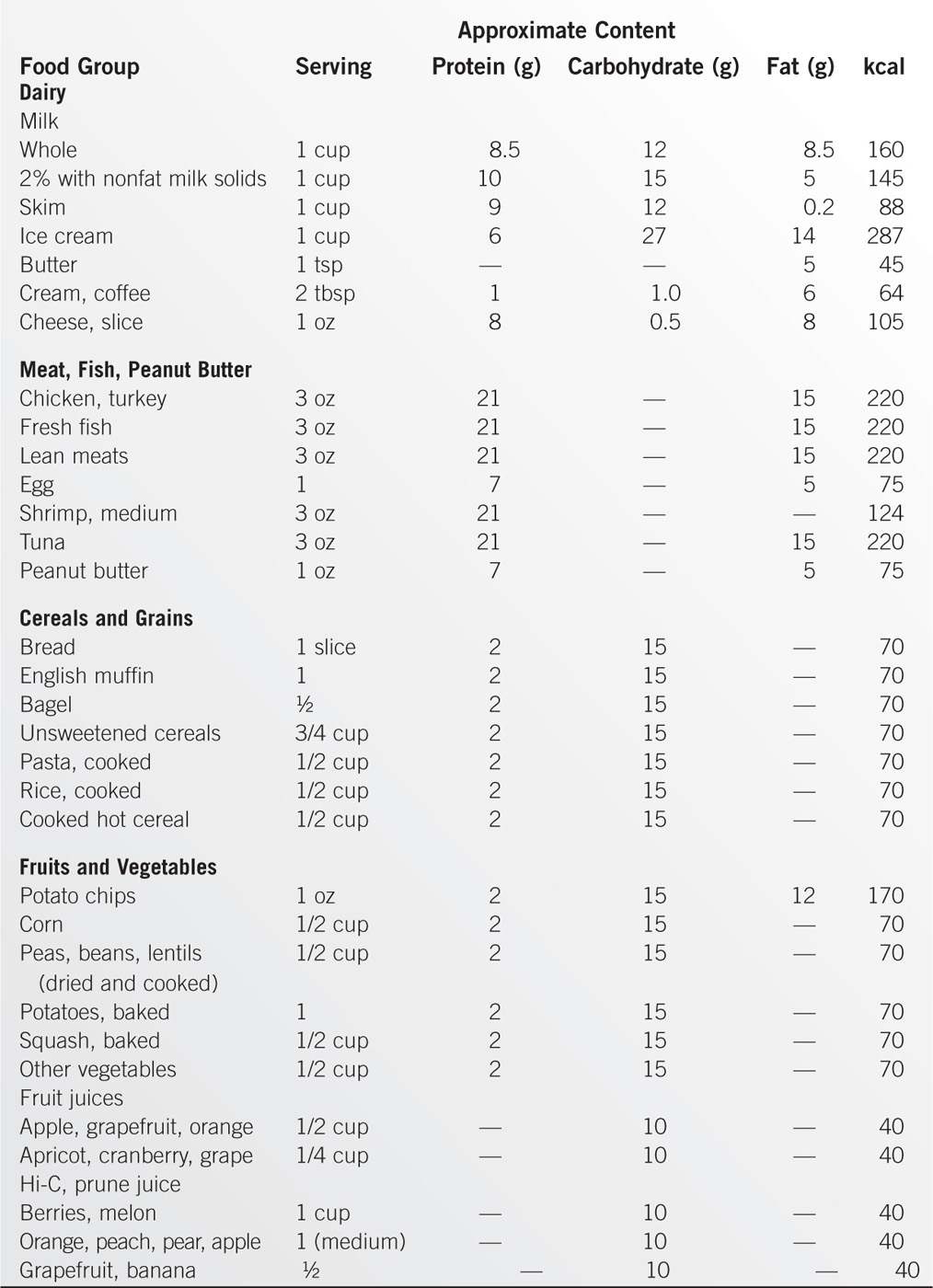
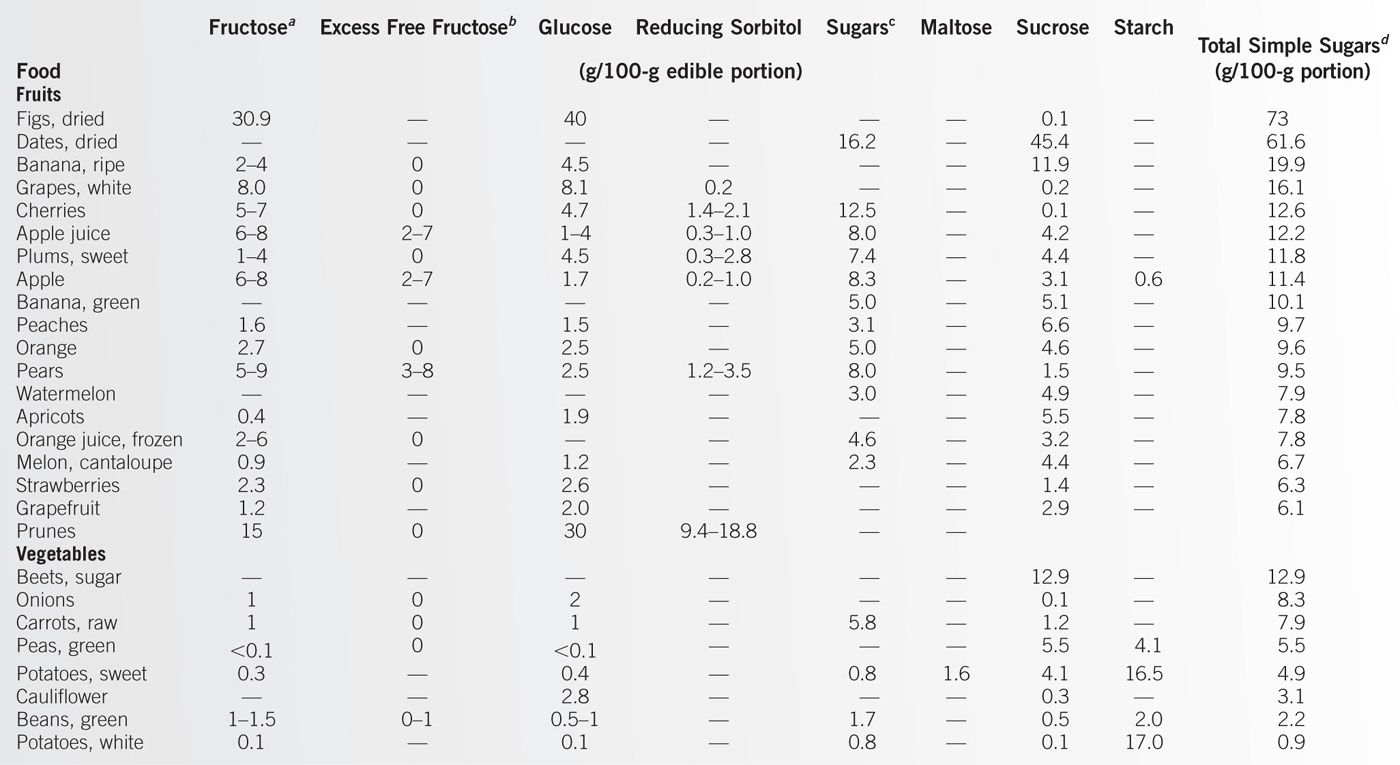
Occasionally, certain foods that are sources of nutrients have special features that must be considered when the foods are used to maintain a balanced diet. For example, avocados provide fiber, folate, potassium, vitamin C, and vitamin B6 in good amounts, but each ounce contains about 50 kcal and 5 g of fat (3). Both of these foods are excellent components of a balanced diet, but the special features of each should be noted. The common macronutrients, vitamins, and minerals contained in foods are listed in Table 12-5, which provides guidelines for maintaining a balanced diet.
US Department of Agriculture Food Guides
Methods for educating consumers about a balanced diet have been devised by the US Department of Agriculture (USDA) since the 1940s (4). The first guide divided foods into seven groups (leafy yellow vegetables, citrus fruits and tomatoes, potatoes and other vegetables, dairy products, meat and nuts, bread and cereals, and butter and margarine), but the recommendations lacked serving sizes. In 1956, the Basic Four Food Guide was introduced (dairy products, vegetables and fruits, meat and nuts, and bread and cereal). This specified amounts from each of these groups, but did not give guidance on calorie intake, fats, or sugars. This guide was expanded in 1979 by adding a fifth group to provide guidance on intake of fats, sweets, and alcohol. The Food Wheel was introduced in 1984 using the five food groups but giving daily amounts of food at three calorie levels. The Food Pyramid guide was launched in 1992 with goals for nutrient adequacy and moderation. Added fats and sugars were visualized throughout the five food groups and at the tip of the pyramid. The pyramid was expanded in 2005 to MyPyramid, including daily amounts of food at 12 calorie levels, and added a band for oils and the concept of physical activity. The latest version is MyPlate, introduced in 2011 at the same time as the 2010 Dietary Guidelines for Americans (DGA). The shape of the icon has been modified to a plate, as the pyramid proved confusing, with the most restricted foods at the top of the pyramid. However, MyPlate continues the personalized approach started with MyPyramid. This brief summary of the USDA Food Guides is meant to underline the continued use of food groups and serving sizes, and the continuous development of the concept for consumer use. In fact, MyPlate and MyPyramid are just different ways of illustrating the same principles.
Dietary Guidelines for Americans 2010
Many guidelines have been developed to provide a diet to minimize the risks for major chronic conditions, such as heart disease, cancer (see Chapter 15), stroke, diabetes, hypertension, dental caries, alcoholism, and obesity. The DGA are evidence-based federal recommendations developed every 5 years, and “designed to prevent and reduce diet-related chronic diseases, while promoting good health and healthy weight among Americans ages two and older” (5). In response to focus groups and the current marketing of foods, the 2010 Dietary Guidelines focused on two concepts: to maintain calorie balance over time that achieves and sustains a healthy weight and to focus on consumption of nutrient-dense foods and beverages. The key recommendations of the 2010 Guidelines are listed in Table 12-6. These recommendations have been used to create the advice presented in MyPlate, so each program reinforces the other. In addition, MyPlate notes the importance of physical activity to accompany any dietary program. MyPlate offers the following tips (3):
• Build a healthy plate.
• Make half your plate fruits and vegetables.
• Switch to skim or 1% milk.
• Make at least half your grains whole.
• Vary your protein food choices, using fish, beans, and lean meats.
• Cut back on foods high in solid fats, added sugars, and salt.
• Choose foods and drinks with little or no added sugars.
• Look out for salt (sodium) in foods you buy.
• Eat fewer foods that are high in solid fats.
• Eat the right amount of calories for you.
• Enjoy your food, but eat less.
• Cook more often at home.
• When eating out, choose lower-calorie menu options.
• Be physically active your way.
• Pick activities that you like and do as much as you can regularly.
• Use food labels to help you make better choices.
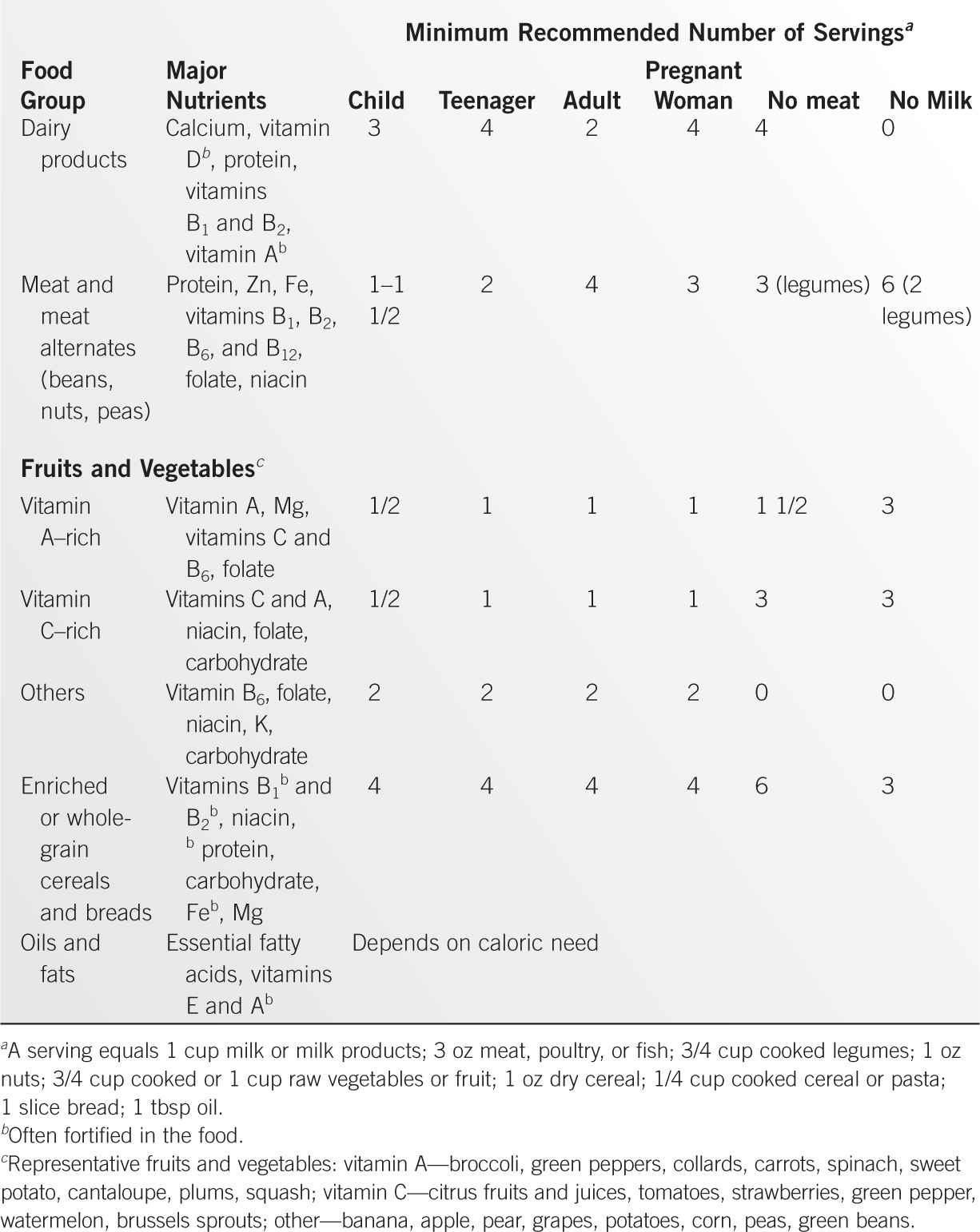
MyPlate offers, as did MyPyramid, a daily food plan that provides specific recommendations at 12 different calorie-intake levels. Table 12-7 presents such a plan for a 2,000-calorie pattern.
Key Recommendations of the Dietary Guidelines for Americans 2010 |
Balancing Calories to Manage Weight | Building Healthy-Eating Patterns |
Prevents and/or reduce overweight through improved eating and physical activity behavior | Select an eating pattern that meets nutrient needs over time |
Control total calorie intake to manage body weight | Account for all foods and beverages consumed |
Increase physical activity and reduce sedentary behavior | Follow food safety recommendations to reduce risk of foodborne illness |
Foods and Food Components to Reduce | Foods and Nutrients to Increase |
Sodium intake to <2.3 gm, and further to 1.5 gm for persons >51 years old and with high BP, diabetes, or chronic renal disease | Vegetable and fruit intake |
<10% of calories from saturated fat | Dark-green, red, and orange vegetables |
<300 mg of dietary cholesterol | >Half of all grains as whole grains |
Limit trans fatty acids (e.g., hydrogenated oils) | Fat-free or low-fat milk and milk products |
Reduce intake of solid fats and added sugars | Seafood, lean meat and poultry, eggs, beans and peas, soy products, nuts, and seeds as protein sources |
Limit refined grain foods, esp. with added sugar | Use oils to replace solid fats when possible |
Alcohol in moderation (1 drink/d for women, 2 for men) | Foods that provide potassium, dietary fiber, calcium, and vitamin D |
Modified from Development of 2010 Dietary Guidelines for Americans. http://www.health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf.
The DGA aims to reduce diet-related chronic diseases. Vegetarian diets achieve many of these objectives because they reduce the risks for hypertension, coronary artery disease, diabetes (type 2), and gallstones (6,7). Diets designed to prevent cancer or heart disease are based on similar recommendations (see also Chapter 15). The dietary recommendations outlined above and discussed in Chapters 2 and 3 are intended for general populations in the United States. However, some special considerations should be emphasized for African Americans and other minority groups. The diets of middle-aged African Americans may be lower in calcium, magnesium, iron (for women), folacin, and zinc. Obesity is more prevalent in African American women than in White women, and it may be more difficult for them to achieve a desirable weight. Hispanic-Americans tend to consume a diet higher in fiber and with less animal fat. Overweight has been a greater problem in Hispanic-Americans than in Anglo-Americans. The diet of Asian/Pacific-Americans is generally higher in fish, shellfish, and fruits and vegetables but lower in dairy products and calcium. As these populations become more assimilated into Anglo-American societies, group differences may diminish.
Daily Food Plan on a 2,000-Calorie Pattern |
Food Group | Amount | Comments |
Grains | 6 oz | Aim for at least 3 oz of whole grains |
Vegetables | 2.5 cups | Vary types, aim for each week: dark-green veggies 1.5 cups, red/orange veggies 5.5 cups, beans/peas 1.5 cups, starchy veggies 5 cups, other veggies 4 cups |
Fruits | 2 cups | Eat a variety of fruit, whole or cut-up rather than juices |
Dairy | 3 cups | Low-fat (1%) or fat-free milk, yogurt, and cheese |
Protein foods | 5.5 oz | Use seafood 2x/week; vary protein to choose beans, peas, nuts, and seeds more; keep meat/poultry portions small and lean |
Fats, sugars, salt | Limit | Oils to 6 tsp/d, calories from solid fats and added sugars to 260 kcal/d, sodium to <2300 mg/d |
Physical activity | 150 min/wk |
|
Adapted from www.chooseMyPlate.gov.
The American Heart Association has issued its comments on the DGA 2010, which largely confirm its own 2006 Guidelines, designed to reduce the risk of cardiovascular disease (CVD) (8). These recommendations are very similar to their 2006 document, and to all other evidence-based healthy diets. Recommendations include the suggestions to
• Achieve and maintain a healthy body weight (body mass index [BMI] 18.5 to 24.9).
• Consume a diet rich in vegetables and fruits (especially those that are deeply colored).
• Select whole-grain, high-fiber foods (half of grain intake should be whole grain).
• Consume fish at least twice a week (especially oily fish rich in ω-3 fatty acids).
• Limit intake of saturated fat to less than 7% of calories, trans fat to less than 1% of calories, and cholesterol to less than 300 mg per day by selecting lean meats, skim and low-fat dairy products, and minimizing intake of partially hydrogenated fats by substituting solid margarines with liquid vegetable oils.
• Minimize intake of beverages and foods with added sugars (especially sucrose and corn syrup).
• Choose and prepare foods with little or no salt (limit to 2.3 g of sodium per day).
• Consume alcohol in moderation (less than two drinks per day for men, one drink per day for women).
Other Important Factors in Maintaining a Healthy Diet
Practical Advice
Food should be consumed as three daily meals. This practice avoids periods of great hunger with subsequent overeating and provides energy for tasks to be performed throughout the day. Snacks can certainly be a part of the diet and can include foods from any of the major groups. Junk or fast foods also can be included in a balanced diet. It is only when most of the daily calories are derived from these foods that they pose a problem. Fast foods often contain many calories in the form of fat and carbohydrates, with lesser amounts of protein. Moreover, they usually do not include fruits and vegetables and so do not provide all the micronutrients needed. The term empty calories, which has been used to describe the nutritive value of these foods, is a poor one. The caloric value of fast foods is as real as that of any other foods because all calories are equal. The foods lack many of the other nutrients, but the caloric value is the same.
The best way to entice a patient to follow a balanced diet is to review food lists, identify the perceived problems in the intake of all foods, and provide specific recommendations for foods in each major group. In addition, the health-care provider must discover what behavioral patterns accompany the abnormal or irregular intake of food if an attempt to correct the diet is to be made.
The average hospital house diet is balanced as far as nutrients are concerned, although the palatability is not always good because the flavors are usually quite bland. The hospital diet provides each day between 2,000 and 2,500 kcal, 60 to 80 g of protein, 2.5 to 3.5 g of sodium, 3.5 to 4.5 g of potassium, 1.0 to 1.3 g of calcium, 1.1 to 1.5 g of phosphorus, 300 to 400 mg of magnesium, 7 to 9 mg of iron, and 13 to 14 mg of zinc. However, many teaching hospitals do not design house diets to meet nationally recognized dietary recommendations (9). Moreover, they do not always provide enough information for the patients to select appropriate and healthful choices.
Alcohol
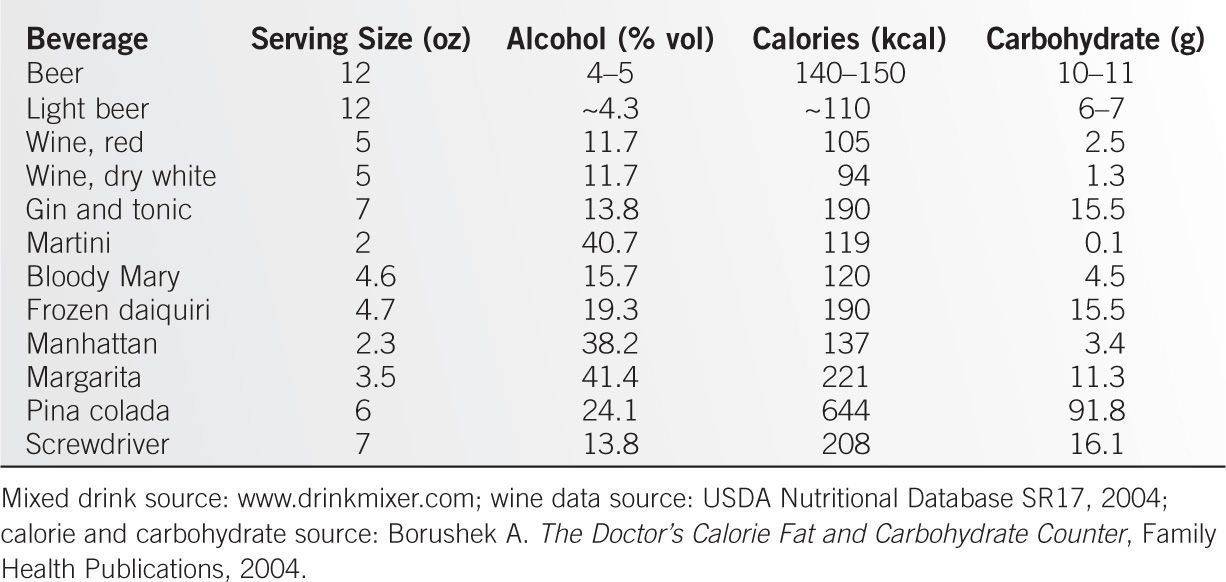
Alcohol is a component of many diets, and the carbohydrate and caloric load should be appreciated, as these can be considerable (Table 12-8).
Taste and Smell
One major factor in maintaining an adequate oral intake is the presence of normal taste and smell. It is now clear that the gustatory system, unlike other sensory systems, is comprised of many (~50) different receptors concentrated in only a few cell types, providing clues to perceive thousands of different taste sensations by a combination of receptor activation (10). Thus, sensing sweet, salt, bitter, and amino acids is probably coordinated within the brain. Moreover, genetic variations in bitter taste perception can cause great variability in the acceptance and use of certain foods, particularly vegetables (11). Central representation of taste discrimination may be the reason why people lose smell and taste acuity as they age, and this change is associated with poorer appetite and food intake (12). In addition, many elderly people are unaware of this impairment in smelling acuity. The basal forebrain cholinergic system sends projections to the olfactory bulb and to other brain regions involved in the perception of memory and cognition (13). Thus, it is not surprising that olfactory loss also occurs early in Alzheimer and Parkinson diseases and other degenerative brain disorders. Other important causes of altered taste and smell include depression, the postmenopausal state, and many medications, particularly halide salts that are concentrated in salivary secretions.
Sweet-tasting products also can produce satiety, and may be important in the reward mechanism in response to food (14). While taste receptors in the mouth may mediate much of this feedback, it is clear that luminal contents in the intestine are recognized by specialized enteroendocrine cells in the intestinal epithelium that can act on nerve endings to transmit signals (15). Molecular signals are best described for sugars (transporters and G protein–coupled receptors), but fatty acid receptors and transporters (including CD36) have been implicated in nutrient sensing, as have peptide and amino acid G protein–coupled receptors.
“Health-promoting” Diets Other Than DGA 2010
Vegetarian Diets
The vegetarian diets include strict vegan (without milk or eggs), lacto–vegetarian, ovo–vegetarian, and lacto–ovo–vegetarian. The strict vegan diet compared with an omnivore diet contains lower fat, less saturated fat, a high polyunsaturated/saturated fat ratio, no cholesterol, about 50% to 100% more fiber, and somewhat less protein (6). A lacto–ovo–vegetarian diet contains intermediate ranges of these components. The more milk and cheese is ingested, the higher the animal fat and cholesterol content. But all vegetarian diets contain more plant foods, bringing with them higher intake of fiber, folate, antioxidants, and phytochemicals. These components are thought to account for many of the lower risks that have been observed for developing cancer (especially colon and lung), obesity, heart disease, type 2 diabetes, hypertension, constipation, and gallstones (7). The risks of vegetarian diets are mostly seen with strict vegan diets, and include osteopenia from low calcium intake, vitamin B12 deficiency, and impaired growth from low energy intake. Vegetarian diets are now considered to offer more health benefits than risks (16). However, the value of a vegetarian diet may not be universal in all cultures. A review of eight Asian nation cohort studies in Bangladesh, China, Japan, Korea, and Taiwan did not show a higher rate of mortality for total meat intake (17). In fact, meat intake was inversely associated with CVD mortality among men in these Asian countries.
Vegetarian diets are also good sources of most vitamins and minerals, but not vitamin B12 or iron. Plant foods that contain as much calcium as one cup of cow’s milk include 1 cup of calcium-fortified juice or soy milk, or calcium-set tofu (18). Natural sources (e.g., 2 cups of broccoli or kale) may contain as much calcium, but the bioavailability will not equal that of milk. Vegetarian diets can also provide vitamin D3, either from fortified plant milk (40 to 120 IU per cup) or from commercial mushrooms (~380 IU per cup) (18).
Nitrates and Nitrites
Another concern about diets that contain a large amount of fruits and vegetables (vegetarian, DASH [dietary approaches to stop hypertension], Mediterranean, Nordic, etc.) is that these foods contain about 80% of dietary nitrates, and these diets probably exceed the World Health Organization’s (WHO) Acceptable Daily Intake for nitrate by five- to sixfold (19). Nitrates are present in up to 50 mg per L in drinking water, the permissible concentration recommended by the WHO. Estimated average nitrate intakes from food are 31 to 185 mg per day in Europe and approximately 40 to 100 mg per day in the United States of America, with a bioavailability of 100% (19). Nitrite content of foods is approximately 10% or less that for nitrates. The WHO Acceptable Daily Intake for nitrate ions is 3.7 mg per kg body weight, and for nitrites 0.06 mg per kg (20). The Environmental Protection Agency recommendations are approximately 7.0 mg per kg of nitrate. Exogenous nitrate is converted to nitrite on the tongue by bacterial nitrate reductases, and in the tissues by mammalian reductases. Nitrite ions are converted to nitric oxide (NO), which has beneficial effects on blood pressure and blood vessels (15,21). Endogenous NO is produced from L-arginine.
Vegetable sources rich in nitrate include broccoli, carrots, cauliflower, and cucumber (20 to 50 mg per 100 g fresh weight), cabbage, turnip (50 to 100 mg per 100 g), celeriac, Chinese cabbage, endive, fennel, kohlrabi, leek, parsley (100 to 250 mg per 100 g), and celery, cress, lettuce, red beetroot, spinach, and arugula (>250 mg per 100 g) (22). Current regulatory limits for exogenous intake of nitrates are easily exceeded by normal daily intakes of individual foods, especially spinach and soya milk. There are data suggesting that dietary nitrate and/or nitrite might improve cardiovascular (CV) health (e.g., by lowering blood pressure), but the current regulatory limits are based on concerns of carcinogenicity and methemoglobinemia, generated by data largely from animal experiments. Although in vitro and animal data suggest that nitrates are converted to carcinogenic N-nitrosamines, there are few data in humans that nitrates are carcinogenic (19). This view is supported by the review by the WHO Committee on Food Additives (23), and epidemiological studies suggesting that abundant intake of vegetables decreases the risk for cancer. Current data are not sufficient to generate an accurate benefit/risk assessment for nitrate intake, in part because of the lack of inclusion of nitrate/nitrite concentrations in standard food databases.
Mediterranean Diet
The Mediterranean diet reinforces the plant-based core of the dietary pattern of MyPlate, but also emphasizes cultural and lifestyle activities, including conviviality, culinary activities, physical activity, and adequate rest (24). The key components of the diet itself include eating largely plant-based foods (fruits, vegetables, whole grains, legumes, and nuts), replacing butter with olive or canola oil, using herbs and spices for seasoning instead of salt, limiting red meat to only a few times a month, eating fish and poultry at least twice a week, and drinking red wine in moderation. The health benefits of this diet have included lower overall mortality, lower CVD and cancer incidence or mortality, and lower risk for neurodegenerative disease (25). This diet has been well accepted in Southern Europe, where it fits the needs and lifestyle of that cultural region.
Nordic Diet
The Nordic diet was developed as a regional diet stressing locally available foods, as the Mediterranean diet was not easily reproduced in Northern Europe. This diet emphasizes the use of native berries, cabbage and related cruciferous vegetables, native fish and other seafood, wild and pasture-fed animals (e.g., moose, deer, reindeer, hare, goose, duck, grouse), rapeseed/canola oil as the source of monounsaturated fat, and oat/barley/rye grains in preference to wheat (26). Such a diet has been shown to lower mortality and to improve insulin resistance (27). The importance of the Nordic diet has been the emphasis on diets and food that can be delivered regionally. Part of this delivery system has been the concept of “shop centers” at which families receive dietary instruction and collect most of their foods (28). While purchasing of foods has been high at these centers during study trials, it needs to be confirmed that the concept could be expanded on a larger scale.
DIETS OF ALTERED CONSISTENCY
Clear Liquid Diet
A clear liquid diet consists of liquids that can be seen through (e.g., water, broth, plain gelatin) that are easily digested and leave no undigested residue. It is often used before tests, procedures (e.g., colonoscopy), or surgeries. A clear liquid diet meets the daily requirement for water but minimally stimulates the gastrointestinal tract. This effect is achieved at the cost of minimal ingestion of protein and fat—macronutrients that are potent stimuli of gastric and pancreatic secretions and gastrointestinal motility. In addition, the diet is low in fiber. Because few unabsorbed components are provided, fecal weight and bacterial mass are decreased.
A clear liquid diet is used in the following cases: to treat dehydration resulting from excessive diarrhea or vomiting (if the vomiting has ceased), in mild or moderate pancreatitis as a prelude to introducing full feeding, to decrease output from enterocutaneous fistulae, to manage diarrhea resulting from inflammatory bowel disease (IBD), to maintain nutrient intake during chemotherapy or radiation therapy for cancer, and to prepare a patient for bowel surgery or for colonoscopic examination (29). In the surgical setting, a clear liquid diet is useful in the recovery phase of abdominal or other surgery when partial ileus is present. This restriction may not be applicable to patients after gastrointestinal surgery once bowel sounds have been heard. Early refeeding by tube or per os of either liquid or solid food has been used successfully after gastrointestinal surgery and may be beneficial for reducing hospital stay and complications (30). There seems to be no clear advantage to withholding feeding from patients following lower-bowel surgery, and perhaps even after upper-abdominal surgery. A clear liquid diet may be useful preoperatively as well, as some data suggest that preoperative fasting has adverse consequences for the patient, especially insulin resistance (31). No studies are available demonstrating an effect of preoperative fasting on differences in morbidity and mortality.
The identification of foods that are easily digested may be more culturally than scientifically derived (32). Thus, the use of limited diets, such as clear liquid, has persisted for a long time. Following gastrointestinal or gynecological surgery, the small bowel recovers normal motility first (6 to12 h), followed by the stomach (12 to 24 h) and colon (48 to 72 h). Thus, early feeding (fluids or food within the first 24 h postoperatively) has been shown to be safe and to shorten hospital stay, although such a schedule is limited in some patients by nausea (33). While the timing of feeding has been studied, the initial choice of diet has been much less studied. Clear liquids are usually offered, but a regular or soft bland diet has been equally well tolerated (34). The Enhanced Recovery After Surgery (ERAS) Group recommendations suggest solids allowed up to 6 hours before colorectal surgery, and early feeding and oral supplements from the day of surgery until “normal” food intake is achieved (35). Thus, the time-honored progression from clear liquid to full liquid to soft solid no longer seems necessary for most patients with colorectal or gynecological surgery (or with other nonabdominal surgeries). The same thinking applies to mild acute pancreatitis, for which nonliquid soft or solid diets are as well tolerated as liquid ones, and lead to earlier discharge from hospital (36).
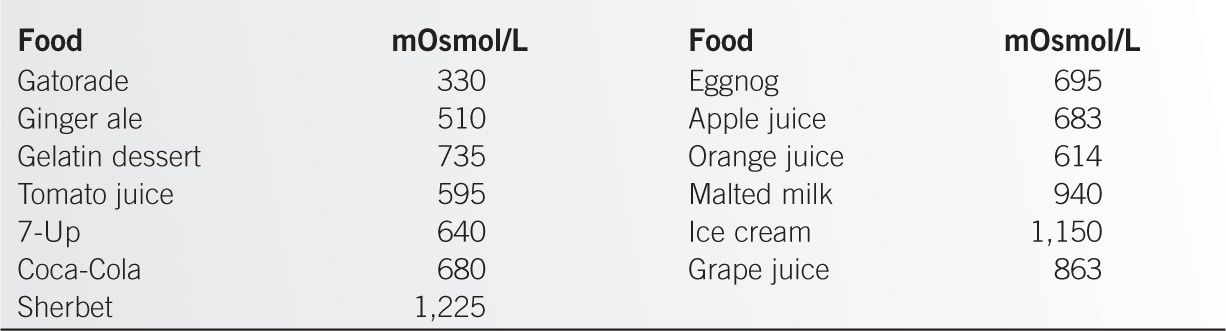
Increased intake of calorie-containing beverages (150 to 300 kcal per day) has been associated with an increase in weight in the United States. A Beverage Guidance Panel was organized and has issued a report (37). This panel concluded that drinking water should be the preferred beverage to fulfill daily water needs, followed by tea and coffee, low-fat and skim milk, noncalorically sweetened beverages, beverages with some nutrients (juices, whole milk, alcohol, and sport drinks), and least of all calorically sweetened but otherwise nutrient-poor beverages. Beverages sweetened with sugar or high-fructose corn syrup (HFCS) pose a risk for fatty liver (fructose increases hepatic lipogenesis), obesity (as intake of beverages does not replace other calories), and hypertriglyceridemia (due to fructose) (38). The clear liquid diet designed for medical purposes needs to use caloric beverages, but it is worth remembering that in other circumstances, it is better to drink calorie-poor beverages, mainly water.
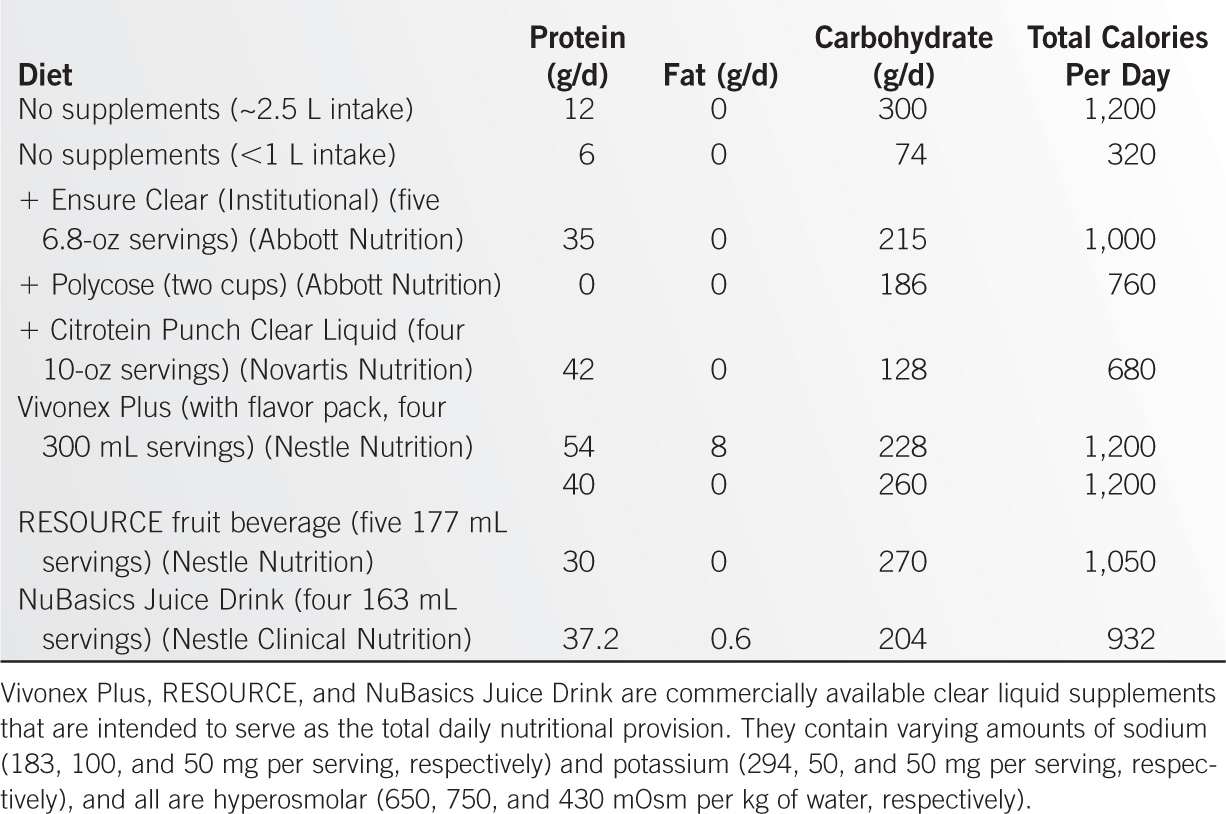
The clear liquid diet is largely water and sugar and provides few other nutrients unless supplements are added. Without supplements, the diet provides about 1,200 kcal per day (300 g of carbohydrates) along with 1.0 g of sodium, 50 to 60 mg of calcium and magnesium, 2,000 to 2,500 mg of potassium, less than 100 mg of phosphorus, 1.2 mg of iron, and only 0.33 mg of zinc. To obtain even this supply of nutrients, one must ingest about 1,500 mL of strained fruit juice, 600 mL of gelatin or fruit ice, and 30 g of sugar added to coffee or tea. Intake of these volumes can be achieved by healthy or younger patients. The diet of an elderly or ill patient may be even more restricted because intake is smaller.
Multiple vitamin and iron supplementation is suggested if the patient is to be on the diet for more than 3 weeks, or sooner if deficiency is present when the diet is initiated. If the diet is to be continued beyond 3 days or if fluid intake is limited, it can be supplemented with carbohydrate and a small amount of protein in addition to some micronutrients. Table 12-9 lists these modifications. The supplemented clear liquid diet provides about half the daily adult protein allowance, and it meets or exceeds allowances for vitamins E and C, folic acid, thiamine, riboflavin, niacin, vitamins B6 and B12, and iron. Vitamin A, calcium, and phosphorus are provided at about 60% of the daily allowance. Carbonated beverages can be substituted for Polycose™ as a source of carbohydrate, but they have many fewer calories. The use of supplements depends on the acceptability of fruit juices and gelatins as the major caloric source for the patient. Foods allowed include coffee, tea, carbonated beverages, broth, bouillon, strained fruit juices, gelatin, sugar, and sugar candies. Side effects do not develop if supplements are provided. Calories, protein, vitamins, and minerals are needed in the usual circumstances during long-term use.
Caffeine
It is generally agreed that the caffeine content of various beverages alters certain aspects of gastrointestinal function (e.g., transit time is shortened), and causes (unwanted) alertness and a jittery feeling. For this reason, the inclusion of caffeinated beverages may not be desirable in other diets. However, these drinks are usually included in a clear liquid diet. Table 12-10 lists the caffeine content of some foods and drugs.
Caffeine Content of Foods and Drugs |
Food | Unit | Caffeine Contenta (mg/unit) |
Prepared Coffee | 6-oz cup |
|
Instant, freeze-dried |
| 61–72 |
Percolated |
| 97–125 |
Drip |
| 137–174 |
Starbuck’s Coffee Grandeb Dunkin Donuts Coffee with Turbo Shotc | 16-oz cup 20-oz cup | 330 436 |
Decaffeinated Coffee | 6-oz cup |
|
Ground |
| 2–4 |
Instant |
| 0.5–1.5 |
Tea, Bagged or Loose | 6-oz cup | 15–75 |
Black, 5-min brew |
| 40–60 |
Green, Japan, 5-min brew |
| 20 |
Iced Starbuck’s Teas | 12-oz cup 16-oz cup | 67–76 80–135 |
Cocoa Beverages | 6-oz cup | 10–17 |
Chocolate |
|
|
Chocolate milk | 8 oz | 2–7 |
Milk chocolate | 1 oz | 1–15 |
Semi-sweet | 1 oz | 5–35 |
Baker’s | 1 oz | 26 |
Syrup | 1 oz | 4 |
Bar | One | 60–70 |
Carbonated Drinks | 12-oz can |
|
Colasc Mountain Dew |
| 45–55 54 |
Diet colas |
| 35-47 |
Root beer, citrus |
| 0 |
Ginger ale, tonic, other nondiet |
| 0–22 |
Drugs | Tablet |
|
Cold tablets |
| 30–32 |
Alertness tablets |
| 100–200 |
Weight control tablets |
| 140–200 |
Pain relief OTC |
| 32–65 |
Prescription pain tablets |
| 30–100 |
Sport/Energy Drinksc |
|
|
AMP energy | 8.5 oz | 75 |
AMP Energy Boost Original | 16 oz | 142 |
Five Hour Energy | 1.9 oz | 208 |
Full Throttle | 16 oz | 200 |
Monster Energy | 16 oz | 180 |
Red Bull | 8.5 oz | 80 |
SoBe No Fear | 16 oz | 174 |
V8 V-Fusion + Energy | 8 oz | 80 |
aThe ranges represent the range of figures from the literature because the method of preparation affects caffeine content of some beverages.
bData from Mayo Clinic Diet Manual (www.mayoclinic.com/health/caffeine); Adapted from Nagy M. Caffeine content of beverages and chocolate. JAMA. 1974;29:337; Bunker ML, McWilliams M. Caffeine content of common beverages. J Am Diet Assoc. 1979;74:28.
cData from Center for Science in the Public Interest. http://www.cspinet.org/new/cafchart.htm, updated Dec 2012.
The caffeine content of beverages depends on the amount of water used, method of brewing, and type of coffee or tea. Because caffeine is water-soluble, the longer the exposure to hot water, the greater the extraction of caffeine. Coffee is a complex mixture of chemicals and provides more than caffeine alone, including those with biological effects, such as phenolic compounds, magnesium, and quinides that can alter insulin sensitivity. Many of these compounds are not found in the coffee bean itself, but result from coffee metabolism in the small intestine and colon (39). Unfiltered coffee contains the diterpenes cafestol and kahweol that have been implicated in elevating cholesterol (40).
Low doses (<50 mg per day) probably have little effect on gastrointestinal function. The actual caffeine content of cocoa is not certain because of the wide variation in reported figures and the fact that most hospitals and homes now use instant cocoa mix, a prepared product. Theobromine, not caffeine, is the major methylxanthine stimulant in cocoa (~250 mg per cup) and chocolate. Caffeine is also a component of some over-the-counter analgesics and of many dietary supplements. These sources should be considered when caffeine intake seems important.
The health consequences of caffeine ingestion are not severe (41). For those patients with hypertension or hyperhomocysteinuria, or for groups that might be more vulnerable to the effects of caffeine (elderly, children, adolescents), limiting intake may be helpful. A subset of patients with restless leg syndrome may have attacks triggered by caffeine (42). No consistent epidemiologic evidence has been found of an effect on birth-related outcomes, including low birth weight, prematurity, spontaneous abortion, and congenital anomalies. However, many studies have not been controlled for smoking, alcohol, or medication. In one case-control study, more spontaneous abortions occurred in nonsmoking women who ingested more than 100 mg of caffeine a day when the fetus had a normal karyotype (43). The risk was proportional to the dose of caffeine ingested. Moreover, high caffeine intake is associated with the risk for late miscarriages, stillbirths, and infants who are small for their gestational age (44). One might cautiously allow reduced caffeine intake during early pregnancy, limiting coffee consumption to 3 cups per day (40). The hypercalciuric effect of 300 mg of caffeine has been well established in women with a diet low in calcium (<600 mg per day), but the mechanism is not clear. However, no effects have been noted on bone health, and caffeine is not considered an important risk factor for osteoporosis, except possibly when used on a long-term basis by persons with a dietary calcium deficiency. The pharmacologic effects on the CV, renal, respiratory, gastrointestinal, and central nervous systems have been studied extensively (41). Consumption of up to 500 mg of caffeine does not cause arrhythmias, but some patients may be especially sensitive to caffeine and should limit their intake. Although data have been reported on both sides of the issue, it does not appear that caffeine causes hypertension or coronary artery disease, nor are the data convincing that caffeine causes hyperlipidemia or fibrocystic breast disease, nor does it appear to increase the risk of chronic disease (45).
Studies are limited on coffee ingestion in relationship to all-cause mortality. Several studies have shown a positive association between higher levels of coffee consumption and CV mortality (46), but other studies have shown an inverse association, and other studies have suggested a U-shaped or J-shaped relationship between coffee ingestion and health outcomes (46). A large US-based study (Aerobics Center Longitudinal Study) confirmed a positive association between high coffee consumption (>4 cups per day) and all-cause mortality in men and women under 55 years of age (46). Although the NIH-AARP study found that coffee consumption was inversely associated with total and cause-specific mortality, there are many confounding issues and alternative explanations for the results arising from this large database that also apply to other large databases (47). Thus, the role of coffee ingestion in any effect on life span is still uncertain.
Because coffee contains many more chemicals than caffeine, studies of coffee intake have shown some interesting differences from that of caffeine alone. Coffee ingestion is associated with a lower risk of type 2 diabetes, but prospective studies are needed to confirm the relationship (48). In fact, irrespective of the caffeine content, sugar-sweetened beverages are associated with a higher risk for type 2 diabetes mellitus (T2DM), while coffee intake (not necessarily caffeine) was again associated with a lower risk (49). Coffee intake does not seem to increase the risk of heart disease or cancer, and 3 to 4 cups per day (300 to 400 mg caffeine) appear not to carry any long-term health risk (40). Although no increased risk of colon and rectal cancer was seen with ingestion of caffeinated coffee or tea, ingestion of more than 2 cups of decaffeinated coffee was associated with a decreased risk of rectal cancer (50). Tea ingestion may improve endothelium-dependent vasodilation. A meta-analysis of prospective cohort studies concluded that an increase in tea consumption of 24 oz per day was associated with a 11% decrease in myocardial infarction (51). But the results of subsequent studies have been inconsistent, and firm conclusions cannot be made (37).
Yet another association has been made regarding the benefits of coffee ingestion, which is on the risk of hepatocellular cancer. A meta-analysis of 16 studies showed a relative risk reduction of approximately one-third in both case-control and cohort studies, and over 50% reduction for high consumption (3 cups or more per day), regardless of a history of alcohol or liver disease (52). Although coffee contains multiple bioreactive compounds other than caffeine (e.g., phenols, diterpenes), decaffeinated coffee does not seem to be protective. However, as with other associations, prospective studies are needed to show causation.
Although habituation to caffeine is common, it is not considered a drug of abuse, and it does not fulfill the Diagnostic and Statistical Manual-IV criteria for psychoactive substance dependence. Headache is a frequent withdrawal symptom. However, “energy drinks” are taken by persons with higher levels of risk-taking. It is possible that the neuropharmacologic effects of caffeine might play a role in enhancing alcohol addiction, although there is no evidence that taking energy drinks with alcohol increases alcohol consumption or increases alcohol dependence (53). Caffeine reverses alcohol-related slower reaction time, but did not alter the impairment of performance caused by alcohol (54). Thus, because no benefit of adding caffeine to alcoholic beverages could be demonstrated, a settlement was reached with two national breweries who agreed to remove caffeine and other stimulants from their products. In November 2011, the Food and Drug Administration (FDA) announced that caffeine is an unsafe food additive to alcoholic beverages, citing that caffeine obscured “some of the sensory cues individuals might normally rely on to determine their level of intoxication” (55). However, “energy drinks” may also pose a risk to health. These drinks contain high levels of caffeine per drink (ranging from 80 to 208 mg), while other drinks contain more than 400 mg of caffeine per serving (Table 12-10). Currently, the FDA sets the maximal allowable caffeine for cola-like drinks at 71 mg per 12-oz serving, but this limit does not apply to energy drinks (56). There are many other components in energy drinks (e.g., taurine, ginseng, glucuronolactone, B vitamins), but there is no evidence that any of these components alter physical or cognitive performance (57).
Full Liquid Diet
The full liquid diet is designed to provide adequate nourishment in a form that requires no chewing. Such a diet can also be useful when the esophagus is narrowed and solid food cannot pass. The full liquid diet (or mechanical soft diet) is indicated for patients who cannot chew properly or who have esophageal or stomach disorders interfering with the normal digestion of solid foods. Liquid supplements (500 kcal) given to patients postoperatively after major abdominal surgery led to improved weight (58). This diet can be used in conjunction with dilation in the management of esophageal stricture. Available methods for dilation include bougienage with mercury-weighted rubber catheters or with metal (olive) dilators.
The diets in which table foods are used can be maintained for long periods only when appropriate supplementation is provided or when all allowed food groups are included. Otherwise, this diet can be nutritionally incomplete. Alternatively, commercially available liquid diets can be used alone (see Chapter 10). However, long-term acceptability is greater when table foods are used as the major source of nutrition.
Full liquid diets can be given through a gastrostomy tube to bypass esophageal obstruction. In such cases, enteral supplements that supply all nutritional needs may be preferred (see Chapter 10) because taste is no longer a factor. Full liquid diets can be helpful temporarily after many types of surgery for debilitated patients who may not have recovered sufficient strength to chew food. Usually, this phase of recovery lasts no more than a few days, except after laryngectomy, when soreness and swelling are present and a new swallowing technique must be learned. In such instances, the use of creamier foods and thicker liquids makes it easier for patients to relearn how to swallow.
Practical Aspects
Certain characteristics of this diet should be kept in mind, especially for successful long-term use:
1. Foods need not be bland.
2. Milk-based foods form an important part of the diet. Lactose intolerance presents a problem when this diet is used, but many milk substitutes are now available, based on either corn syrup or soy.
3. Flavoring is helpful for some milk-based liquids, but natural or vanilla flavor is best tolerated for long-term use.
4. Caloric intake should be maintained near the estimated requirement.
5. Medications should be given in liquid form if possible.
6. Table foods allowed on a full liquid diet include all beverages, broth, bouillon, strained cream soups, poached or scrambled eggs, cereal (e.g., cream of wheat, farina, strained oatmeal), strained fruit juices, ice cream, sherbet, gelatin, custards, puddings, tapioca, yogurt without fruit, margarine, butter, cream, and all spices.
7. The full liquid diet easily provides adequate calories, protein, and essential fatty acids but not certain vitamins, notably ascorbic acid and thiamine, unless fruit juices and cereals are routinely included. The average hospital full liquid diet provides 1,900 to 2,000 kcal per day, along with 40 to 50 g of protein, 3 to 4 g of sodium, 3 to 4 g of potassium, 1.8 g of calcium, 1.3 g of phosphorus, 200 to 300 mg of magnesium, 3 mg of iron, and 8 to 9 mg of zinc.
Side Effects
The diet can be boring, and it is wise to include some items from the mechanical soft diet. If lactose intolerance is present, diarrhea may result, and milk substitutes can be used. If meat soups or brewer’s yeast are not used, the diet will be deficient in folic acid, iron, and vitamin B6.
Supplements Required
No supplements are required if all food groups are used. However, a multiple vitamin and mineral preparation, preferably liquid, is not unreasonable if this diet is to be used for a long time.
Mechanical Soft Diet
The mechanical soft diet is designed to provide a greater variety of foods than the full liquid diet for patients who find it difficult to chew or have an anatomic stricture. Patients with dysphagia may require a liquid or soft solid diet. A history of coughing or choking during meals, prolonged eating time, hoarseness after eating, regurgitation of liquid or food into the nose, frequent drooling, recurrent respiratory infections, and weight loss should lead to an evaluation of oral or pharyngeal swallowing problems. The diet must be planned individually depending on the reason for the restriction. The entire range of solid and liquid foods is used so that the diet is nutritionally balanced. One attempts to provide easily masticated foods. Because texture is an important part of taste, patients must choose the foods that they tolerate best and are most acceptable to them.
A mechanical soft diet is indicated for patients who have difficulty chewing because of advanced age or infirmity, postoperative weakness, or dental problems. It is also indicated for patients with anatomic strictures of the esophagus, especially those caused by carcinoma. For patients with strictures in other parts of the intestinal tract, such as the duodenum in active Crohn disease, only certain restrictions may be necessary because gastric grinding/mixing softens food, and allows only food particles of approximately 5 mm in diameter to enter the duodenum.
Practical Aspects
Spices (except hot peppers) are allowed and are in fact desirable to make food more palatable. Food thickeners, largely gums and modified starches, are available as an aid in swallowing to avoid aspiration. Patients with oral or pharyngeal dysphagia should eat slowly, sit up as straight as possible, keep their head in an optimal position for swallowing (as determined by swallowing studies), and ingest small amounts at any one time.
1. Foods allowed on a mechanical soft diet. All beverages and soups are allowed. Whole tender meat is permissible, as is ground or puréed meat, but not fibrous meat. Eggs and cheese are permissible. Melted cheese or nonfat dry milk can be used to increase protein content. All potatoes and starches are allowed. Breads and cereals are acceptable, except for high-fiber cereals and hard, crusty breads. Cooked or refined ready-to-eat cereals are often better. Vegetables can be included if they are well cooked or puréed, but raw vegetables must be shredded or chopped. Foods that are hard to chew must be chopped, ground, or blended. Canned or fresh fruits without skin or seeds are acceptable, but not other fresh or dried fruits. Nuts are not allowed. Desserts are acceptable if they do not contain nuts.
2. The bland diet is often combined with a mechanical soft diet and has been used for years in the treatment of ulcer disease. However, no evidence has been found of the value of a bland diet that restricts spices or coarse foods.
3. Some dietary maneuvers have been helpful in the past in the management of acid peptic disease, such as the use of small, frequent feedings to minimize acid secretion after a meal and the avoidance of snacks before bedtime to prevent acid stimulation during sleep. Other dietary modifications in peptic disease have included the elimination of alcoholic and caffeine-containing beverages and smoking. However, with the current availability of potent acid-suppressing medications, these restrictions are now usually unnecessary.
4. Certain dietary restrictions also may benefit patients with gastroesophageal reflux disease (GERD). Foods that increase lower esophageal sphincter pressure include tomatoes and tomato juice, citrus fruits, chocolate, peppermint, and very fatty foods. However, the value of restricting fatty foods in the treatment of GERD has been questioned (59).
Side Effects
No side effects have been associated with this diet.
Supplements Required
Supplements are not required.
Modified-fiber Diets
Dietary fiber is not one chemical substance, nor is it completely indigestible. It is a component of the diet that either by itself or through its metabolites produces certain physiologic effects in humans, although the nature and importance of these effects are as yet poorly delineated. Fiber is not the same as residue. The latter term refers to all stool solids that result from the ingestion of any given diet. In addition to fiber, residue includes bacteria, exfoliated cells, and mucus. A full or clear liquid diet is best for minimizing fecal residue. Bacteria comprise the largest component of stool solids on a Western diet (~50%), with fiber comprising only approximately 17% (60). Fiber alters the bacterial environment by providing a diluent of luminal contents, and by adding mass to promote colonic movement, but fiber does not promote a large bacterial mass in healthy subjects (61). However, in patients with short-bowel syndrome (SBS) who deliver more fat and calories to the colon, the amount of bacteria excreted in the stools and their fat content is increased, leading to an underestimate of the digestibility of ingested energy and fat (62).
Definition
The definition of dietary fiber has changed over time, developing by consensus. Trowell in 1972 first defined fiber as the proportion of food that is derived from the cellular walls of plants and is poorly digested by humans. The accepted definition of dietary fiber by the American Association of Cereal Chemists (2000) is “the edible parts of plants or analogous carbohydrates that are resistant to digestion and absorption in the human small intestine with complete or partial fermentation in the large intestine. Dietary fiber includes polysaccharides, oligosaccharides, lignin, and associated plant substances. Dietary fibers promote beneficial physiological effects including laxation, and/or blood cholesterol attenuation, and/or blood glucose attenuation” (63). About the same time as the AACC document was prepared, the Institute of Medicine (IOM) prepared a volume on dietary reference intakes (DRIs) that included fiber, recognizing that nondigestible carbohydrates could be isolated and when added to products might produce a health benefit (64). The IOM definitions are as follows: “Dietary fiber consists of nondigestible carbohydrates and lignin that are intrinsic and intact in plants. Functional fiber consists of isolated, nondigestible carbohydrates that have beneficial physiological effects in humans. Total fiber is the sum of dietary fiber and functional fiber.” The European Commission defined fiber as carbohydrate polymers with three or more monomeric units that are neither digested nor absorbed in the human small intestine (Statement of the Scientific Panel on Dietetic Products, Nutrition, and Allergies, July 6, 2007, at the 17th plenary session, www.efsa.europa.eu/en/efsajournal/pub/1060.htm). This definition included edible carbohydrate polymers occurring naturally in foods and those that have been obtained from food raw materials.
Fiber Content
The fiber content of foods is most commonly based on the rather indirect and imprecise measurement of crude fiber—the residue of food that remains after sequential acid and alkali treatment. The relationship between the measurement (of the residue that escapes digestion) and the physiologic role of the residue is confusing. A proposal for a definition of methods of analysis has been made by the Codex Committee on Nutrition and Foods for Special Dietary Uses. This group has stated that nondigestible material is composed of carbohydrate polymers with a degree of polymerization greater than 3, and that these polymers can be present in food when raw or prepared, or added back as synthetic polymers. This opinion has been confirmed by a consensus reached at the Ninth Vahouny Fiber Symposium, which agreed also on the functions of dietary fiber that is not digested or absorbed in the small intestine as increased stool bulk, decreased transit time, increased colonic fermentation and short-chain fatty acid production, positive modulation of colonic microflora, reduced blood total or LDL cholesterol (LDL-C), reduced postprandial blood glucose or insulin levels, weight loss in adiposity, and increased satiety. All these definitions and inclusions have caused a major issue with regulators and consumers (66). The division of fiber into dietary and functional (i.e., added) fiber has created much of this confusion. Although US labeling does not distinguish dietary from functional fiber, many products called functional fiber are on the market. Canadian regulators have concluded that a synthetic or “novel” fiber, when produced and added back to food, can be included in the total for dietary fiber if it meets the accepted definitions (is not digested and is polymerized enough) and has a proven physiological function (67). However, this is a difficult hurdle, as only a small number of novel fibers have been approved since 1985 (ground bleached oat hulls, soy cotyledon, sugar beet fiber, and psyllium seed husk) (66), and wheat bran soluble fiber, rich in arabinoxylan oligosaccharides (Bran Vita™). For an understanding of the uses of altered-fiber diets, the definition, measurement, metabolism, and possible functions of dietary fiber and functional fibers should be considered.
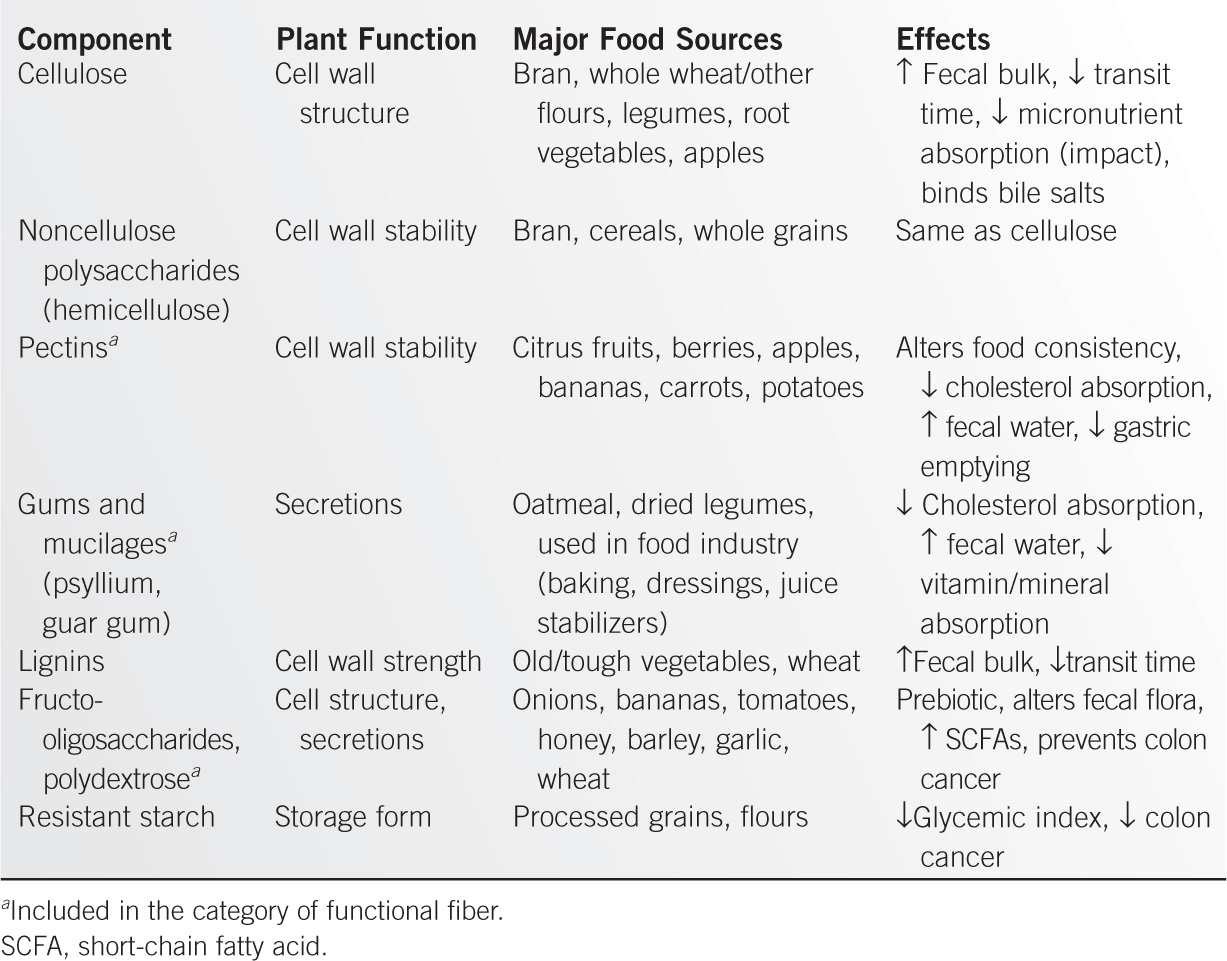
Classes of Fiber
The major chemical classes of dietary and functional fiber are cellulose, noncellulose polysaccharides, and lignin (Table 12-11). These classes can also be arranged based on those that are water insoluble/less fermented (cellulose, hemicellulose, and lignin), and water soluble/well fermented (pectin, gums, and mucilages) (68). All of these classes are all included in the category of nonstarch polysaccharides (NSPs), referring to the naturally occurring cell-wall material in plant foods. Although the NSP content of cereals is high, the ratio of NSP to dry matter (DM) is much greater in fruits and vegetables than in cereals (69). The total fiber content of plants, as exemplified by their content of NSP, is what has been considered the factor leading to health benefits, rather than individual components of NSP. Cereals and grains are rich in arabinoxylans (xylose polymers), cellulose (β-glucans/glucose polymers), and polymers of arabinose, mannose, and galactose. Fruits and vegetables are rich in pectins (uronic acid polymers), cellulose (glucose only), and polymers of rhamnose and fucose in addition to the other polymers found in cereals. The fiber components that are not found in the cell wall (gums, fructo-oligosaccharides, resistant starch) are the major sources of fiber that are added to foods and called “functional” fiber. Because of this label, it is often assumed that they are more beneficial than plant wall–derived fiber, but this is not the case. Most health benefits have been shown to be due to the use of whole plants in the diet, and it is not possible to make independent claims for most of the components of dietary fiber (69).
Cellulose
Cellulose is a straight-chain polymer of glucose with a β-1,4 linkage. It is not digested by pancreatic or small-bowel enzymes. Cellulose is a major structural component of cell walls but rarely accounts for more than 20% of total polysaccharides. It is highly represented in wheat bran, apple and pear skin, and strawberries. Related to celluloses are the β-glucans, composed of straight polymers of β-1,4 glucose and β-1,3 glucose (70).
Hemicelluloses
Hemicelluloses are linear and highly branched polysaccharides of xylose, arabinose, mannose, glucomannans, galactomannans, galactoglucomannans, and glucuronic acid. They act as plasticizers and intertwine with lignin between the cellulose fibers of the cell wall. Nonstructural polysaccharides, including pectins, gums, and mucilages, are branched polymers containing many uronic acids that hold water and form gels. They are highly branched in growing plants and become less branched as the support structure becomes more developed. They act as adhesives and are insoluble in unripe fruit, becoming soluble only as the fruit matures. Thus, the amount extracted may vary with the age of the fruit.
Resistant Short-Chain Carbohydrates
These include those nonglycemic carbohydrates that are soluble in 80% ethanol, other than highly polymerized sugar alcohols. The resistant short-chain carbohydrate (RSCC) fraction includes carbohydrates otherwise referred to as nondigestible oligosaccharides, and includes inulin, fructo-oligosaccharides, polydextrose, methylcellulose, and resistant maltodextrins.
Resistant Starches
Resistant starches are defined as starches that enter the colon. RS1 is physically inaccessible because of its particle size or entrapment in food. RS2 and RS3 resist amylase action because of their compact (unbranched) structure; RS2 is unbranched, and RS3 is retrograded (i.e., altered during processing) (71). Some starches are relatively resistant because they become available slowly in the intestinal lumen. Most resistant starches are produced during food preparation, a process that can either increase or decrease the amount of RS. The food properties that determine whether or not carbohydrate is digestible are determined in vitro by measuring the release of rapidly and slowly available glucose (RAG/SAG); what is left is RS (69). Cereals and bakery products have lower SAG values than do pasta and whole grains. The intake of such starches in a Western diet is estimated at 5 to 10 g per day.
Common Commercial Ingredients High in Dietary Fiber
Acacia gum (gum Arabic) is produced from two species of tree. The gum is a large and complex polysaccharide consisting mainly of arabinogalactans, contributing to soluble fiber. β-Glucan is a component of cell walls from fungi, algae, and grains, although the location of the glucan within the cereal grain varies. This variability leads to large differences in yield when various cereals are processed (72). Chitin and chitosan are β- 1→4 linked insoluble polysaccharides found in arthropods, some fungi, and yeasts. These compounds are the second most abundant (after cellulose) fiber polymer in nature, and are widely produced and consumed in supplements. Algal polysaccharides include alginates, agars, carrageenans, ulvanes, and fucoidans, and are widely used in foods and pharmaceutical products (73). Because these products are largely water soluble, they are easily added to products for thickening and texture, and have been touted as having many health benefits.
Corn bran contains nearly 90% of weight as insoluble fiber, two-third hemicelluloses with some cellulose, is widely available, and has high water-binding capacity (72). Inulin is a soluble fiber composed of a linear chain of fructose molecules that is present in thousands of plants and vegetables. Plants with the highest inulin content include onion, leek, garlic, Jerusalem artichoke, artichoke, and chicory. This fiber is added to provide viscosity and to stabilize emulsions, but is available as a prebiotic as well, promoting the growth of bifidobacteria (72). Oat bran contains from approximately 30% to 90% dietary fiber, much of which is β-glucan. Pectins are linear chains of galaturonic acid with some rhamnose component. Pectin does not contribute much to fecal bulk or transit time.
Polydextrose is a synthetic soluble fiber made from glucose molecules with mainly 1,6 linkages that consequently delivers only approximately 1 kcal per g of energy. It also contains approximately 10% sorbitol and 1% citric acid. Polydextrose is often used as a replacement for sugar, starch, and fat, and as a bulking agent and dietary fiber source in food products, in part because it is stable and very water soluble. It has also been shown to promote the growth of beneficial bacteria, and is used as a prebiotic (72). If a serving contains more than 15 g of polydextrose per serving, the label must contain a statement about laxation. Thus, commercial products tend to limit the content of polydextrose. Like many other dietary fiber components, polydextrose is not specifically identified by usual food analysis for dietary fiber (see below).
Psyllium/ispaghula is the common name used for members of the plant genus Plantago, whose seeds are harvested for production of mucilage. The husk of the seeds provides approximately 70% soluble fiber as a polymer of arabinose, galactose, rhamnose, and galacturonic acid (72). Psyllium increases stool weight and water content, and the number of bowel movements, and is a common component in many commercial fiber products (e.g., Metamucil™, Correctol™, Effersyllium™, Fiberall™, Hydrocil™, Konsyl™, Perdiem™, and Syllact™). Psyllium is also used as a thickener and is used in frozen desserts, as its viscosity property is little affected by changes in temperature.
Rice bran is a by-product of white rice production, containing approximately 20% to 33% insoluble fiber, mostly cellulose and lignin. Thus, it is used mostly in rice flours and breakfast cereals. Soy bran is made from the hull of the bean, and contains 65% to 95% insoluble fiber. Soy fiber contains approximately 75% dietary fiber as a mixture of insoluble and soluble fiber, with much less cellulose than soy bran. Soy bran and fiber are used in multigrain breads, muffins, noodles, breakfast cereals, snack foods, and other baked products (72). Wheat bran contains approximately 45% dietary fiber (cellulose and hemicellulose) with protein and starch making up the rest of the product. Wheat bran is often marketed by itself as a fiber source. Wheat fiber is a further-refined product, almost completely composed of dietary fiber. This product is used for baking because of its high water-holding capacity and storage stability.
Measurement
Four methods for measuring dietary fiber have provided enough data to be useful in assessing the fiber content of foods.
Crude Fiber
Crude fiber is the residue of plant food left after sequential extraction with solvent, dilute acid, and dilute alkali. Early chemists thought that residue-resisting alkali and acid treatment was indigestible. The crude fiber procedure was developed in the 19th century and was favored because of the purity of the residue, which was low in ash and nitrogen content. Extraction and loss of hemicelluloses (>80%) and lignin (50% to 90%) are a consequence of solubility at acid and alkaline pH. All components of dietary fiber are at least partially soluble in these solutions. However, the degree of extraction varies with food preparation, particle size, and presence of other fiber components. Crude fiber is still the measure of fiber reported in some food tables and was the original basis for all altered-fiber diets, but it provides an incomplete and inaccurate assessment of fiber because hemicellulose and lignin are extracted more than cellulose. Crude fiber is slowly being replaced by other methods. The relation of crude fiber to plant cell wall polysaccharide content depends on the proportions of pectins, cellulose, and hemicelluloses, which vary among vegetables and fruits. Monocotyledons in general are high in hemicelluloses and lignin and low in crude fiber. Legumes are higher in lignin but low in hemicelluloses and are intermediate for crude fiber. Dicotyledonous nonlegume vegetables have the highest proportion of cellulose and crude fiber.
Neutral Detergent Residues
These were developed by Van Soest and McQueen (74) and refined further by Englyst et al. (75), and Anderson and Bridges (76). Neutral detergent fiber or residue results from extraction with boiling sodium lauryl sulfate and ethylenediaminetetraacetate (EDTA) and is nonhydrolytic. Pectins and mucilages are removed completely, and the residue contains cellulose, lignin, and hemicelluloses (i.e., the cell wall components of fiber). This residue contains other nonlignin components that are not polysaccharides. Because neutral detergent residue includes all the major plant cell wall components, it continues to be used to assess the dietary fiber content of foods.
The Method of Southgate (77)
This method is the most complex but probably the most accurate because it measures both soluble polysaccharides (mucilages, gums, and pectins) and cell wall components. A series of extractions with organic solvents and acids is followed by enzymatic treatment and hydrolysis. Data derived by this method or a modification of the method are recorded as “total dietary fiber,” which includes noncellulose polysaccharides (hemicelluloses, gums, mucilages, and pectins) and lignins.
Association of Official Analytical Chemists Method
In the Association of Official Analytical Chemists (AOAC) method, enzymes and gravimetry are used. After fat is extracted from food, dried samples are gelatinized and then digested with protease and amyloglucosidase to remove protein and starch. The soluble dietary fiber is precipitated with ethanol, dried, and ashed. Total dietary fiber equals ethanol-precipitated-residue weight minus ashed-residue weight. This is the method now used by the USDA for its tables of food fiber content (see www.usda.gov).
The “correct” assessment of fiber content cannot be made from these data because the physiologic importance of each component is not known. In addition, the preparation of food may alter the measurements by removing soluble and loosely bound components. Thus, fiber supplements should be offered with an understanding of the nonequivalent nature of the product sources.
Fermentation of Fiber
Variations in Degradation
The proportion of cellulose digested in the colon varies widely, from 47% to 80%. Purified cellulose is handled differently from dietary cellulose and is less degraded, about 25% (78). Bran cellulose is less degraded, perhaps because of its high lignin content. Cellulose metabolism is increased by slow transit, as in the elderly. Noncellulose polysaccharides are in general more completely degraded. Wheat bran is among the most poorly digested sources of dietary fiber, for reasons not related solely to its chemical composition. The digestion of NSPs is variable and unpredictable. Most freshly cooked foods and uncooked cereals contain a high percentage of readily digested starch. However, a cooled, cooked potato is less digestible than a freshly cooked one. Thus, it is not true that starch is completely digested and absorbed in the small intestine. Moreover, the fermentation products of starch and NSPs differ in the large intestine. Factors that affect starch digestibility in humans include (besides the physical form) transit time, food processing, and the presence of amylase inhibitors, lectins, or phytates (79). In a Western-type diet, the amount of fermentable carbohydrate entering the colon includes, on average, 12 g of NSPs and a variable amount of starch.
Volatile Fatty Acids
Volatile fatty acids are probably the main product of fiber polysaccharides and are well absorbed by the human colon. Thus, some of the nutritive value of dietary fiber is recovered by the absorption of fermentation products. It has been estimated that from 20 g of dietary fiber, 100 mEq of volatile fatty acids is produced, of which about 20% is excreted and the rest absorbed or used by bacteria.
Fermentation
The overall fermentation process as it is now understood can be defined quantitatively. Fermentation of resultant soluble hexoses is about 60%. Hydrogen produced in large amounts is converted to methane in the ruminating animal. Of humans, only 30% to 40% produce methane, so hydrogen gas is excreted in large amounts. The gas by-products of carbohydrate fermentation are odorless but carry with them the more noticeable by-products of protein breakdown (putrefaction). The volatile fatty acids (acetate, propionate, and butyrate) are available in part as energy sources. Some of the available energy supports bacterial growth. It has been estimated that fermentation of 100 g of carbohydrate supports the growth of 30 g of bacteria. The effect of bacterial growth on other colonic functions has not been determined.
Functions of Dietary Fiber
A high-fiber diet increases stool bulk, produces more frequent stools, and decreases transit time through the intestine. Fecal bile acids appear to be increased when fiber is included in the diet. Table 12-11 reviews the properties of fiber components that may be responsible for the (known and postulated) effects of dietary fiber. However, the intake of fiber must be adequate if the potential benefits are to be realized. Intake in the United States remains lower than the recommended 25 g per day, averaging 17 g per day in the third National Health and Nutrition Examination (NHANES III) (80).
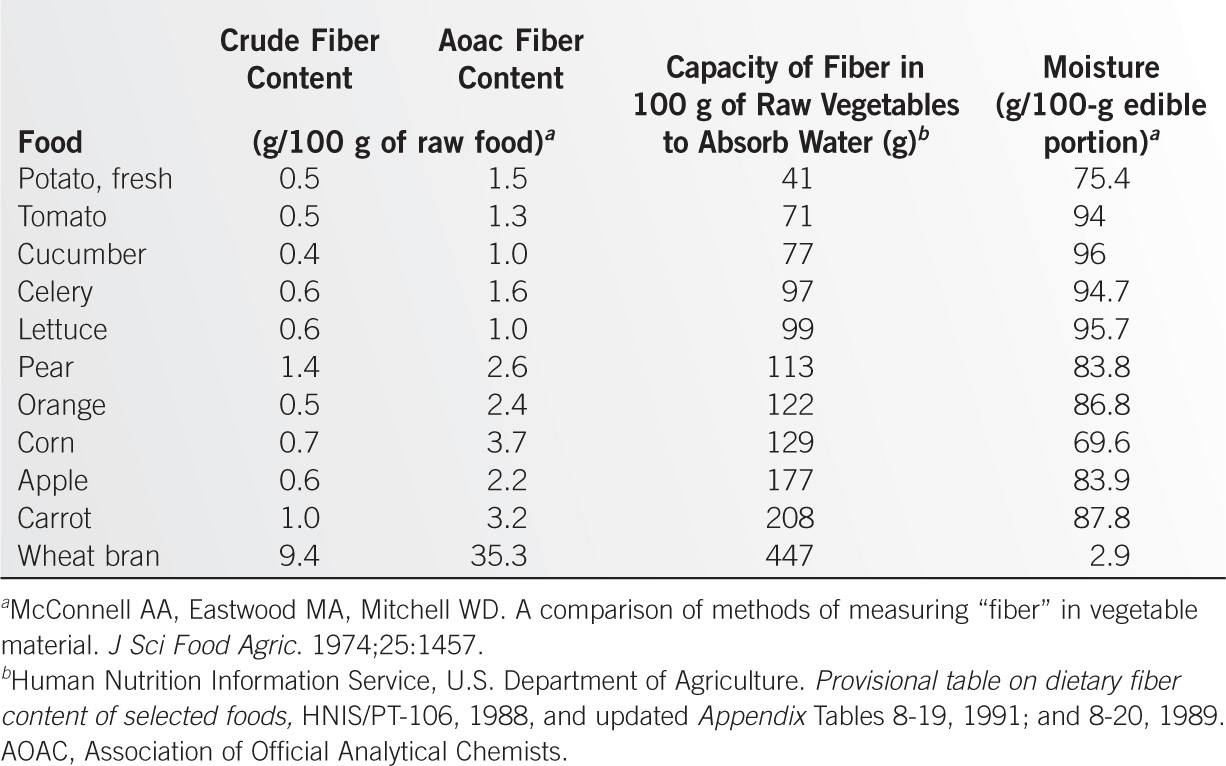
Factors Related to Increased Stool Weight
Even when a function of dietary fiber has been established (water-holding capacity), that function does not necessarily correlate with the crude fiber or total dietary fiber content of foods (Table 12-12). Moreover, the increment in stool weight is not linearly related to either the in vitro water-holding capacity or the water content of the food. It is possible that more than one factor (e.g., volatile fatty acid production in addition to water-holding capacity) is responsible for the observed result—an increase in stool weight. The practical aspect of this information is that not all fiber sources are alike, and the effect of a high-fiber diet may depend on the exact mixture of foods used.
Decreased Intake of Food. Obesity is rare in populations that consume a high-fiber diet, possibly because of a lower caloric intake or increased satiety (81). Dietary fiber intake is lower for obese subjects and BMI is lower in subjects who have higher fiber ingestion (82). Supplementing 14 g per day of fiber is associated with modest weight loss (1.9 kg over 3.8 months), but decreased intake was found mostly in obese subjects (83). The mechanism for this weight loss is unclear but might include satiation, altered glycemic responses, decreased energy absorption, altered gastric emptying, or decreased food intake at a later meal (82). Convincing evidence for most of these mechanisms is lacking. Supplements proposed to work by increasing satiety have shown some effect (glucomannan, guar gum) or no effect (psyllium), but the positive trials showed only modest results in small numbers of subjects (84). Intervention studies show that a very large amount of fiber (~30 g per meal) is needed to decrease energy intake taken after the fiber-containing meal, but this is much beyond what most subjects could tolerate (64). The data are rather better to support a role for dietary fiber in limiting weight gain, especially when compared with high meat intake (85).
Coronary Heart Disease. Coronary heart disease has been inversely related to fiber intake, for example, in the Nurses’ Health Study, in which each increase of total daily dietary fiber of 10 g was associated with a relative risk reduction of 0.81 (86). Of the various sources of dietary fiber, only cereal fiber was strongly associated with a reduced risk for coronary heart disease (relative risk reduction of 0.63 per 5 g daily). Soluble fiber decreases serum total and LDL-C, risk factors for CVD, but there are no epidemiologic studies that link functional fiber (mostly soluble fibers) with the risk of coronary artery disease (64). Moreover, most epidemiological studies link high fiber intake from cereal products with lower rates of CVD. Higher fiber intake, mostly from cereals and vegetables, is associated with lower mortality, particularly from circulatory, digestive, and inflammatory diseases (87). The association was similar for men and women and after correcting for confounding lifestyle and dietary factors.
Diabetes. Fiber ingestion by diabetic patients leads to some delay in gastric emptying, improvement in glucose tolerance, and reduction of hyperinsulinemia and hyperlipidemia (88). The diet used for this study contained 25 g each of soluble and insoluble fiber, and the effect was greater than that seen when the American, British, and Canadian Diabetes Association recommendations were used (8 g of soluble and 16 g of insoluble fiber per day). Total fiber intake may decrease the risk of diabetes and improve postprandial glucose responses, although it may be difficult to separate any positive effect from an improvement in weight (89).
Mineral Availability. Binding by fiber of minerals and trace elements has been shown consistently in vitro, but has not been consistently reported in clinical studies. When a wide variety of food is available and ingested, it is not known whether fiber intake affects mineral availability, and micronutrient supplements are not needed when fiber intake is increased. In fact, oligofructans have been reported to improve calcium absorption and calcium balance in experimental models (90).
Colonic Disorders. The evidence for the inverse association of dietary fiber with diverticular disease, cancer of the colon, and irritable bowel syndrome (IBS) is incomplete, and much of it is based on epidemiologic data (64). In one prospective study, a low intake of fiber (13 g per day) was associated with an increase in the relative risk for the development of symptomatic diverticular disease of 2.35 (91). Some data suggest that a fiber intake of 30 to 35 g per day is inversely related to the risk for colon cancer (see references 92 and 93 for reviews of case-control studies), but the data do not unequivocally support a protective role for fiber. Nine large epidemiological studies examining the relationship between fiber and colorectal cancer (CRC) have been analyzed; four studies showed a statistically significant lower risk for CRC associated with higher fiber intake, but five did not (94). It is possible that the highest levels of fiber intake might show a preventive effect against colon tumors, but the data are not available for very high fiber intakes. Studies have suggested a protective role for fiber against colorectal adenomas (95–97). When other dietary risk factors (smoking, alcohol, folate, red meat, total milk, and total energy) are accounted for in prospective cohort studies, the significance of the association disappeared (98). Because it is difficult to single out one dietary component in relation to cancer prevention (see also Chapter 15), it is not possible to make a recommendation for altering fiber content at this time, except to suggest that the DRI of fiber be followed (Table 12-13).
Although dietary fiber is known to improve the number and bulk of bowel movements in normal subjects, the evidence for its value in IBS is not evident. Some randomized controlled trials (RCTs) show benefit, but most do not (99). It is not clear whether the effect, if and when it occurs, does so in patients with diarrhea compared with constipation or with the mixed bowel pattern, but it is unlikely that fiber is effective against the entire symptom complex (pain, bloating, etc). Any use of fiber in IBS patients should be individualized, especially if a trial of use appears to be helpful.
Lowering Cholesterol Levels. Soluble gel-forming fiber (β-glucans, pectins, guar gum) decreases serum total and LDL-C concentrations and improves insulin resistance (100). The effect may be mediated by cholesterol binding, altered gastric emptying, or both. Sources of insoluble fiber (wheat bran, cellulose) have no effect. Rice bran lowers cholesterol, but the effects appear to be produced by nonfiber components. The cholesterol-lowering effect is small but within the practical range of intake. For example, 3 g of soluble fiber from oatmeal (84 g) decreases total and LDL-C by about 0.13 mmol per L (101). The addition of psyllium supplements (10.2 g per day) to a prudent American Heart Association diet can lower total cholesterol by about 5% and LDL-C by 8.6% (102). Although a decreased intake of saturated fat is the most important dietary factor in lowering serum cholesterol, the effect of soluble fiber is comparable with decreasing dietary cholesterol to below 200 mg per day and with a weight loss of 5 kg (103).
Treatment of Inflammatory Colitis. Some products of the fermentation of fiber (especially short-chain fatty acids, primarily butyrate) are an important energy source for colonic mucosal cells. Infusions of sodium butyrate (100 mmol per L) in the form of enemas may relieve ulcerative colitis (UC) and diversion colitis, but the data are not consistent, and a strong recommendation cannot be made with current information (104). Based on data mostly in rodents, it is possible that dietary fiber plays a role in immunomodulation, as evidenced by changes in inflammatory markers, but data in humans are virtually absent (105).
Indications for Modified-fiber Diets
Current Consumption Levels
Total dietary fiber intake has been only about half of the recommended intake in recent decades in the United States, estimated as 11 to 13 g per day in NHANES II (1976–1980) (92) and as 10 to 14 g per day in NHANES III (1988–1991) (80,106). Fewer grain products are consumed on average than in the 1930s and 1940s, but more fresh fruits and vegetables are now consumed throughout the year than previously.
Adequate Intake Values (g/day) for Total Fiber |
Life Stage (year) | Male | Female |
1–3 | 19 | 19 |
4–8 | 25 | 25 |
9–13 | 31 | 26 |
14–18 | 38 | 26 |
19–50 | 38 | 25 |
51–>70 | 30 | 21 |
Pregnancy/lactation |
| 28/29 |
Source: Food and Nutrition Board, Institute of Medicine, Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). Washington DC: National Academies Press, 2005.
Recommended Intake
The recommendations of the IOM committee on macronutrients considered the availability of food fiber and added (or functional) fiber, as well as the amount of fiber needed to deliver possible health benefits when estimating the dietary recommended intake for fiber. Not enough data were available to provide an estimate average requirement (EAR), so an adequate intake (AI) was used to meet the average needs of a healthy population (Table 12-13).
Low-Fiber Diet
This diet is indicated whenever decreased fecal bulk is desired, as during preparation for barium studies or intestinal surgery, although a clear liquid diet is often preferred in such cases. A low-fiber diet may be used in acute diarrheal illnesses, such as gastroenteritis and UC, and in SBS when the colon is still present. This diet is not indicated for the long-term treatment of diverticular disease or IBS. In patients with diverticulitis presenting with a chronic partial obstruction of the colon, a low-fiber diet may be used temporarily. Partial obstruction of any part of the intestinal tract (e.g., pylorus, colon) may be managed either by mechanical softening of foods (more useful for upper intestinal obstructions) or by a low intake of fiber (more useful for lower-intestinal obstructions).
Partial Low-Fiber Diet
Sometimes, a diet with only a moderate restriction of fiber is indicated. When an ileal segment is very narrow in a patient with Crohn disease, only the most indigestible of the fiber sources need be eliminated (bran buds, corn, nuts); the other fiber-rich foods often can be consumed in moderation. Gastric phytobezoars can be treated initially with a full low-fiber diet; however, to prevent recurrences, the elimination of pulpy fruits (citrus fruits, pears) and persimmons from the diet is sometimes sufficient. Alternatively, a modified low-fiber diet can be used, in which only the foods highest in fiber (Table 12-13) are avoided. Examples include fruits (oranges, grapefruits, prunes, raisins, figs, cherries, persimmons, apples, grapes, berries), vegetables (celery, pumpkin, sauerkraut, lettuce, broccoli, brussels sprouts, potato skins), and others (bran, coconut, peanut, popcorn, kidney beans). An unusual food therapy for gastric phytobezoars is the use of Coca-Cola, based on no known mechanism. Forty-six patients have been reported in 24 publications, using 0.5 to 3 L per day for 1 day to 6 weeks, and demonstrating efficacy in most cases (107). However, none of the reports is controlled, and there is every reason to think that high-volume washing of the stomach might be effective.
High-Fiber Diet. A high-fiber diet is used in the long-term treatment of recurrent diverticulitis (not simple diverticulosis) and irritable bowel disease when altered bowel habit is a major symptom. A high-fiber diet is not essential for every healthy adult who is ingesting the recommended amount of dietary fiber per day (Table 12-13). It is sometimes used nonspecifically in the treatment of chronic diarrhea to produce semiformed, less liquid stools, especially as a fiber-supplemented enteral formula (108). However, the effect is often produced at the expense of an increase in the number or volume of stools. Moreover, if a high-fiber supplement is administered to a patient through a small-bore tube, the tube may become obstructed. For these reasons, a high intake of fiber must be used cautiously in most cases of diarrhea.
Practical Aspects
A clear liquid diet may be substituted for a low-fiber diet, but only for a short time because caloric intake is insufficient. Alternatively, commercially prepared liquid diets can be used (see Chapter 10). Table 12-14 lists total dietary fiber per average serving. Both high-fiber and low-fiber diets can be derived from such tables. Low-fiber diets are adequate in protein and fat. If dairy products are eliminated from the diet because of lactose intolerance, protein and calcium intake from other sources should be increased.
Commercial Psyllium Powders
These powders contain about 3.4 g of psyllium mucilloid per teaspoon. Because preparations are produced and packaged differently, the instructions for use of each product should be carefully followed and not transferred to other products. Some plants (e.g., Plantago) are very rich in psyllium, which comprises 10% to 12% of soluble fiber. The exact conversion of grams of psyllium to total dietary fiber is uncertain, but a 1:1 equivalence is probably nearly correct, and a suitable estimate for practical application.
Fiber Content/Serving of Commonly Used Foods |
Total Dietary Fiber 5 g
Baked beans (1/4 cup)
Split peas (1/2 cup)
Chick peas, kidney beans, lentils (1/2 cup)
Butter beans, cooled (1/2 cup)
Blackberries (1/4 cup)
Grapes, white (12)
Raspberries (1/2 cup)
Bran wheat (1/4 cup)
All-Bran, raisin bran (1/3 cup)
Shredded Wheat (2 biscuits)
Almonds (15)
Grapenuts (1 cup)
Prunes, stewed (1/2 cup)
Total Dietary Fiber ~4 g
Peas, fresh or canned (1/2 cup)
Turnip greens (1/2 cup)
Broccoli (1 cup)
Cranberries (1 cup)
Prunes, dried (3)
Pear with skin (1 medium)
Apricots (5)
Apple (1 large)
Figs, dried (2)
Total Dietary Fiber ~3 g
Beets, boiled (1/2 cup)
Potato with skin, baked (one 2 1/2-in diameter)
Rye crackers (4)
Fruit pie (9-in diameter, 1/6 of pie)
Corn flakes (1 cup)
Total Dietary Fiber ~2 g
Banana (1 small)
Peach (1 medium)
Potato (1 medium with skin)
Corn on cob (small ear)
Carrot (1 medium)
Cabbage, boiled (1/2 cup)
Tomato (1 medium)
Turnips (2/3 cup)
Cauliflower, raw (1 cup)
Rhubarb (1/4 cup)
Strawberries (10 large)
Plums (2 medium)
Orange (flesh) (1 small)
Tangerine (1 large)
Cherries (15)
Puffed wheat (1 cup)
Corn flakes (1 cup)
Flour, wholemeal (3 tbsp)
Peanut butter (2 tbsp)
Bran, powdered (1 tbsp)
Rye bread (1 slice)
Whole wheat bread (2 slices)
Total Dietary Fiber ~1 g
Onion (1 small)
Cauliflower, boiled (1/2 cup)
Celery, raw (1/2 cup)
Potato, boiled, no skin (1 medium)
Asparagus, boiled (4 spears)
Cucumber, raw (2 cups)
Rice Krispies (3/4 cup)
Special K (3/4 cup)
White bread (1 slice)
Popcorn (1 cup)
Raisins (1 tbsp)
Nectarines (1 medium)
Melon, all types (1/4 melon)
Pineapple, fresh (1/2 cup)
Grapefruit (1/2)
Rice, boiled white (1/2 cup)
Flour, white (3 tbsp)
Peanuts (12)
Total Dietary Fiber,0.2 g
Fruit juices, strained (1 cup)
Sugar, white (1 tbsp)
Mayonnaise (1 tbsp)
Fruit jellies (1 tbsp)
Fats (2 tbsp)
Milk (1 cup)
Egg (1 medium)
Meat, fish, poultry (3 oz)
Coffee, tea, soda (1 cup)
Sources of Fiber
High-fiber diets can be based on foods with moderate or high amounts of fiber. Commercial psyllium seed may be used instead of, or in addition to, a high-fiber diet or a bran preparation, but this is not recommended for increasing fiber intake in healthy populations. The type of fiber is different in each source, and the effects are occasionally additive. Most often, however, a patient responds to one or another source of fiber. The psyllium seed preparations are easy to take, their effects are reproducible, and they eliminate the need to use a special diet. However, in some instances, they are ineffective, whereas other types of fiber relieve symptoms. Most dietary fiber in a Western-type diet comes from fresh fruits, vegetables, and cereals. Usual servings of fruits, vegetables, and cereals contain 2 to 4 g of dietary fiber (Table 12-14).
High-Fiber Diet
High-fiber diets should aim to add the equivalent of at least 10 g of total dietary fiber to the diet. This increment may be accomplished by adding a normal distribution of fiber-containing foods to the previous diet, or the use of a single, concentrated source of fiber may be required. The importance of obtaining a dietary history is obvious. Psyllium seed provides 6 to 7 g of fiber in a dosage of 2 tsp per day; All-Bran cereal contains 11.2 g of dietary fiber in each cup; wheat bran contains about 5 g of dietary fiber in each tablespoon. In general, ingestion of two to three doses per day provides 10 g of additional dietary fiber. Keep in mind that not all sources of fiber produce the same effect (Table 12-11). Thus, it is best to increase foods containing dietary fiber. If added (or functional) fiber is used, it may be necessary to try different types of fiber supplement before finding one that improves symptoms or is well tolerated.
Prebiotics are an increasingly common source of fiber that are available over the counter. The major sources of prebiotics available in Europe and the United States are inulin (derived from chicory roots), fructo-oligosaccharides or oligofructose (derived from the hydrolysis of chicory inulin or synthesized from sucrose), galacto-oligosaccharides (synthesized from lactose), and soybean oligosaccharides (extracted from soybeans). The average chain lengths of most of these are quite short, with only three to four residues, except for inulin, which has an average of 10 residues, and they comprise the classification of RSCCs (68). They are used as fat or sugar replacements and to add body to a variety of products, including dairy products, breakfast cereals, baked goods and breads, chocolate and confections, dietetic products, table spreads and salad dressings, and meat products. These supplements should be included on the label of the food products to which they are added, although the amount added may not be specified.
Fiber is being included in enteral feeding formulas for use both in hospital and in the community. Forty-three RCTs have been analyzed, demonstrating a decrease in the diarrhea caused by enteral feedings (109). Bowel frequency was reduced when baseline frequency was high, and increased when it was low. Xanthan gum, a polysaccharide secreted by the bacterium Xanthomonas campestris, is a common food additive used as a thickening agent. It has been provided as a powder to thicken food and beverages for patients with oropharyngeal dysphagia (Resource Thicken Up Clear™), and provides 7 g of fiber per tbsp.
Low-Fiber Diet
Allowed foods are mainly animal foods (eggs, meats, milk), fats, white bread or rice, strained juices, and low-fiber fruits and vegetables, such as peaches without skin and peeled cucumber.
Side Effects
An excess of fiber can increase the frequency of stools in the absence of constipation or worsen the symptoms of chronic constipation. Thus, fiber should be used cautiously to treat constipation as an isolated symptom. Excess fiber may obstruct a structural narrowing of the intestinal tract. When a low-fiber diet is used inappropriately to treat diverticulitis or irritable bowel disease, symptoms may worsen.
Supplements Required
A strict low-fiber diet containing 3 cups of milk per day and some meat servings is adequate for all nutrients except vitamin A (unless liver is eaten) and iron (for female patients). The caloric intake also may be inadequate, depending on the patient. In most cases, the diet is used only for a short time, and nutritional deficiency is not a problem for the nutrient-replete patient.
DIETS THAT RESTRICT OR SUPPLEMENT INDIVIDUAL COMPONENTS
Low-available-carbohydrate Diet
Principles
When gastric emptying is rapid or when food enters the small intestine at an unregulated rate, the presence of small-molecular-weight foodstuffs is to be avoided. Because it is permeable in both directions, the upper small bowel rapidly corrects hypertonic or hypotonic luminal contents to isotonicity. Most meals are hypertonic, so a net loss of fluid into the lumen of the intestine leads to a decreased plasma volume and distention of the upper intestine. The decrease in plasma volume and corresponding increase in intestinal distention accounts for many of the symptoms associated with the dumping syndrome.
Small-molecular-weight soluble substances exert a greater osmotic pressure than do macromolecules. The low-molecular-weight dietary components present in high concentrations are monosaccharides and disaccharides (e.g., dextrose, lactose, sucrose). Free amino acids or dipeptides are rarely encountered in the stomach. Therefore, a diet designed to decrease the osmolarity of ingested food is one low in the type of carbohydrate that is readily available for absorption. Of course, starch can be digested rapidly to maltose and glucose, and so starch also contributes to luminal osmolarity. Because milk sugar is a disaccharide, a low-available-carbohydrate diet is also a low-lactose diet. However, within a given range of osmolarity for liquid solutions such as oral rehydration solutions, it is the carbohydrate content rather than the osmolarity that determines the rate of gastric emptying (110). In people with normal stomachs, high-carbohydrate content decreases gastric emptying, but when the stomach delivers food more rapidly after gastric resection, the mechanism by which carbohydrate regulates gastric emptying is lost, and increased carbohydrate is delivered to the duodenum where it generates increased osmotic pressure.
Different starchy foods are digested at different rates. Moreover, simple sugars vary in their effect on blood glucose levels. Glucose produces a greater effect than sucrose or fructose. Some starches produce a greater effect on blood glucose than do some simple sugars. Factors that affect starch digestibility include particle size, nature of the starch, processing of the starch, presence and type of fiber, and starch–protein–fat interactions (111,112). Because of the difficulty in predicting the effects of starchy or sugar-containing foods on blood glucose levels, the glycemic index (GI) was developed. The GI is defined as follows:
[Area under the 2-h glucose curve for food ÷ area under the 2-h glucosecurve for an equivalent weight of reference sugar] × 100
The original reference sugar was glucose, but bread baked from flour of known composition has proved a better standard. A lower mean glycemic load (GL) in the diet (GI of food times total daily carbohydrate intake) was associated with a twofold lower risk for the development of diabetes and CVD in the large Nurses’ Health Study (86). Review of 11 RCTs found that a low GI or low GL decreased glycated hemoglobin, HbA1c, with no increase in hypoglycemic episodes (113). Review of 24 RCTs found that a low GI lowered serum cholesterol and LDL-C modestly, but no effect was found on HDL cholesterol and triglycerides (114).
Despite this apparent effect on some CV risk factors, a meta-analysis of 15 RCTs using low–GI diets showed only a weak effect on reducing coronary heart disease, but these studies also showed none on LDL or HDL cholesterol (115). A low-carbohydrate diet may not be enough to alter the natural history of CV disease. Follow-up of two large prospective studies involving more than 120,000 patients found that a low-carbohydrate diet, including animal fat and protein, was associated with a higher all-cause mortality, but a low-carbohydrate diet based on vegetable sources was associated with a lower all-cause and CV disease mortality rates (116). When a low-carbohydrate diet is coupled with behavioral treatment, leading to weight loss of approximately 8 kg, there are favorable changes in serum lipids at 1 year, although these improvements were no longer evident at 2 years (117). Thus, the data are not yet consistent enough for a clear recommendation. Moreover, it is not clear what role various factors play in modifying the glycemic potency of foods, and its use in routine clinical management is still controversial.
Indications
Dumping Syndrome
The low-available-carbohydrate diet is useful after vagotomy with or without a drainage procedure because many patients have vasomotor and abdominal symptoms of the dumping syndrome (postprandial nausea, vomiting, weakness, dizziness, cramping, diarrhea, flushing, palpitations) during the early postoperative period (118). The rate of gastric emptying of fluids is enhanced at this time. However, the rate eventually returns to normal and the symptoms subside. Only a few patients must maintain the full diet on a long-term basis, although a large number may remain on a somewhat restricted diet. Some of the symptoms associated with dumping occur 1 to 3 hours after a meal; these may be caused by reactive hypoglycemia (see below). The diet also diminishes such symptoms by decreasing the carbohydrate load. The anatomic configuration of patients who have undergone gastric bypass for obesity (not gastroplasties) is associated with the dumping syndrome because the fundus of the stomach is anastomosed to the jejunum, and such patients often must remain on a low-available-carbohydrate diet.
Reactive Hypoglycemia
This occurs rarely in the absence of gastric surgery, sufficient in degree to produce symptoms (dizziness, hunger, weakness, sweating, palpitations). However, these symptoms are nonspecific and often related to anxiety. The true incidence of reactive hypoglycemia is probably much lower than the frequency of the diagnosis suggests. The definitive diagnosis requires the production of typical symptoms during a 5-hour glucose tolerance test, accompanied by a low plasma glucose level (<50 mg per dL). When reactive hypoglycemia is present, the low-carbohydrate diet is helpful.
SBS Without a Colon
Although it is not widely accepted that an increased intake of fat may be indicated therapeutically, a few reports suggest the possible usefulness of such a maneuver. The rationale is that fat delays gastric emptying and prolongs small-bowel transit time via a humorally mediated mechanism termed the ileal brake (119). A high-fat diet has been used in some cases of SBS (120). The rationale is that in a person with a short bowel and no colon, the importance of unabsorbed fatty acid derivatives as colonic secretagogues is limited. Thus, water secretion is regulated by the osmolarity of the diet, which is lower with a low intake of complex carbohydrate and a high intake of fat. Gastric emptying may also be delayed by a high-fat meal, preventing too rapid presentation of calories to the remaining small intestine, but the same effect probably occurs with high-complex-carbohydrate diets (121).
