of the cricoid cartilage and the beginning of the trachea.
The laryngeal arteries are branches of the superior and inferior thyroid arteries.
The intrinsic muscles of the larynx are innervated by the recurrent laryngeal nerve. The cricothyroid muscle, an intrinsic muscle responsible for tensing the vocal cords, is supplied by a branch of the superior laryngeal nerve. Isolated damage to this nerve causes a bowing of the true vocal cord, which continues to be mobile, although the voice may become hoarse.
The supraglottic structures have a rich capillary lymphatic plexus. The trunks pass through the pre-epiglottic space and the thyrohyoid membrane and terminate mainly in the subdigastric lymph nodes; a few drain to the middle internal jugular chain lymph nodes.
There are essentially no capillary lymphatics of the true vocal cords. Lymphatic spread from glottic cancer occurs only if tumor extends to the supraglottic or the subglottic areas.
The subglottic area has relatively few capillary lymphatics. The lymphatic trunks pass through the cricothyroid membrane to the pretracheal (Delphian) lymph nodes in the region of the thyroid isthmus. The subglottic area also drains posteriorly through the cricotracheal membrane, with some trunks going to the paratracheal lymph nodes and others continuing to the inferior jugular chain.
Cancer of the larynx represents approximately 2% of all cancer diagnoses and is the most common type of head-and-neck cancer (skin excluded).
The ratio of glottic to supraglottic carcinoma is approximately 3 to 1.
Cancer of the larynx is strongly related to cigarette smoking. The risk of tobacco-related cancers of the upper alimentary and the respiratory tracts declines among ex-smokers after 5 years and approaches the risk of nonsmokers after 10 years of abstention (27).
Destructive suprahyoid epiglottic lesions tend to invade the vallecula and pre-epiglottic space, lateral pharyngeal walls, and the remainder of the supraglottic larynx.
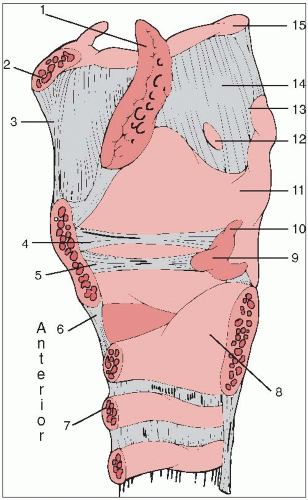
FIGURE 19-1 Midsagittal view of the right larynx. (1) Epiglottis, (2) body of the hyoid bone, (3) median thyrohyoid ligament, (4) vestibular ligament, (5) vocal ligament, (6) cricothyroid membrane, (7) tracheal ring, (8) cricoid cartilage, (9) arytenoid cartilage, (10) corniculate cartilage, (11) thyroid cartilage, (12) foramen for superior laryngeal nerve and artery, (13) superior horn of thyroid cartilage, (14) thyrohyoid membrane, (15) greater horn of the hyoid bone. The anterior is to the left of the drawing
Infrahyoid epiglottic lesions grow circumferentially to involve the false cords, aryepiglottic folds, medial wall of the pyriform sinus, and the pharyngoepiglottic fold. Invasion of the anterior commissure and cords and anterior subglottic extension usually occur only in advanced lesions.
Extension of false cord tumors to the lower portion of the infrahyoid epiglottis and invasion of the pre-epiglottic space are common.
It may be difficult to decide whether aryepiglottic fold/arytenoid lesions started on the medial wall of the pyriform sinus or on the aryepiglottic fold. Advanced lesions invade the thyroid, epiglottic, and cricoid cartilages, and eventually, the pyriform sinus and postcricoid area.
At diagnosis, approximately two thirds of tumors are confined to the cords, usually one cord. The anterior portion of the cord is the most common site.
Subglottic extension may occur by simple mucosal surface growth, but it more commonly occurs by submucosal penetration beneath the conus elasticus. One cm of subglottic extension anteriorly or 4 to 5 mm of extension posteriorly brings the border of the tumor to the upper margin of the cricoid, exceeding the anatomic limits for conventional hemilaryngectomy.
Advanced glottic lesions eventually penetrate through the thyroid cartilage or via the cricothyroid space to enter the neck, where they may invade the thyroid gland.
Because early diagnosis is uncommon, most lesions are bilateral or circumferential at discovery.
Disease spreads mainly to the subdigastric nodes.
The incidence of clinically positive nodes is 55% at the time of diagnosis; 16% are bilateral (11).
Elective neck dissection reveals pathologically positive nodes in 16% of cases. Observation of initially node-negative necks eventually identifies the appearance of positive nodes in 33% of cases (7, 22).
The risk of late-appearing contralateral lymph node metastasis is 37% if the ipsilateral neck is pathologically positive (12).
Fiber-optic illuminated endoscopes (rigid and flexible) are used routinely to complement the laryngeal mirror examination.
A computed tomography (CT) scan should be done before biopsy so that abnormalities that may be caused by the biopsy are not confused with tumor.
CT is preferred to magnetic resonance imaging because the longer scanning time for magnetic resonance imaging results in motion artifact (20).
Archer et al. (3) correlated CT findings with the incidence of cartilage or bone invasion on whole-organ sections. In 12 of 14 patients with pathologic evidence of cartilage invasion, the average diameter of the tumor in two dimensions was more than 16 mm, and the lesion was located below the top of the arytenoid.
The American Joint Committee on Cancer staging system (1) for laryngeal primary cancer is listed in Table 19-1.
Carcinoma in situ sometimes may be controlled by stripping the cord; however, it is difficult to exclude the possibility of microinvasion in these specimens.
TABLE 19-1 American Joint Committee Staging System for Laryngeal Cancer
TX
Primary tumor cannot be assessed
T0
No evidence of primary tumor
Tis
Carcinoma in situ
Supraglottis
T1
Tumor limited to one subsite of supraglottis with normal vocal cord mobility
T2
Tumor invades mucosa of more than one adjacent subsite of supraglottis or glottis or region outside the supraglottis (e.g., mucosa of base of tongue, vallecula, medial wall of pyriform sinus) without fixation of the larynx
T3
Tumor limited to larynx with vocal cord fixation and/or invades any of the following: postcricoid area, pre-epiglottic space, paraglottic space, and/or inner cortex of thyroid cartilage
T4a
Moderately advanced local disease. Tumor invades through the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus)
T4b
Very advanced local disease. Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures
Glottis
T1
Tumor limited to the vocal cord(s) (may involve anterior or posterior commissure) with normal mobility
T1a
Tumor limited to one vocal cord
T1b
Tumor involves both vocal cords
T2
Tumor extends to supraglottis and/or subglottis, and/or with impaired vocal cord mobility
T3
Tumor limited to the larynx with vocal cord fixation and/or invasion of paraglottic space, and/or inner cortex of the thyroid cartilage
T4a
Moderately advanced local disease. Tumor invades through the outer cortex of the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus)
T4b
Very advanced local disease. Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures
Subglottis
T1
Tumor limited to the subglottis
T2
Tumor extends to vocal cord(s) with normal or impaired mobility
T3
Tumor limited to larynx with vocal cord fixation
T4a
Moderately advanced local disease. Tumor invades cricoid or thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscles of the tongue, strap muscles, thyroid, or esophagus)
T4b
Very advanced local disease. Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures
Regional Lymph Nodes (N)
NX
Regional lymph nodes cannot be assessed
N0
No regional lymph node metastasis
N1
Metastasis in a single ipsilateral lymph node, 3 cm or less in greatest dimension
N2
Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension, or in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension, or in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension
N2a
Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension
N2b
Metastasis in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension
N2c

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access