Organisation of diabetes care
ROLE OF THE PRIMARY CARE TEAM IN MULTI-PROFESSIONAL CARE
An important consequence of a chronic condition such as type 2 diabetes is that it is not possible for any one healthcare professional to effectively provide the spectrum of care required. Integrating diabetes care with a team of professionals from a range of disciplines with different but complementary skills, knowledge and experience is critical to success and the prevention of both acute and chronic complications. Members of the team will vary according to the care required and because of other constraints such as resources, clinical setting and geographical location, but may include an ophthalmologist, podiatrist, dentist, dietician, diabetes educator and consultant diabetologist in addition to the general practitioner (GP) and local diabetes specialist nurse.
In the United Kingdom, approximately two-thirds of people with type 2 diabetes are managed entirely in primary care. The primary care team plays an integral role in integrating diabetes care and in ensuring that it is continuous and patient-centred at all stages of the disease. Many people with type 2 diabetes will also have at least one additional chronic health problem, and the primary care team also has the unique ability to provide continuity and coordination of care for patients with multiple chronic diseases.
All team members have a role to play in providing consistent messages, which should reinforce the importance of metabolic control and effective management of other cardiovascular risk factors. This will include emphasising the value of a healthy lifestyle that includes physical activity and healthy eating. They can also emphasise the benefits of attending routine foot, eye and dental check-ups to prevent complications. The end result should be high patient satisfaction with care, good quality of life, improved health outcomes and ultimately lower healthcare costs.
Organizing high-quality care for the rapidly increasing number of people with type 2 diabetes is a major challenge worldwide. Although multi-professional care offers a more diverse range of skills and experience than a single healthcare professional can provide, the coordination of care can be challenging when delivered by multiple individuals in various settings, and it is important to ensure that there is neither unnecessary duplication nor gaps in service delivery and unacceptable delay. Coordination of care works best when there is a clearly identified person undertaking this role within the multi-professional team. In some cases, care coordinators may be directly involved in providing care, whereas in other cases, their role may be to facilitate care provided by other professionals.
The National Health Service (NHS) Five Year Forward View published in 2014, set out a new shared vision for the future of the NHS based around new models of care. It emphasised that over the next 5 years (and beyond), the NHS would need to target the traditional boundaries between primary care and secondary care and community services, which often act as a barrier to the personalised and coordinated health services people require (NHS, 2014), and instead integrate care at all levels to optimise outcomes in people with type 2 diabetes.
Aims of integrated care
The aims of integrated care are as follows:
To provide a high standard of specialised care for individuals with diabetes and their families from a multi-professional team
To provide a greater range of seamless diabetes services closer to patients’ homes
To support those working in primary care to deliver first-class diabetes care
To support and empower people with diabetes to manage their diabetes effectively
To improve access to diabetes services
To improve communication and closer working with GPs and other community services
To provide education, training and support to the healthcare professional working in primary care
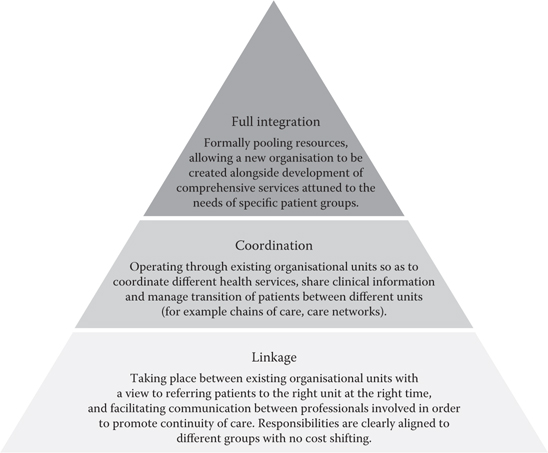
There are many ways of achieving integrated care, and the intensity of integration will vary according to individual circumstances and settings as illustrated in Figure 7.1 (Leutz, 1999).
For example, one solution may be the use of integrated community diabetes services to support primary care such as Intermediate Care Clinics for Diabetes (ICCD). Typically, these are community-based, multi-professional teams, working closely with general practices with the aim of delivering high-quality care nearer to patients. A number of these are already functioning across the United Kingdom. People referred are typically those with poorly controlled type 2 diabetes and/or cardiovascular risk factors. Patients are managed by the ICCD team until the control of risk factors is achieved and then referred back to primary care. Such clinics have been shown to contribute to increased achievement of NICE targets for HbA1c, blood pressure and cholesterol in patients with diabetes, and both patients and primary care physicians have welcomed such enhanced service in the community (Wilson et al., 2014). Cost savings were not observed in a randomised, controlled trial of 49 general practices randomised to usual care or ICCD intervention in which patients were followed for 18 months (Wilson et al., 2014). However, cost savings may not be immediately obvious, as they often relate to the long-term burden of treating complications in secondary care and the effects on patients and their families of morbidity and premature mortality.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree