Type 2 diabetes: epidemiology, complications and costs
EPIDEMIOLOGY
Changes in lifestyle over the past century have resulted in a dramatic increase in the incidence of type 2 diabetes worldwide. Once a disease of Western affluent societies, it has now spread to every country in the world and is increasingly common among the poor. Once almost unheard of in children, rising rates of childhood obesity have rendered it more common in the paediatric population, especially in certain ethnic groups. Recent estimates from the Global Burden of Disease Study indicate that diabetes rates around the world rose 45% between 1990 and 2013, primarily in type 2 diabetes (Global Burden of Disease Study 2013 Collaborators, 2015). According to the International Diabetes Federation, diabetes affected at least 387 million people worldwide in 2014, and that number is expected to rise to 592 million by 2035, with 77% of all diabetes cases occurring in low- to middle-income countries (IDF, 2015).
China and India now account for 60% of the world’s diabetes population. In 1980, less than 1% of Chinese adults had diabetes, but this increased to almost 12% (113.9 million adults) by 2010 (Diabetes in China, 2014). The epidemic is the result of rapid economic development, urbanization and lifestyles that are increasingly sedentary, and poor diets high in saturated fat and calories derived from refined carbohydrates and sugar. Asian people are also particularly susceptible to type 2 diabetes compared with white people and tend to develop the disease at a much lower body mass index (BMI). The average BMI of Chinese people with diabetes is 25 kg/m2, compared with 30 kg/m2 in non-Asians.
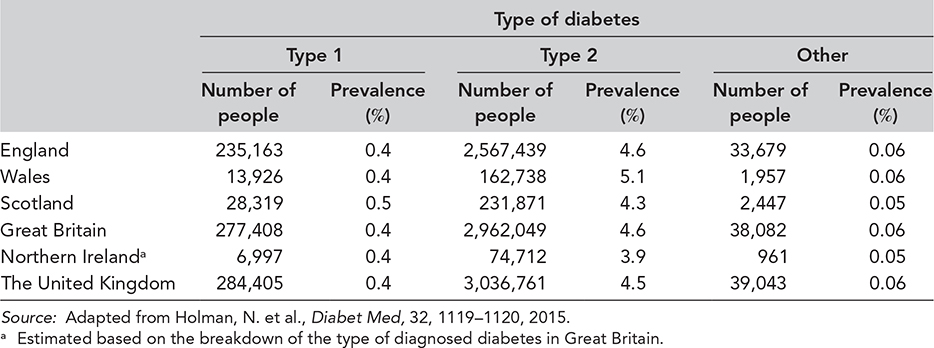
Recent prevalence figures for the United Kingdom have been obtained using data from the Quality and Outcomes Framework for those aged ≥17 years and the National Paediatric Diabetes Audit for England and Wales and the Scottish Diabetes Survey for younger individuals. The data show that at the end of March 2014, there were approximately three million people with a recorded diagnosis of type 2 diabetes, which equates to a prevalence of 4.5% (Table 1.1) (Holman et al., 2015). Throughout the United Kingdom, 1 in 22 people have diagnosed type 2 diabetes. However, these figures do not take into account the numbers of people with undiagnosed type 2 diabetes, currently estimated at around 850,000 (Public Health England, 2014a).
Overweight and obesity are driving the global diabetes epidemic. They affect the majority of adults in most developed countries and are increasing rapidly in developing countries. In the United Kingdom, around 90% of people with type 2 diabetes are overweight or obese (Public Health England, 2014b). The rising prevalence of obesity in the United Kingdom and around the world will continue to lead to a rise in the prevalence of type 2 diabetes. It is estimated that at least half of all cases of type 2 diabetes could be prevented if weight gain in adults could be avoided (Knowler et al., 2002). As a consequence, an epidemic of diabetes-related complications and premature mortality will follow, with people from deprived areas and some minority ethnic groups at particularly high risk.
DIABETES COMPLICATIONS
Diabetes is a chronic disease that causes substantial premature morbidity and death. Over time, damage caused by high blood glucose levels is a major contributing factor to long-term complications, which can be classified broadly as microvascular (including retinopathy, nephropathy and neuropathy) (Figure 1.1) or macrovascular disease (including ischaemic heart disease, myocardial infarction, heart failure and stroke). Without careful, continued management of the condition, a person with diabetes faces a reduced life expectancy of between 6 and 20 years (The Emerging Risk Factors Collaboration, 2011). According to a report conducted by the Health & Social Care Information Centre in 2013, there were around 24,000 premature deaths in England and Wales due to diabetes (both type 1 and type 2) compared to the general population. Those with type 1 diabetes were 131% more likely to die in 2013 than their peers without the condition, and those with type 2 diabetes were 32% more likely to die (National Diabetes Audit: Complications and mortality, 2015). These additional deaths are largely preventable and develop after years of exposure to high glucose, high blood pressure and high cholesterol, which are all signs of poorly managed diabetes. The report assessed the likelihood of a person with diabetes being admitted to hospital for each of a range of diabetes complications, including angina, myocardial infarction, heart failure, stroke, major amputation, minor amputation and renal replacement therapy (dialysis or transplantation). Compared to a person without diabetes, people with diabetes were significantly more likely to be admitted to hospital with one of the complications (Figure 1.2) (National Diabetes Audit: Complications and mortality, 2015).
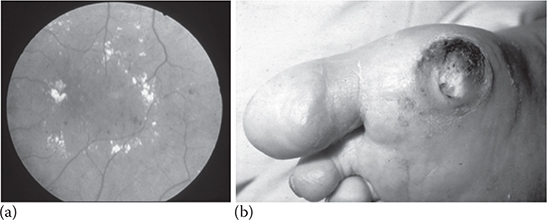
Figure 1.1 Examples of type 2 diabetes associated microvascular complications, including retinopathy and neuropathic ulcer. (a) Hard exudates are visible gathering around the macular region of the retina suggestive of sight threatening maculopathy. Retinal microaneurysms can also be seen. (b) Neuropathic ulcer over the metatarsal head of the big toe.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree