and Christian Waldherr1
(1)
Bern, Switzerland
8.1 Indications and Advantages of Tomosynthesis-Vacuum-Assisted biopsy (T-VAB)
Indications for T-VAB
Non-palpable masses
Mammographically detected Breast Imaging and Reporting Data System (BI-RADS) 4 and 5 lesions with no correlation on ultrasound (US).
Consider a biopsy of BI-RADS 3 lesions in cases of strong familial history, genetic risk, strong uncertainty, or psychological stress.
Small (<10 mm) architectural distortions.
Caution: distortions >15 mm with the histological result of a benign radial scar require magnetic resonance imaging (MRI) or surgical removal, because the associated malignancy is often localized in the edge region of the radial scar (Case 8.1.1).
A needle deviation in dense tissue or an evasion of the lesion is compensated by suction of the tissue or displacement and by greater tissue extraction, reducing the sampling error, especially in small lesions and discontinuously located malignant cells (ductal carcinoma in situ [DCIS]).
Advantages of T-VAB
3D shows targets without tissue overlap (Case 8.1.2).
3D shows radial lesions or radial distortions (Case 8.1.3).
3D shows distance of target to skin (cc, ml) and detector (Case 8.1.4).
Knowing accurate depth (cc, ml) means knowing the best way to access the target (Case 8.1.5).
We can plan the intervention in advance (access from cranial, lateral, or medial) with high safety (Case 8.1.6).
We are now able to biopsy lesions detected only with tomosynthesis – radial lesions (Case 8.1.7).
A substantial or complete removal of lesions (<10 mm) is possible. Caution: don’t forget a clip marker.
The postinterventional good visibility of the biopsy cavity allows the precise control of the correct sampling point (see image Fig.8.16).
We can biopsy the lesions in viewer steps/improved workflow.
Dose reduction.
Easy to handle.
Avoiding open biopsies.
Vacuum biopsies are temporally brief interventions, especially the T-VAB; Temporally short intervention, particularly in T-VAB, clinically smaller hematomas are currently observed with T-VAB.
Comment
T-VAB is the method with the highest accuracy in the diagnostic evaluation of radial lesions. Radial lesions are difficult to biopsy with conventional stereotactic-guided vacuum-assisted biopsy (S-VAB).
Vasovagal Reaction
Over 90 % of our interventions with T-VAB are performed in the decubitus position.
Fewer than 10 % of our interventions are performed in the upright position; prior medication with Effortil (etilefrine) can be helpful.
Etilefrinhydrochlorid
Boehringer Ingelheim Pharma GmbH & Co.KG, Bingerstr.173, 55216 Ingelheim
Challenges/Problems of S-VAB
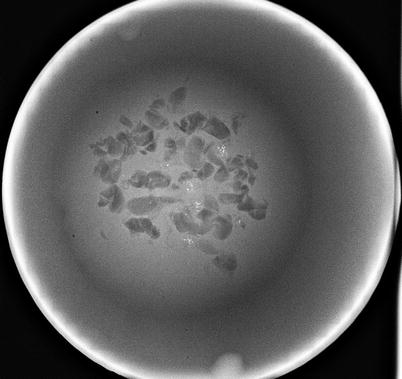
Very fine microcalcifications (MV) re-detection is sometimes difficult (S-VAB Figs. 8.1 and 8.2).
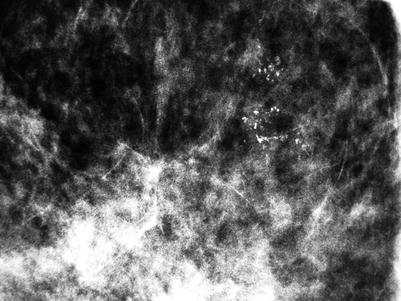
Fig. 8.1

Fig. 8.2
Lesion close to the detector with impossible access pathway; optional—manual entry of the needle to the calculated z-axis (Case 8.1.8).
Occasional required for clarification of focal lesions without associated microcalcifications, stereotactic calculation of the focal depth of the lesion is often problematic, in contrast to most microcalcifications no clear reference point can be determined stereotactically (Case 8.1.8).
Architectural distortions, stereotactic representation of the lesion in both planes may be difficult, target must be identifiable in both 15° shots (Case 8.1.9).
Lesion close to the chest wall may be difficult to reach; in systems with angled needle holder, rarely a problem (Case 8.1.10).
Subcutaneous lesions more difficult to biopsy due to the greater potential to move, insufficient distance of the needle in pre-fire position (needle needs to be withdrawn before firing), and insufficient vacuum suction may be possible (Case 8.1.11).
Long access pathway with the risk of needle deviation, displacement of targets (see Sect. 8.4, Case 1).
Medial access, risk of cutaneous scar on the cleavage.
Small breast with incomplete placement of the needle opening, vacuum suction may be impossible (Case 8.1.12); use plasticine (Play-doh) around the breast to get more breast volume.
Comparison with Breast Surgery
Pain, operation risks, higher costs, postoperative scar, but very accurate.
Disadvantage of Upright System
Movements of the patient may be more relevant.
Less comfortable for patient only in upright position.
Rarely, vasovagal reaction (uncomplicated in decubitus position).
Advantages of Upright System
Device for interventions and diagnostic mammography available.
Several possible approaches for stereotactic/tomoguided intervention ml, cc, obl.
Patients with cervical spine problems are less affected than in the prone position.
8.1.1 Case 1
General Information/Clinical Issues
Patient was a 70-year-old female; screening.
Mammographic Analysis 2D and 3D
Breast density American College of Radiology (ACR) III. On 2D non-specific density right side and only diffusely distributed monomorphic microcalcifications, no mass or distortion (Fig. 8.3a, b); BI-RADS 0. On 3D 2 cm architectural distortion at 12 o’clock position (Figs. 8.4a–c, 8.5, and 8.6 [3D magnification (same figure as 8.4b, c]); BI-RADS 4.
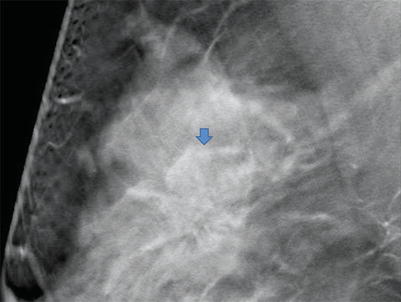
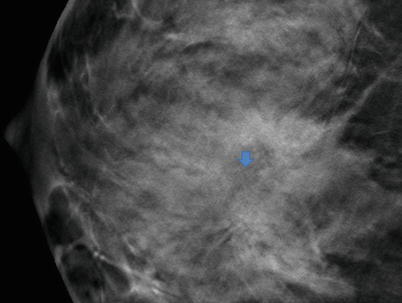
Fig. 8.3
(a, b) 2D Robl (a) and Rcc (b) in 2012
Fig. 8.4
(a–c) 3D Robl slices (a, b) and Rcc (c) in 2012
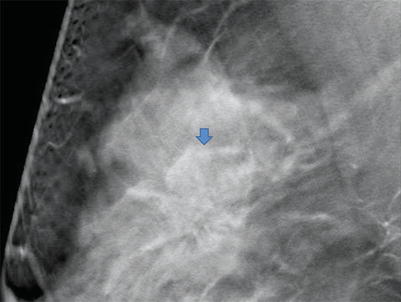
Fig. 8.5
3D Robl magnification
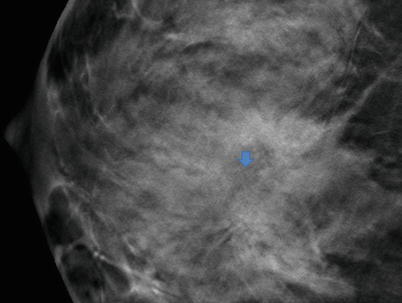
Fig. 8.6
3D Rcc magnification
Recommendation
US with biopsy; MRI can be a problem solver.
Histology of US-Guided Biopsy
Fibrosis, ruptured cyst, granulating inflammation, B2.
Explanation
Histological result maybe conclusive with the radiologic appearance of the lesion on 2D, but is not conclusive with the radiologic appearance of the lesion on 3D, MRI recommended with or without MRI-guided biopsy.
MRI
Ill-defined 10 mm lesion at 12 o’clock with type III curve (Fig. 8.8), MRI-guided biopsy recommended.
Fig. 8.8
MRI
Histology of MRI-Guided Biopsy
Invasive ductal carcinoma.
Final Histology
pT1cpN0(0/2)R0.
Further Imaging/Further Diagnostic
MRI recommended.
Comment:
Distortions >15 mm with the histological result of a benign radial scar require MRI or surgical removal, because the associated malignancy (10 %) is often localized in the edge region of the radial scar.
Image Interpretation Pearls:
MR-guided biopsy – > go for the most aggressive-looking part of the lesion.
8.1.2 Case 2
General Information/Clinical Issues
Patient was a 69-year-old female, status after breast surgery both sides right craniolateral and left caudal (papillomas) in 1988, hormone replacement therapy from 1997- to 2010.
Mammographic Analysis 2D, 2D (Synthetic), and 3D
Breast density ACR III. On 2D in 2010 heterogeneous dense breast tissue, no mass, may be postoperative scar right side lateral (Fig. 8.9a, b); BI-RADS 2. On 2D (synthetic) in 2013 radial 11 mm lesion lateral right side (Figs. 8.10a, b and 8.11a, b); BI-RADS 4. 3D shows radial lesions on both sides, 11 mm right lateral (Figs. 8.12a and 8.13a), 5 mm left mediocaudal (Figs. 8.12b, 8.13b, and 8.14 3D magnification (same figure as 8.12b)); occult on 2D (synthetic) (Fig. 8.10b and 8.11b); BI-RADS 4.
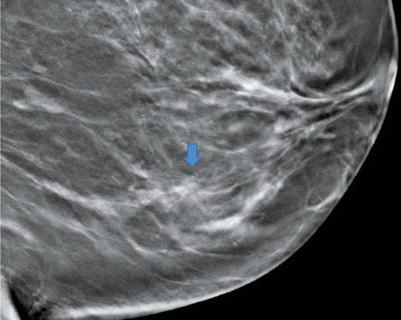
Fig. 8.9
(a, b) 2D Robl (a) and Rcc (b) in 2010
Fig. 8.10
(a, b) 2D synthetic Robl (a) and Lobl (b) in 2013
Fig. 8.11
(a, b) 2D synthetic Rcc (a) and Lcc (b) in 2013
Fig. 8.12
(a, b) 3D Robl (a) and Lobl (b) in 2013
Fig. 8.13
(a, b) 3D Rcc (a) and Lcc (b) in 2013
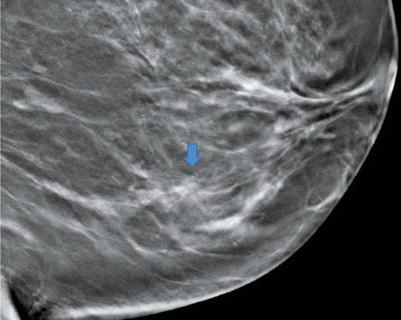
Fig. 8.14
3D Lobl magnification
Conclusion/Diagnosis with 2D (Synthetic)
Suggestive of malignancy right side (BI-RADS 4).
Conclusion/Diagnosis with 3D
Suggestive of malignancy both sides (BI-RADS 4).
Recommendation
US (in biopsy standby) or T-VAB; MRI can be a problem solver with differentiation between postoperative scar and malignant tumor.
US
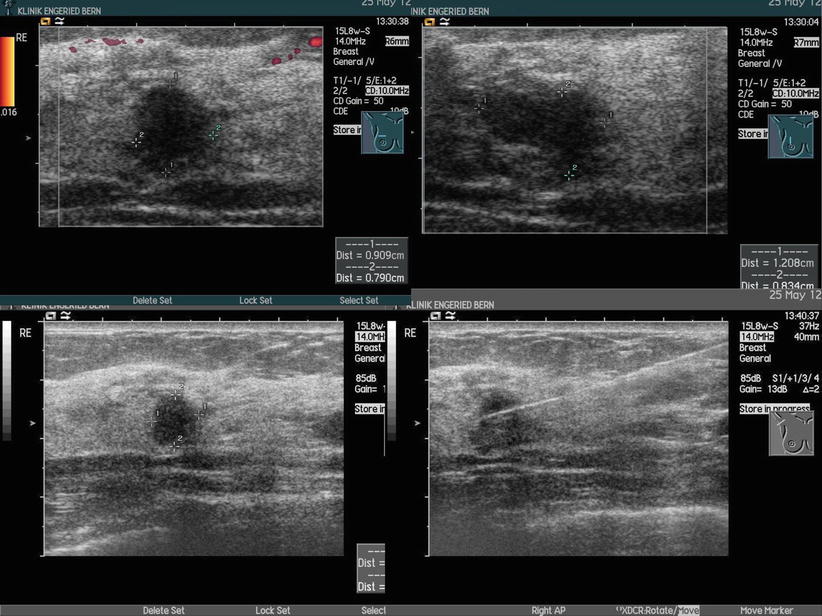
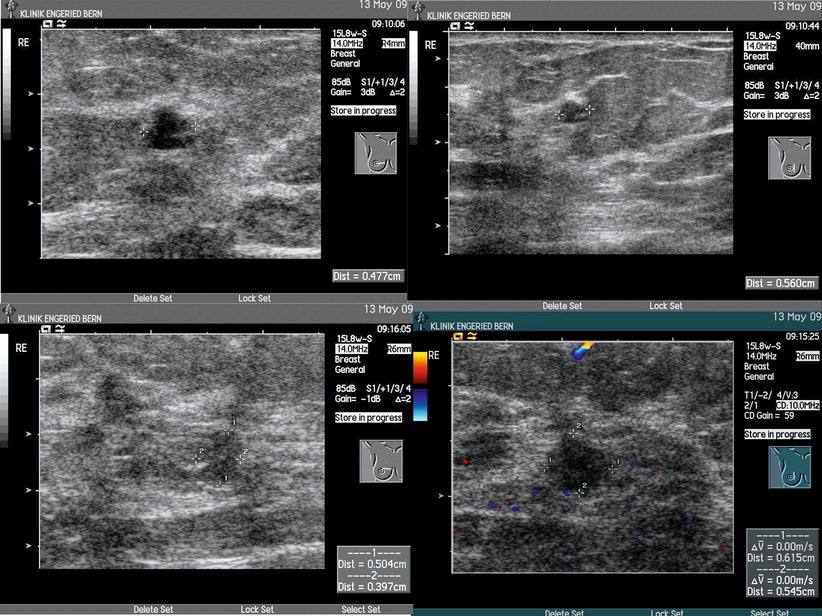
Ill-defined hypoechoic round lesion with posterior shadowing at 9 o’clock right side (Fig. 8.15), biopsy recommended; BI-RADS 4 right side; the small radial lesion on the left side could not be found on US; BI-RADS 0 left side; T-VAB recommended (Fig. 8.16).
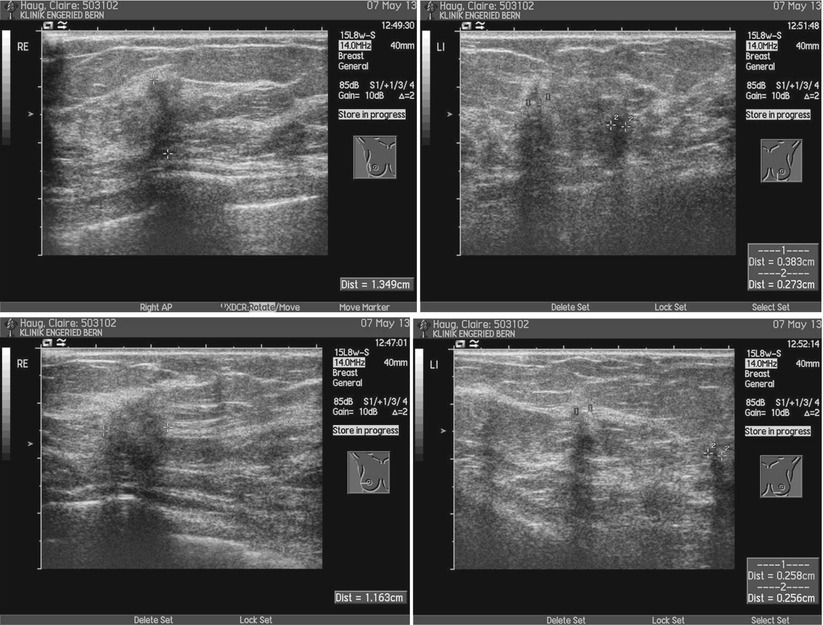
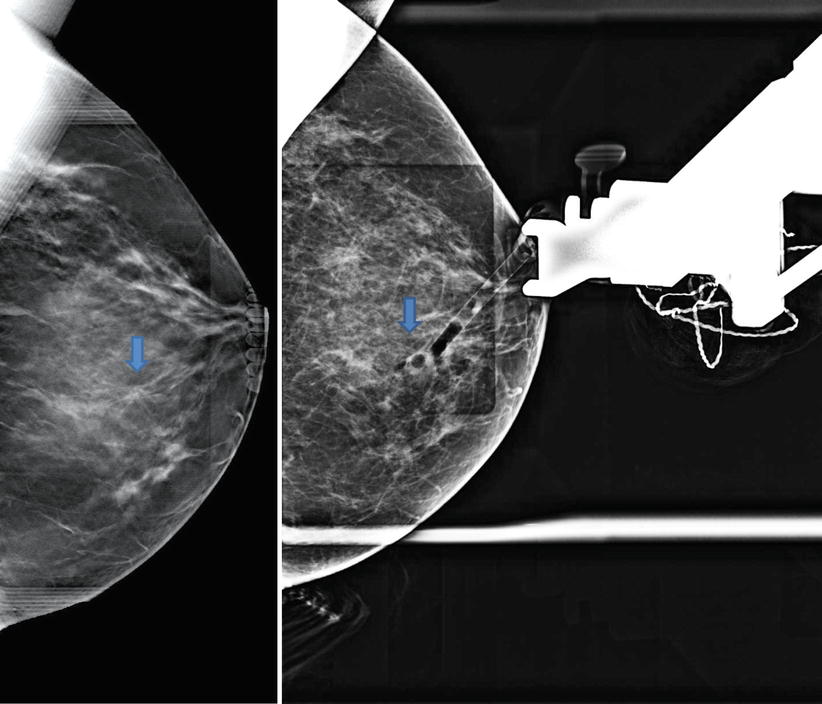
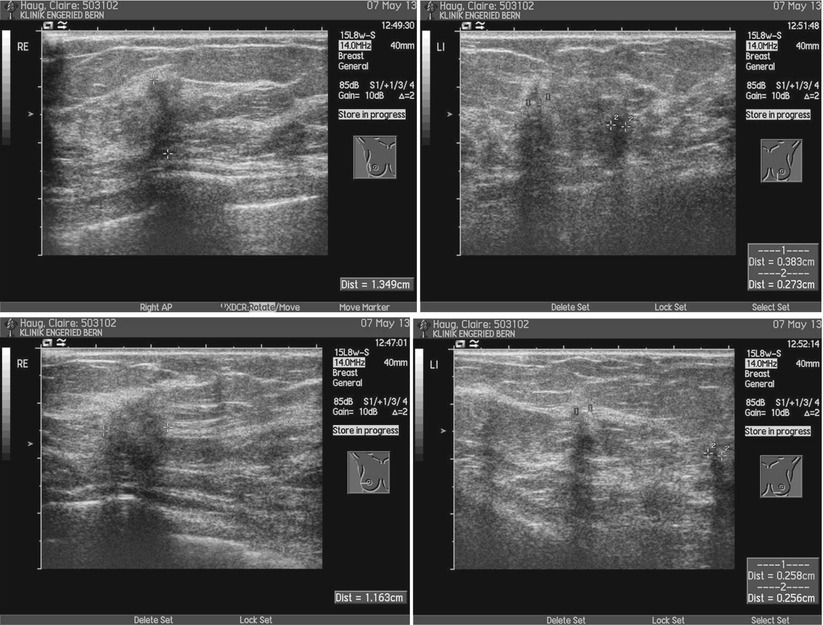
Fig. 8.15
US right and left
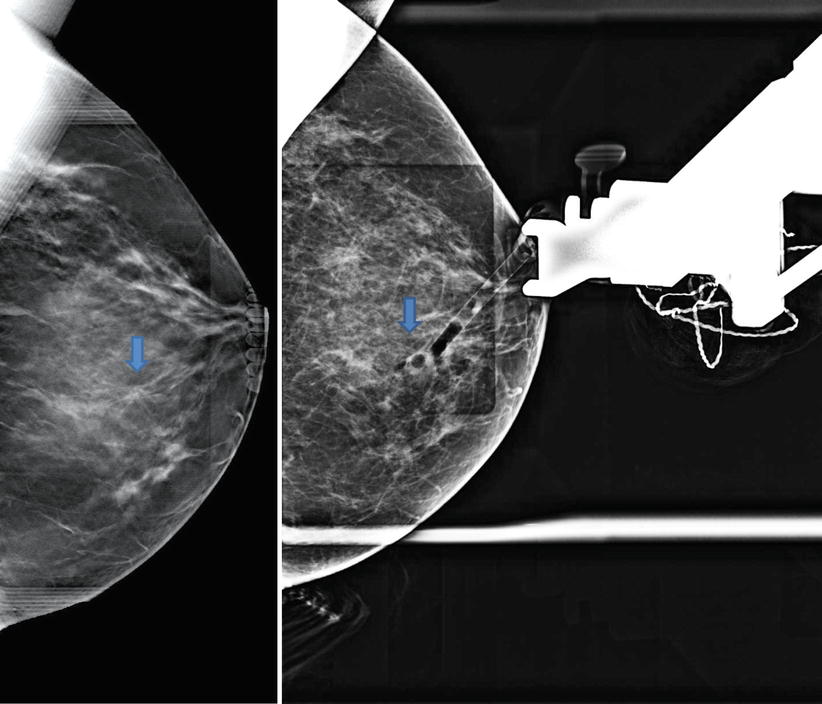
Fig. 8.16
T-VAB 3D Lcc localization of the target in upright position and 2D before clip positioning
Explanation
3D has a higher diagnostic accuracy than 2D; the newly detected radial lesions require histological confirmation.
Histology
Invasive ductal carcinoma, moderately differentiated, G2 on both sides.
Further Imaging/Further Diagnostic
MRI recommended.
Comment
Small (5 mm) radial lesions are difficult to find on a second-look US or they can be occult.
Image Interpretation Pearls
3D shows targets without tissue overlap and highlights radial lesions.
8.1.3 Case 3
General Information/Clinical Issues
Patient was a 71-year-old female, familial high-risk (mother and grandmother); in 2009 newly demarcated group of amorphous microcalcifications retroareolar right posterolateral – BI-RADS 4; S-VAB in 2009 unable to be performed due to subcutaneous location with large movability of the microcalcifications; on follow-up in 2010 right microcalcifications no longer distinguishable—previously artificial ?; in 2012 new progressive amorphous microcalcifications left centrocaudal – BI-RADS 4; histology after S-VAB sclerosed fibroadenoma; in 2013 T-VAB histology: invasive ductal breast carcinoma G2 (probably completely removed – 3 mm), postoperative histology pointed to different hormone receptors (progesterone >90 % preoperatively, 20–30 % postoperatively), re-examination of the 3D showed, retrospectively, a second, 4 mm lesion, cranial and closer to the chest wall.
Mammographic Analysis 2D, 2D (Synthetic), and 3D
Breast density ACR II. On 2D (2012) clip left side centrocaudal, no mass or distortion (Figs. 8.17a, b and 8.18a, b); BI-RADS 1. On 2D (synthetic) in 2013 no change compared with 2D in 2012 (Figs. 8.19a, b and 8.20a, b); BI-RADS 1. On 3D in 2013 radial distortion (3 mm) supramammillary right side (Figs. 8.21a, b, 8.22 and 8.23 3D magnification (same figure as 8.21a, b))); BI-RADS 4.
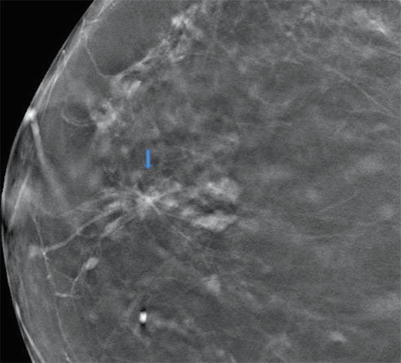
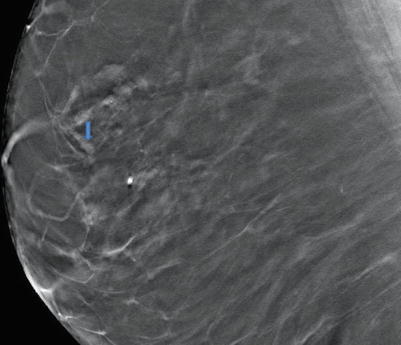
Fig. 8.17
(a, b) 2D Robl (a) and Lobl (b) in 2012
Fig. 8.18
(a, b) 2D Rcc (a) and Lcc (b) in 2012
Fig. 8.19
(a, b) 2D synthetic Robl (a) and Lobl (b) in 2013
Fig. 8.20
(a, b) 2D synthetic Rcc (a) and Lcc (b) in 2013
Fig. 8.21
(a, b) 3D Rcc (a) and Robl (b) in 2013
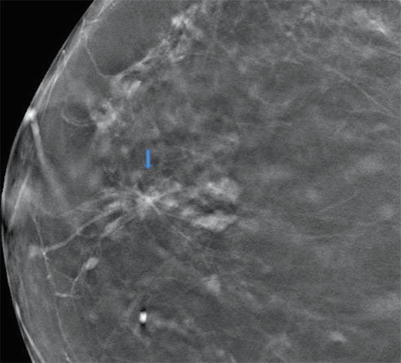
Fig. 8.22
3D Rcc magnification
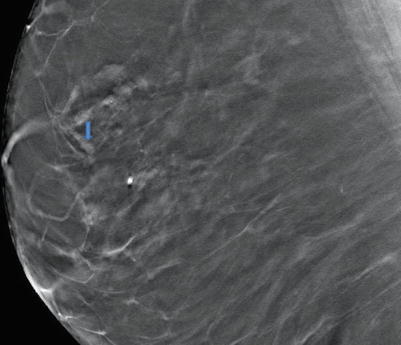
Fig. 8.23
3D Robl magnification
Recommendation
US with biopsy or T-VAB (Fig. 8.24); sometimes MRI can be a problem solver.
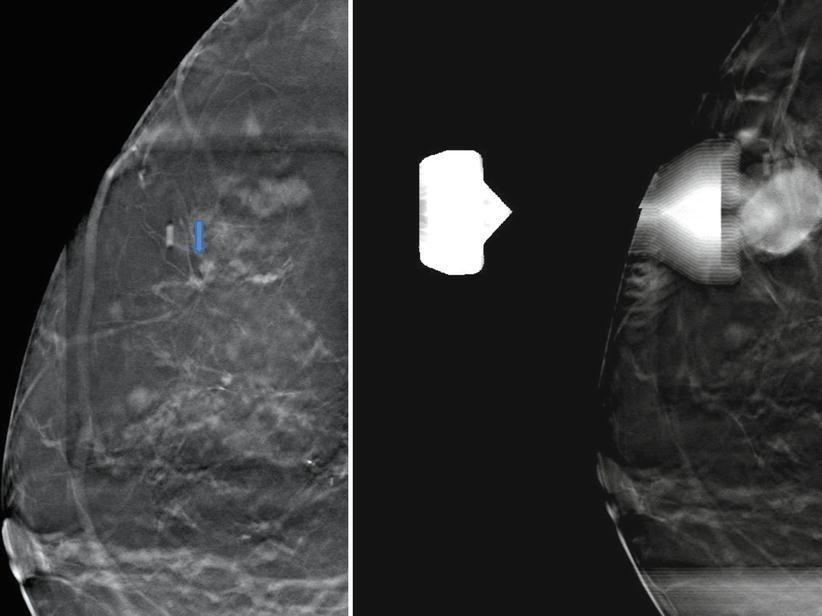
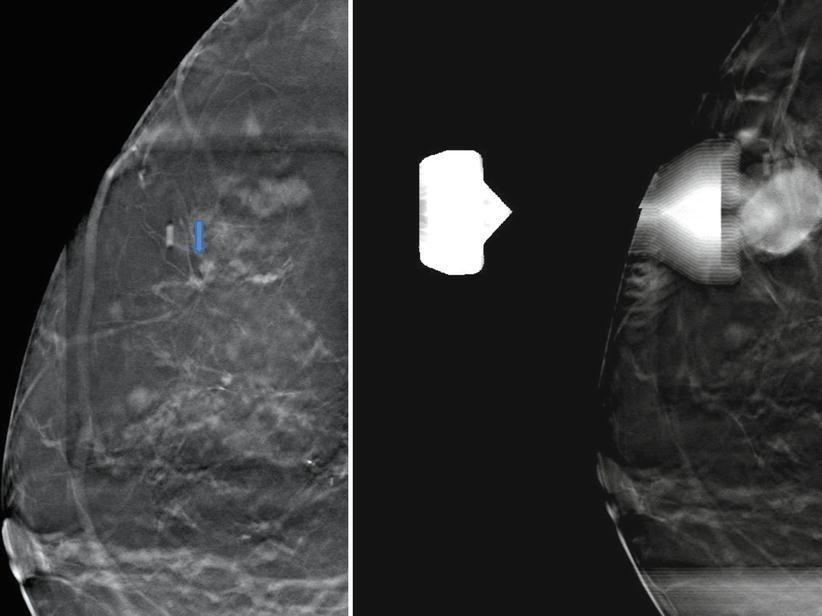
Fig. 8.24
T-VAB 3D Rml in decubitus position
US
External US occult.
Histology of T-VAB-Guided Biopsy
Invasive ductal breast carcinoma G2 (probably completely removed – 3 mm).
Postoperative Histology
Invasive ductal breast carcinoma G2, postoperative histology points to different hormone receptors (progesterone >90 % preoperatively, 20–30 % postoperatively) – > cannot be the same tumor as the one diagnosed preoperatively.
Explanation
Final Histology
Bifocal breast cancer.
Further Imaging/Further Diagnostic
MRI optional.
Comment
Small (5 mm) radial lesions are difficult to find on a second-look US or they can be occult, even very small lesions (3–4 mm) detected on 3D are easy to biopsy with T-VAB with high security; always look for second lesions, even retrospectively.
Image Interpretation Pearls
3D shows targets without tissue overlap and highlights radial lesions, even very small lesions are reproducible on T-VAB.
8.1.4 Case 4
General Information/Clinical Issues
Patient was a 48-year-old female, clustered amorphous microcalcifications on external mammogram; for the planning of the intervention (S-VAB), complementary 3D images are made in Rcc and Rml projections.
Mammographic Analysis 2D (Synthetic) and 3D
Breast density ACR II.On 2D (synthetic) the microcalcifications are centrocaudal, no depth determination is possible (Fig. 8.27a, b); BI-RADS 4. On the 3D Rcc projection the microcalcifications are directly subcutaneously close to the detector; therefore, an intervention in the upright position would be difficult; on the 3D Rml projection the calcifications are centrally located with enough distance from the skin and detector; therefore, an intervention in the decubitus position is easy to perform without problems (Fig. 8.28a, b) BI-RADS 4.
Fig. 8.27
(a, b) 2D synthetic Robl (a) and Rcc (b) in 2012
Fig. 8.28
(a, b) 3D synthetic Robl (a) and Rcc (b) in 2012
Conclusion/Diagnosis with 3D
(BI-RADS 4).
Recommendation
If only 2D is available, additional 3D should be created before an intervention.
US
No internal US.
Explanation
Histology
DCIS.
Further Imaging/Further Diagnostic
MRI optional.
Comment
3D shows distance of target to skin (cc, ml) and detector; knowing the accurate depth (cc, ml) means knowing the best pathway to access the target.
Image Interpretation Pearls
3D shows the exact location of the targets without tissue overlap.
MRI
Performed MRI showed non-mass enhancement lateral left side, histology of MRI-guided biopsy revealed diffuse adenosis, apocrine cysts, fibrosis, B2.
8.1.5 Case 5
General Information/Clinical Issues
Patient was a 56-year-old female, mastodynia.
Mammographic Analysis 2D, 2D (Synthetic), and 3D
Breast density ACR III. On 2D polymorphic clustered microcalcifications right side mediocaudal (Fig. 8.31a, b) BI-RADS 4; on 3D Rcc (Fig. 8.32a, b) a radial mass is detected, not visible even on spot compression view (Fig. 8.33); BI-RADS 5.
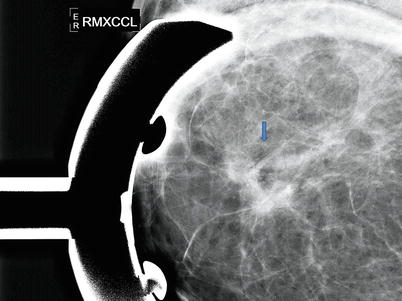
Fig. 8.31
(a, b) 2D Rcc (a) and Robl (b) in 2009
Fig. 8.32
(a, b) 3D Rcc and 3D magnification Rcc in 2009
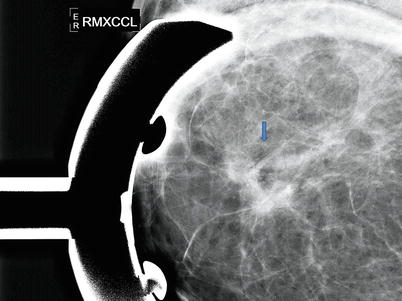
Fig. 8.33
2D Rcc spot compression view
Conclusion/Diagnosis with 3D
Highly suggestive of invasive breast cancer, not only possible DCIS (BI-RADS 5).
Recommendation
US with biopsy or S-VAB performed (05/09).
Explanation
Due to questionable sonographic correlating lesion, S-VAB is recommended, with higher safety to biopsy the right place, as well as to reduce the sampling error.
Histology of S-VAB
Apocrine metaplasia, intraductal papillomas, flat epithelial atypia (FEA), no DCIS (Fig. 8.35).
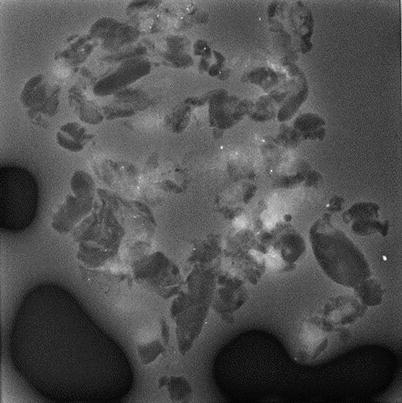
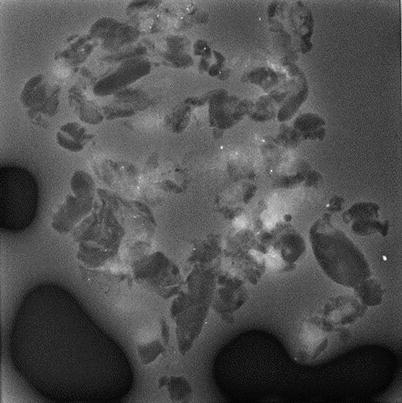
Fig. 8.35
S-VAB specimen
Postoperative Histology
Invasive ductal breast cancer.
Further Imaging/Further Diagnostic
MRI recommended.
Comment
3D reduces false-positives, 3D increases the sensitivity, and 3D increases the earlier detection of malignant lesions.
Image Interpretation Pearls
The diagnostic accuracy of 3D is at least equivalent to digital spot compression views.
8.1.6 Case 6
General Information/Clinical Issues
Patient was a 76-year-old female, follow-up under hormone replacement therapy.
Mammographic Analysis 2D Spot Compression View, 2D (Synthetic), and 3D
Breast density ACR II. 2D (synthetic) (Fig. 8.36a, b), 3D (Figs. 8.37a, b and 8.38 3D magnification (same figure as 8.37b)), and 2D spot compression view (Fig. 8.39) show a 6 mm architectural distortion lateral right side; BI-RADS 4.
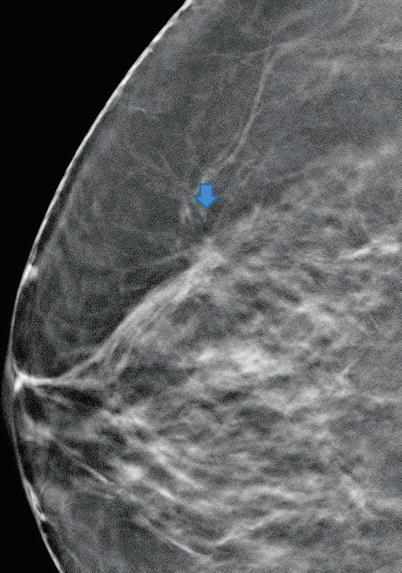
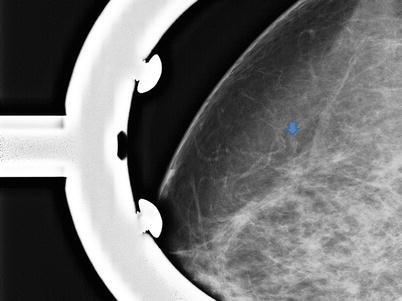
Fig. 8.36
(a, b) 2D synthetic Robl (a) and Rcc (b) in 2013
Fig. 8.37
(a, b) 3D Robl (a) and Rcc (b) in 2013
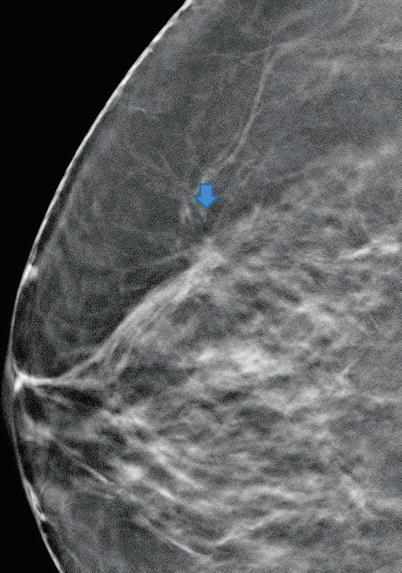
Fig. 8.38
3D Rcc magnification
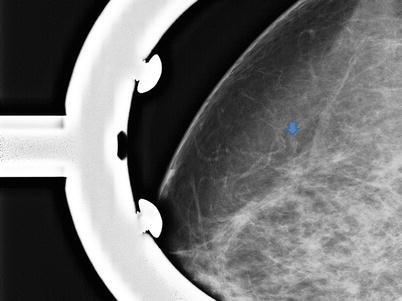
Fig. 8.39
2D Rcc spot compression view
Conclusion/Diagnosis with Spot View, 2D (Synthetic), and 3D
Suggestive of malignancy (BI-RADS 4).
Recommendation
US (with or without biopsy) or T-VAB.
US
Due to three small lateral hypoechoic lesions on US, the local association in the lateral aspect of the right breast were three small hypoechoic lesions in ultrasound, therefore, the detected radial lesion in 3D could not be assigned properly (Fig. 8.40); BI-RADS 0, T-VAB recommended.
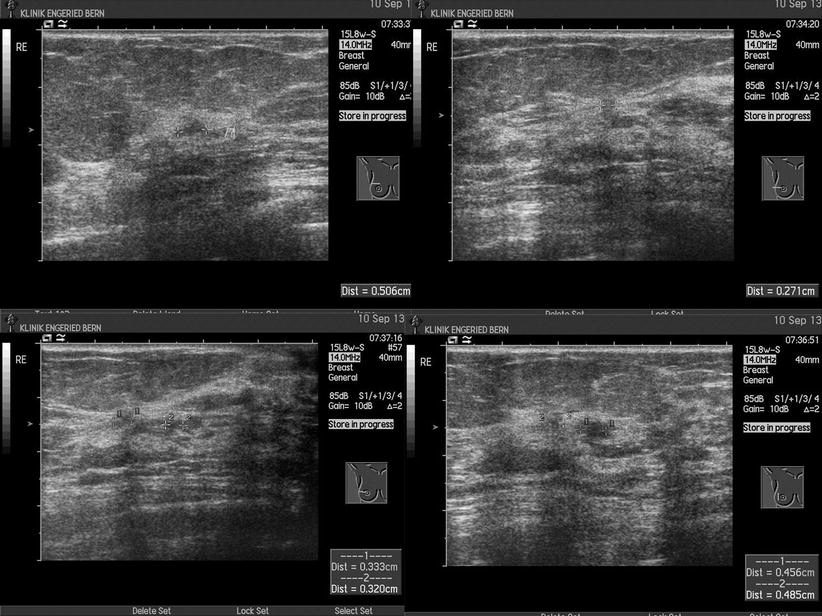
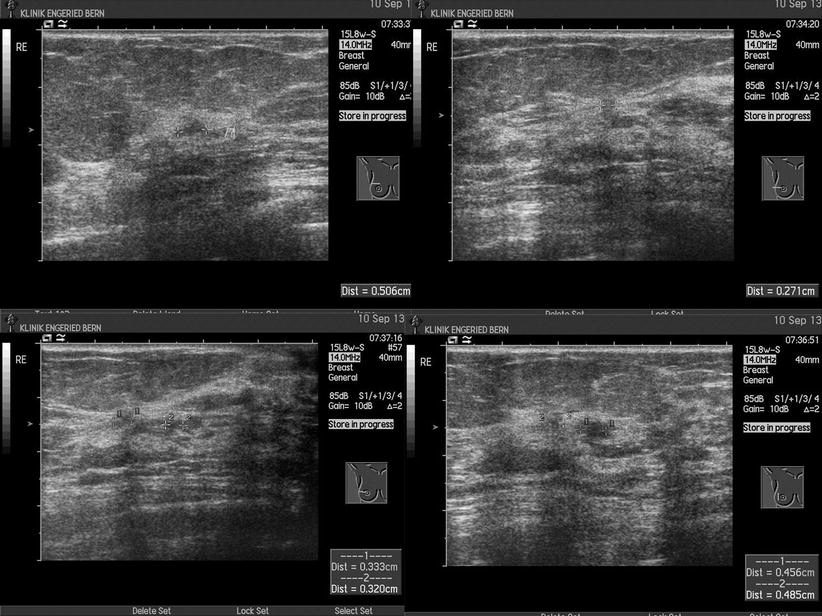
Fig. 8.40
US
Explanation
Relocalization of the small architectural distortion is possible with 3D without problems and is less time-consuming than US. T-VAB in decubitus position (Fig. 8.41) shows two arterial vessels in the immediate neighborhood of the architectural distortion; to avoid major bleeding the intervention is performed in the upright position (Fig. 8.42a, b). T-VAB is helpful in planning of the intervention.
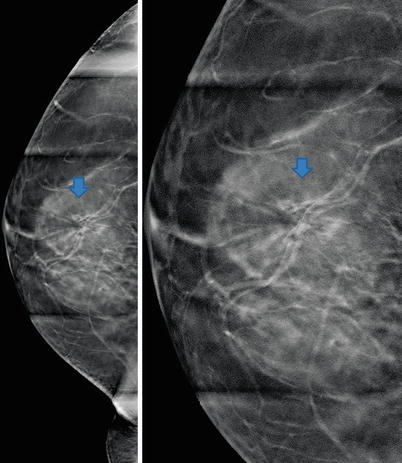
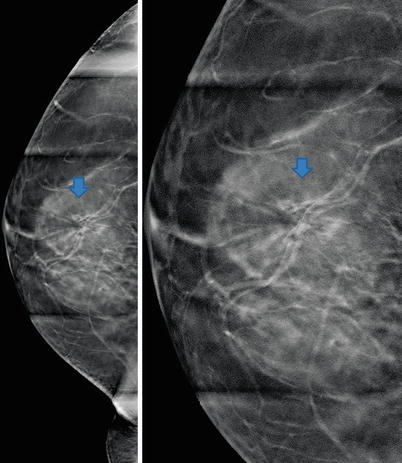
Fig. 8.41
T-VAB Rml in decubitus position
Fig. 8.42
(a, b) T-VAB Rcc in upright position
Histology After T-VAB
Radial scar, sclerosing adenosis, fibrosis, usual ductal hyperplasia (UDH), B3.
Further Imaging/Further Diagnostic
No MRI recommended (ACR II and small lesion).
Comment
We can plan the intervention in advance (access from cranial, lateral, or medial) with high safety.
Image Interpretation Pearls
3D shows the exact location of the targets without tissue overlap; any problems with arterial vessels can be detected in time.
8.1.7 Case 7
General Information/Clinical Issues
Patient was a 56-year-old female.
Mammographic Analysis 2D, 2D (Synthetic), and 3D
Breast density ACR III. On 2D and 2D (synthetic) no mass or distortion visible (Fig. 8.43a, b and 8.44a, b); BI-RADS 1. On 3D a small 5 mm architectural distortion is detected, mediocaudal left side (Figs. 8.45a, b, 8.46, and 8.47 3D magnification (same figure as 8.45a, b)); BI-RADS 4.
Fig. 8.43
(a, b) 2D Lobl (a) and Lcc (b) in 2012
Fig. 8.44
(a, b) 2D synthetic Lobl (a) and Lcc (b) in 2012
Fig. 8.45
(a, b) 3D Lobl (a) and Lcc (b) in 2012
Fig. 8.46
3D magnification Lcc
Fig. 8.47
3D magnification Lobl
Conclusion/Diagnosis with 3D
On 2D S-VAB, the radiating distortion cannot be located and is masked by dense glandular tissue (Fig. 8.48a, b); on 3D T-VAB, the lesion is easily localized again and the intervention can be performed (Fig. 8.49a, b).
Fig. 8.48
(a, b) 2D Lml stereotactic pair
Fig. 8.49
(a, b) T-VAB Lcc localization of target (a) and inserted clip after vacuum-assisted biopsy (b)
Recommendation
US with biopsy or T-VAB; sometimes MRI can be a problem solver.
US
No clear assignment of mammographically detected lesion (images); BI-RADS 2.
Explanation
Before 3D T-VAB all lesions not localizable on 2D S-VAB had to be submitted to time-consuming MRI and MRI-guided biopsy, with higher costs.
Histology
At least B4, highly suggestive of invasive breast cancer.
Further Imaging/Further Diagnostic
MRI recommended.
Comment
We are now able to biopsy lesions detected only with tomosynthesis – mainly small radial lesions.
Image Interpretation Pearls
3D shows the exact location of the target without tissue overlap and highlights radial lesions.
8.1.8 Case 8
General Information/Clinical Issues
Patient was a 68-year-old female, screening, follow-up.
Mammographic Analysis 2D and 3D
Breast density ACR III. On 2D follow-up (Figs. 8.50a, b and 8.51a, b) and 3D (Fig. 8.52a, b) progressive polymorphic microcalcifications right central caudal; BI-RADS 4.
Fig. 8.50
(a, b) 2D Rcc (a) and Robl (b) in 2008
Fig. 8.51
(a, b) 2D Rcc (a) and Robl (b) in 2010
Fig. 8.52
(a, b) 3D Robl and 3D magnification in 2010
Conclusion/Diagnosis with 3D
The immediately subcutaneous location of microcalcifications can be seen only on 3D, suggestive of malignancy (BI-RADS 4).
Recommendation
US with biopsy or S-VAB.
Explanation
At this time (2010) we had an upright system; no T–VAB was available. With the calculated parameters (compression of the breast 33 mm, depth z-axis 33 mm) of the 2D S-VAB system (Fig. 8.54), an intervention appeared impossible. 3D showed (Fig. 8.55a, b) that the microcalcifications were 8–10 mm away from the skin. We tried an intervention with the following advice: − put a depot with local anesthesia between the skin and the microcalcifications; due to the insufficient distance of the needle in the pre-fire position to the detector, the needle needs to be withdrawn before firing; fire the needle at a sufficient distance to the detector; after correct position (manually in post-fire position) of the needle, abolish the breast compression completely; due to the reduced compression the lesion is now near the needle chamber.
Fig. 8.54
2D stereotactic pairs in upright position
Fig. 8.55
(a, b) 3D Rcc with scale
Histology S-VAB
DCIS.
Postoperative Histology
Extension of disease was significantly underestimated by imaging; multifocal DCIS, R1.
Further Imaging/Further Diagnostic
MRI optional.
Comment
S-VAB is occasionally required for the clarification of focal lesions; stereotactic calculation of the focal depth of the lesion is often problematic; with lesions close to the detector, access may be impossible; an option is the manual entry of the needle, in post-fire position, to the calculated z-axis.
Image Interpretation Pearls
3D shows the exact location of the targets; 3D planning of the intervention can be very helpful.
8.1.9 Case 9
General Information/Clinical Issues
Patient was a 72-year-old female, family history of breast cancer (sister), hormone replacement therapy.
Mammographic Analysis 2D and 3D
Breast density ACR III. On 2D (2009) may be “slight architectural disturbance”, stable compared with priors (2007) on right side laterocranial (Figs. 8.56a, b and 8.57a, b); BI-RADS 0. On 3D in 2010 the lesion is an obvious 7 mm architectural distortion compared with 2D (Figs. 8.58a, b); BI-RADS 4.