Sucrase–Isomaltase Deficiency
Congenital sucrose–isomaltase deficiency is a rare autosomal recessive disorder, but the incidence of heterozygotes in the United States of America is estimated to be as high as 8.9% (122). For infants with sucrase–isomaltase deficiency, glucose or fructose may be added to formulas that contain no carbohydrate (see Chapter 10). Sucrose is added to many commercial baby foods, especially puréed fruits. Labels should be read carefully. Older children with this disorder become more tolerant to sucrose, and the diet is less necessary. An unsupplemented low-sucrose diet may be limited in ascorbic acid and folic acid, and perhaps also iron, thiamine, and niacin. An FDA-approved oral solution is available containing sucrase from Saccharomyces cerevisiae (baker’s yeast), marketed as Sucraid (sacrosidase) (www.sucraid.net). The usual dose is 1 to 2 mL per meal. About three-fourths of treated patients can be reasonably asymptomatic while ingesting sucrose. The most common side effects are abdominal pain, vomiting, and allergic reactions.
Low-Carbohydrate Diet for Obesity and CVD
The basis for the low-carbohydrate diet for metabolic disorders remains unproven. It is clear that weight loss can occur, but the effect is not long-lasting (123), and it could be due to a decrease in food intake, secondary to limited food choices that achieves portion control in a manner that is not specific to meal content. In fact, a review of low-carbohydrate diets found that it is the duration of diet and restriction of energy intake, not restriction of carbohydrates, that leads to weight loss (124). With current information, a low-carbohydrate diet itself cannot be recommended to decrease weight long term or to decrease the risk of metabolic disorders.
Low-Carbohydrate Diet Postoperatively Following Bariatric Surgery That Includes Gastric Bypass
When a gastric bypass is created, food from the small fundic pouch moves directly into the jejunum, creating an anatomical situation that produces dumping syndrome. The diet is restricted in volume, but also avoids concentrated sugars and alcohol (125). Patients should eat and drink slowly, take small bites, and chew well to avoid distending the gastric pouch or producing staple dehiscence.
Functional Gastrointestinal Disorders and Low–FODMAP Diet
In the early 2000s, an elimination diet (FODMAP) was introduced to reduce symptoms in patients with functional gastrointestinal disorders (FGIDs), but has achieved its widest use in IBS. FODMAP is an acronym for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These diet components are either osmotically active themselves or ferment rapidly in the colon and/or small bowel to become osmotically active. The theory is that by producing more intraluminal volume and altering intestinal microflora, these food components lead to GI symptoms (126). Indeed, such food components have been shown to increase stool volume and gas production. Evidence that diets restricted in FODMAP components improve symptoms in patients with FGIDs, however, is more controversial. Several studies show that 75% of FGID (127) or IBS (128) patients show improvement in bloating, abdominal pain, or gas. However, these results have been achieved in patients who complain of those symptoms and who tend to be ingesting FODMAP–containing foods. Thus, the diet may be most useful in patients who are exaggerating the symptoms from their underlying disorder because of ingestion of foods that induce luminal gas and fluid production. The best way to establish the validity of eliminating such foods is by a double-blind placebo-controlled food challenge, but this is not practical in practice (129). The best approach is to provide individual guidance regarding FODMAP–rich foods, often with the assistance of a trained dietitian (126,129,130). The long-term implications of such a diet are unclear in that the FODMAP elimination diet removes many fruits and vegetables felt to be otherwise foods that might prevent some chronic diseases, and reduces luminal Bifidobacteria, a so-called “good” bacterial genus (131). This uncertainty about microbial composition, along with uncertainty about efficacy, has led to caution about advocating this diet for all patients with FGID (132). One should instead ascertain whether foods likely to be rich in FODMAPs are being ingested and contributing to symptoms, prior to restricting them on a trial basis.
Fructose Intolerance
Fructose absorption is more limited than that of glucose, but is quite variable, ranging from 5 to 50 g in absorption studies with fructose administration alone (133). This is because the intestinal transport of fructose is mediated by the facilitative transporters GLUT5 and GLUT2 (134). GLUT7 is another facilitative hexose transporter that accepts fructose as a substrate (135). However, fructose malabsorption can be modulated by glucose, possibly by increasing solvent drag. Most dietary forms of fructose (sucrose, honey) contain fructose and glucose in a 1:1 ratio, thus limiting the clinical effect of fructose malabsorption (133). HFCS may contain more fructose relative to glucose, but many preparations of HFCS contain high-molecular-weight glucose polymers that provide variable available glucose. Fruits such as apples, pears, and watermelon contain more fructose than glucose, but the ratio in vegetables is close to 1:0. Thus, it is difficult to interpret the correlation of hydrogen breath tests (suggesting malabsorption) with symptoms, as this must be tested using usual dietary intake with glucose. Whether patients do demonstrate true fructose intolerance must be decided on an individual basis. The most common setting appears to occur in patients who ingest large volumes of beverages containing HFCS. In such cases, what is needed is restriction of HFCS ingestion, not a fructose-restricted diet.
There is a large literature suggesting that excessive fructose ingestion is a risk factor for metabolic diseases, including fatty liver (136). However, it is unclear whether the effect, if real, is due to fructose or to HFCS, or whether the metabolic changes simply reflect differences in caloric intake (137). The available evidence suggests that fructose in its natural form is not associated with adverse effects, but that fructose in the form of HFCS may overwhelm the ability of tissues to handle large amounts of fructose. Excessive intake of refined sugar may explain, in part, the high incidence of metabolic disease, but rapidly absorbed sources of sugar (present either free or as part of high GI starch) also contribute to cardiometabolic disease (138). It also seems unlikely that replacing fructose with glucose will suffice to reverse the metabolic changes seen with HFCS, as increased calories and high GI can produce similar results (138).
Practical Aspects
1. Timing. Food should be taken as six dry meals per day. Because liquids leave the stomach faster than solids, it is better to allow solid foods, with a potentially high osmotic load, to liquefy slowly and be diluted with endogenous secretions. Liquids should be taken 30 to 45 minutes after solids and limited to 1 cup per meal.
2. Milk in all forms, including ice cream and other frozen desserts, should be avoided. Even lactose substitutes contain high concentrations of monosaccharides, disaccharides, or both. Only calorie-free beverages should be consumed.
3. Sugar, sweets, candy, syrup, chocolate, and gravies should be avoided.
4. The stomach should not be overloaded.
5. Foods likely to be high in sugars have the following listed as the first or second ingredient: brown or invert or table sugar, corn sweetener, corn syrup, dextrose, fructose, fruit juice concentrate, glucose, HFCS, honey, lactose, maltose, malt syrup, molasses, sucrose, or syrup.
6. Patient education materials on a diet for dumping syndrome are also available on the Internet from the University of Pittsburgh Medical Center (http://www.upmc.com/patients-visitors;education/nutrition/pages/dumping-syndrome-diet.aspx) and from the University of Virginia (http://www.medicine.virginia.edu/clinical/departments/medicine/division/digestive-health/nutrition-support-team/patient-education/postgastrectomy%20-%20dumping?2011-2010.pdf).
7. Osmolarity of foods. Simple sugars and low-molecular-weight carbohydrates, in addition to electrolytes and amino acids, all contribute to the osmolarity of food, either as a preformed liquid or after liquefication in the intestinal lumen. Dietary fats are relatively water-insoluble and do not increase osmolarity significantly.
One major aim of a low-available-carbohydrate diet is to reduce the osmolarity of ingested foods. This diet eliminates foods with a sugar content likely to increase the osmolarity of the gastric contents. The osmolarity of the gastric contents is usually hypertonic after a meal, but iso-osmolar liquids are emptied most efficiently by the stomach. A diet low in available carbohydrate is used to lower the gastric and intestinal osmolarity as much as possible.
In acute disorders such as gastroenteritis, in which gastric emptying is impaired, or in chronic disorders such as diabetic gastroparesis, the use of iso-osmolar foods is helpful. Unfortunately, such a diet may be low in calories because it is the calorie-containing components of food that contribute most to osmolarity. Moreover, fat decreases the rate of gastric emptying, so low-fat liquids are needed for rapid gastric emptying. During acute illnesses, however, iso-osmolar low-calorie liquids can be used for short periods alone.
Nearly all liquid or semisolid foods are hyperosmolar (1) (Table 12-15). When nausea or vomiting is among the symptoms to be treated, the use of these fluids should be modified so that appropriate dilutions decrease the osmolarity to about 280 to 300 mOsmol per L.
8. Foods allowed include those containing protein, fat, or complex polysaccharides.
Foods containing simple sugars should be avoided. Table 12-16 lists the fructose, glucose, sucrose, and starch contents of many foods. In this table, foods are ranked in decreasing order of simple sugar content—that is, monosaccharides and disaccharides. Foods high in simple sugars should be avoided or taken in small amounts. Fructose in excess of glucose is the main determinant of fructose malabsorption and diarrhea. This excess is seen especially in honey, apples, and pears. However, the largest source of dietary fructose is as a sweetener in dietetic foods and soft drinks and in corn syrups (~50% fructose) (139). The mean daily intake of free fructose in the United States is 20 g. Sorbitol is ingested in fruits along with fructose, and as a sweetener in candy, mints, “sugarless” chewing gum, and dietetic foods. As much as 2 g of sorbitol can be contained in one stick of gum. The decreased carbohydrate absorption of fruit juices in young children is related to the sorbitol content of the juice (140). The lactose contents of milk products are listed in Table 12-17, and these should also be limited. In congenital sucrase–isomaltase deficiency, a rare disorder, only foods containing little sucrose can be ingested. As seen in Table 12-16, this diet eliminates many fruits and vegetables and most sweets.
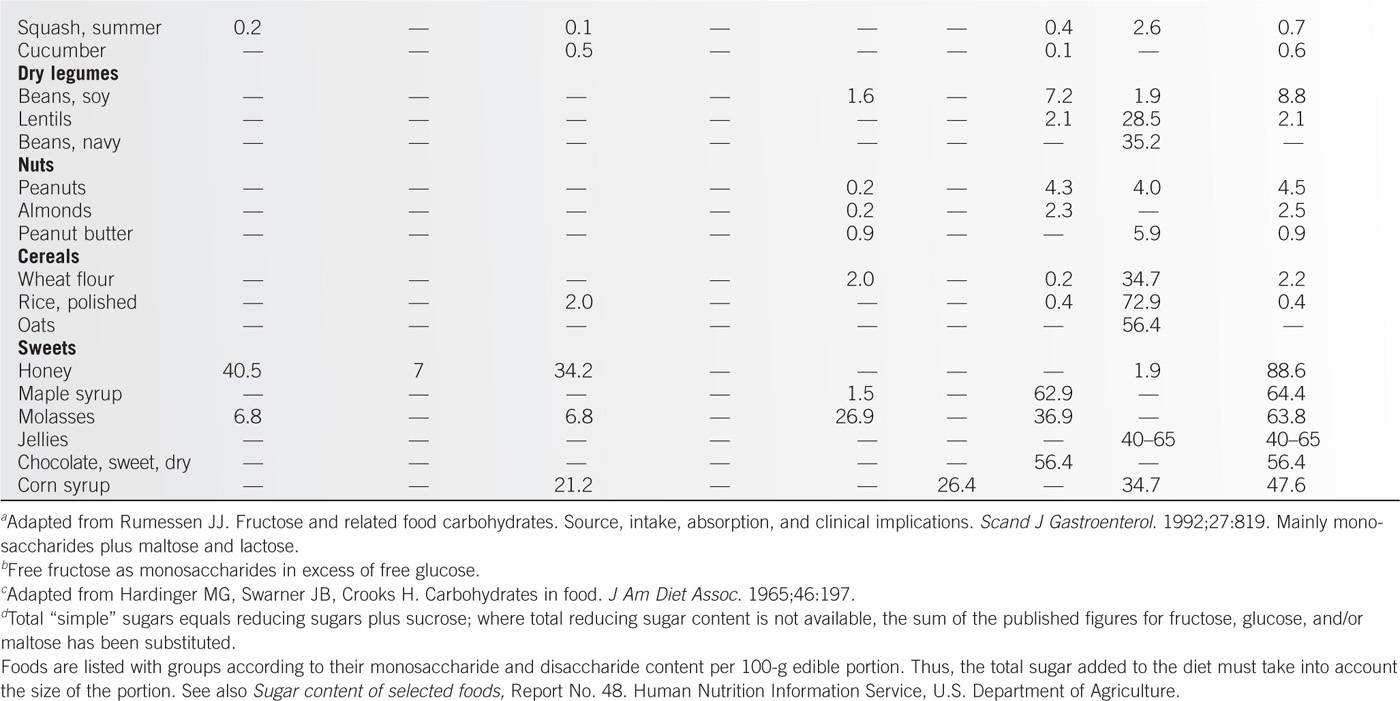
Lactose Content of Selected Milk Products |
Product | Lactose Content (g/unit) |
Whole milk (1 cup) | 11 |
2% Milk (1 cup) | 9–13 |
Skim milk (1 cup) | 11–14 |
Chocolate milk (1 cup) | 10–12 |
Sweetened condensed milk (1 cup) | 35 |
Reconstituted dry whole milk (1 cup) | 48 |
Buttermilk (1 cup) | 9–11 |
Light cream (1 tbsp) | 0.6 |
Half and half (1 tbsp) | 0.6 |
Whipped cream topping (1 tbsp) | 0.4 |
Low-fat yogurt (1 cup) | 11–15 |
Cheeses |
|
Hard (Parmesan, blue, Gouda) (1 oz) | 0.6–0.8 |
Semihard (American, Cheddar) (1 oz) | 0.4–0.6 |
Soft (Camembert, Limburger) (1 oz) | 0.1–0.2 |
Spread (added cream) (1 oz) | 0.8–1.7 |
Cottage |
|
Regular (1 cup) | 5–6 |
Low-fat (1 cup) | 7–8 |
Ice creams |
|
Regular (1 cup) | 9 |
Sherbet (1 cup) | 4 |
Ice milk (1 cup) | 10 |
Sorbets, ices (1 cup) | 0 |
Butter (1 tbsp) | 0.15 |
Oleomargarine | 0 |
Data from Welsh JD. Diet therapy in adult lactose malabsorption: present practices. Am J Clin Nutr. 1978;31:592.
Most beverages contain available sugars and should be limited. These include beer, sodas, and iced tea or lemonade made with sugar. Canned fruits often contain extra sugar in the packing fluid; if these are used, the fluid should be drained away before the fruits are eaten.
9. Fructose has been singled out as an important component of available carbohydrate in the diet. Average consumption of fructose in the United States is approximately 30 g per year, half from sucrose and half from HFCS. Fructose enters the glycolytic pathway at the level of triose phosphates, thus bypassing the major control point at which glucose enters, that is, phosphofructokinase. Fructose can serve, therefore, as an unregulated source of acetyl CoA for hepatic lipogenesis. Fructose has been shown in short-term studies to increase energy intake and body weight, to decrease insulin sensitivity, and to increase postprandial plasma triglyceride levels (141). A low-carbohydrate diet should also be low in fructose.
10.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree