and Christian Waldherr1
(1)
Bern, Switzerland
6.1 Malignant Changes: Ductal Carcinoma in Situ (DCIS)
6.1.1 Case 1
General Information/Clinical Issues
Patient was a 62-year-old female. cT0 N0, previous history of benign surgical biopsy left side laterocranial (papilloma).
Mammographic Analysis 2D and 2D (Synthetic) and 3D
2D in 2011 (Fig. 6.1a, b) and 2D synthetic in 2013 (Fig. 6.2a, b) show a slowly growing well-circumscribed 5 mm mass (Figs. 6.1a, b and 6.2a, b) laterocranial close to the subcutis. Mass in only one view on 2D synthetic Lobl and 3D Lobl (Figs. 6.2a, 6.3a, 6.4, and 6.5 [3D magnification, same figure as 6.2a and 6.3a]) hyperdense, no associated microcalcifications; ultrasound (US) recommended (BI-RADS 0).
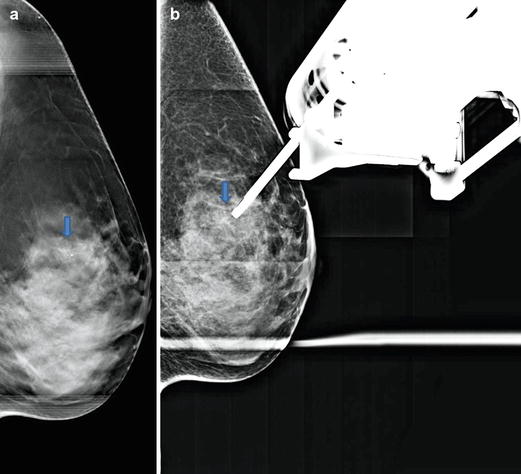
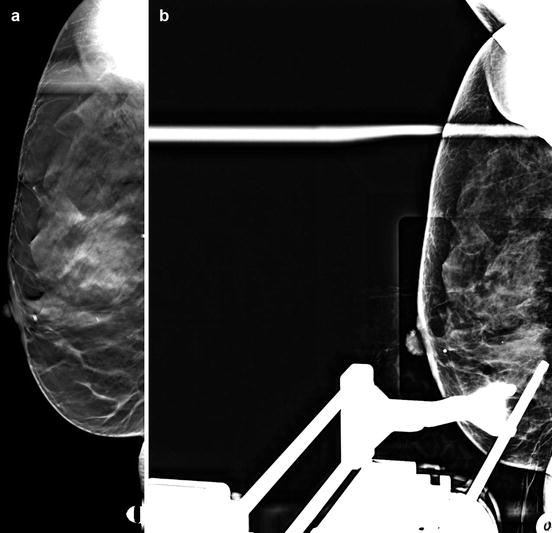
Fig. 6.1
(a, b) 2D Lobl (a) and Lcc (b) in 2011
Fig. 6.2
(a, b) 2D synthetic Lobl (a) and Lcc (b) in 2013
Fig. 6.3
(a, b) 3D Lobl (a) and Lcc (b) in 2013
Fig. 6.4
3D magnification Lobl
Fig. 6.5
3D magnification Lcc
Differential Diagnosis on 2D
Cyst, fibrocystic changes, atypical ductal hyperplasia (ADH), atypical lobular hyperplasia (ALH), lobular carcinoma in situ (LCIS), fibroadenoma, papilloma, lymph node, mucinous or papillary carcinoma, DCIS, invasive ductal carcinoma (IDC).
Conclusion/Diagnosis with 3D
No advantage compared with 2D and 2D synthetic in this case.
Recommendation
Rule out malignancy with ultrasound (US), especially if the mass is hyperdense (BI-RADS 0); 10 % of DCIS is manifested as a mass .
US
Vertically oriented well-circumscribed lesion hypoechoic at 1 o’clock near the subcutis (Fig. 6.6).
Fig. 6.6
US in 2014
Histology
DCIS, low differentiated, G3.
Further Imaging/Further Diagnostic
No magnetic resonance imaging (MRI) recommended.
6.1.2 Case 2
General Information/Clinical Issues
Patient was a 47-year-old female.
Mammographic Analysis 2D (Synthetic) and 3D
Compared withwith priors: 2D (synthetic) and 3D (Figs. 6.7a, b, 6.8a, b, and Fig. 6.11 [3D magnification, same figure as 6.8a]) in 2012 show progressive clustered macrocalcifications (morphologically more likely benign appearance) and fine powdery microcalcifications (indistinct, amorphous) laterocaudal left side on 2D (synthetic) and 3D (Figs. 6.9a, b, 6.10a, b, and 6.12 [3D magnification, same figure as 6.10a]), no associated mass; BI-RADS 4.
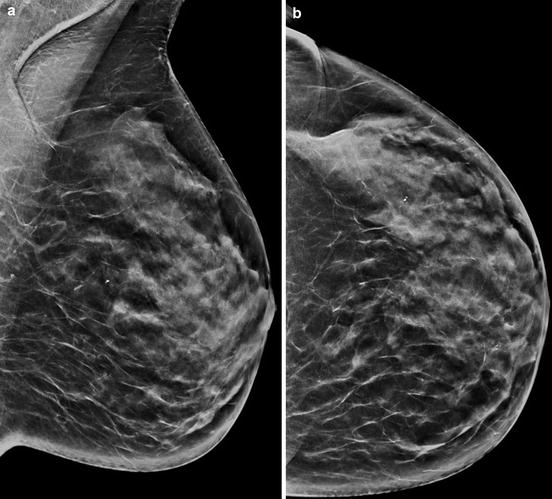
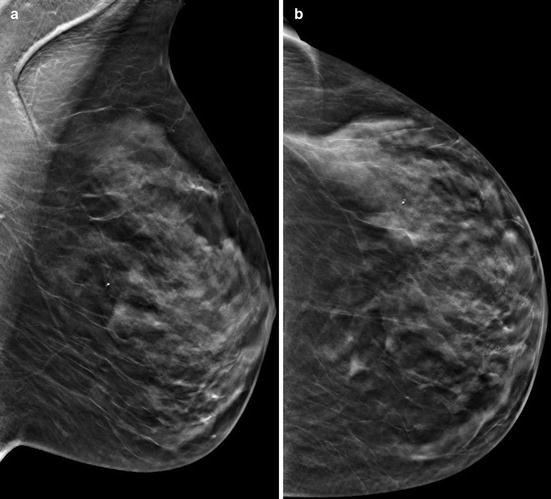
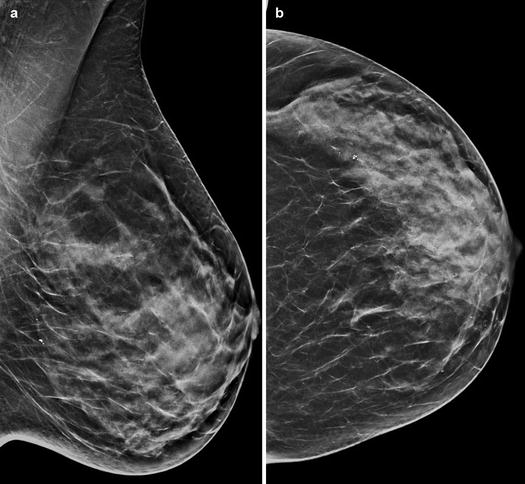
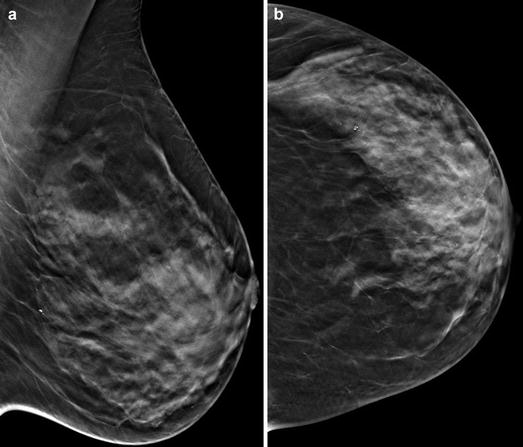
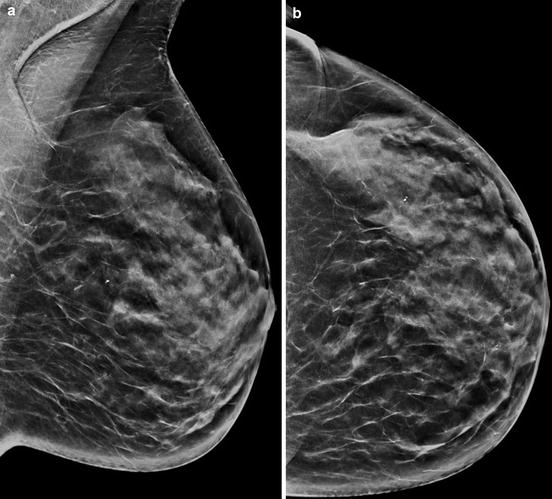
Fig. 6.7
(a, b) 2D synthetic Lobl (a) and Lcc (b) in 2012
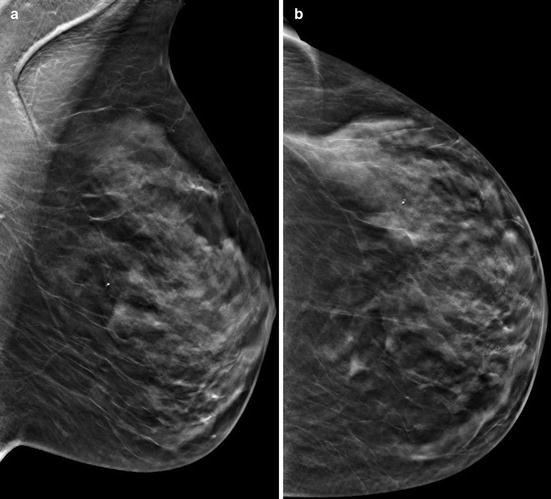
Fig. 6.8
(a, b) 3D Lobl (a) and Lcc (b) in 2012
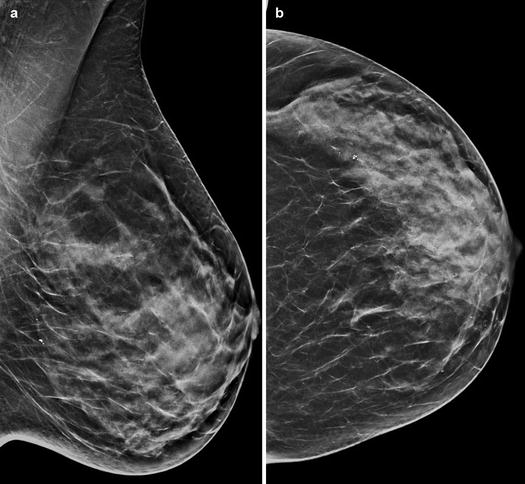
Fig. 6.9
(a, b) 2D synthetic Lobl (a) and Lcc (b) in 2014
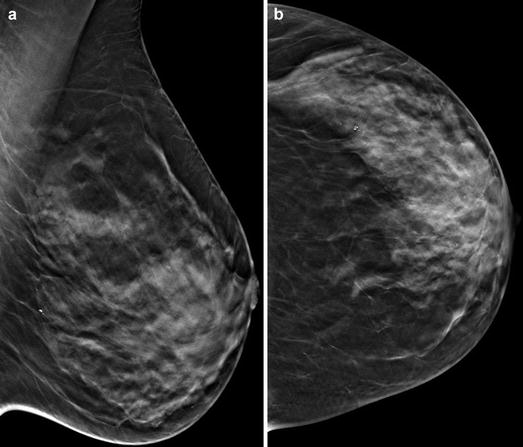
Fig. 6.10
(a, b) 3D Lobl (a) and Lcc (b) in 2014
Fig. 6.11
3D magnification Lcc in 2012
Fig. 6.12
3D magnification Lcc in 2014
Differential Diagnosis on 2D (Synthetic)
Cyst, fibrocystic changes, ADH, ALH, LCIS, fibroadenoma, papilloma, lymph node, mucinous or papillary carcinoma, DCIS, IDC.
Conclusion/Diagnosis with 3D
No advantage compared with 2D (synthetic) and 2D spot view (Fig. 6.13) in this case, suggestive of malignancy (BI-RADS 4).
Fig. 6.13
Spot view Lcc in 2014
Recommendation
US-guided biopsy or S-vacuum-assisted biopsy (S-VAB) or tomosynthesis guided vacuum-assisted biopsy (T-VAB) biopsy recommended.
US
−
Histology
DCIS with comedo necrosis, low differentiated, G3.
Further Imaging/Further Diagnostic
MRI optional.
6.1.3 Case 3
General Information/Clinical Issues
Patient was a 66-year-old female, breast cancer in left breast in 2002.
Mammographic Analysis 2D and 3D
Linearly arranged (group of four) monomorphic microcalcifications mediocranial, difficult to detect on 2D (Figs. 6.14a, b and 6.15), more obvious on 3D (Fig. 6.16a, b), casting-type calcifications, no mass; BI-RADS 4.
Fig. 6.14
(a, b) 2D Rcc (a) and Robl (b) in 2013
Fig. 6.15
2D magnification Robl
Fig. 6.16
(a, b) 3D Robl (a) and 3D magnification Robl (b)
Differential Diagnosis on 2D
Fibrocystic change, papilloma, fat necrosis, or DCIS.
Conclusion/Diagnosis with 3D
No advantage compared with 2D in this case, suggestive of malignancy (BI-RADS 4).
Recommendation
US
No internal US.
Histology
DCIS, moderately differentiated.
Further Imaging/Further Diagnostic
No MRI recommended.
MRI
6.1.4 Case 4
General Information/Clinical Issues
Patient was a 65-year-old female; progressive microcalcifications on mammograms, asymptomatic.
Mammographic Analysis 2D (Synthetic) and 3D
Differential Diagnosis on 2D (Synthetic) and 3D
DCIS.
Conclusion/Diagnosis with 3D
Recommendation
US, or S-VAB or T-VAB biopsy (Fig. 6.22a, b).
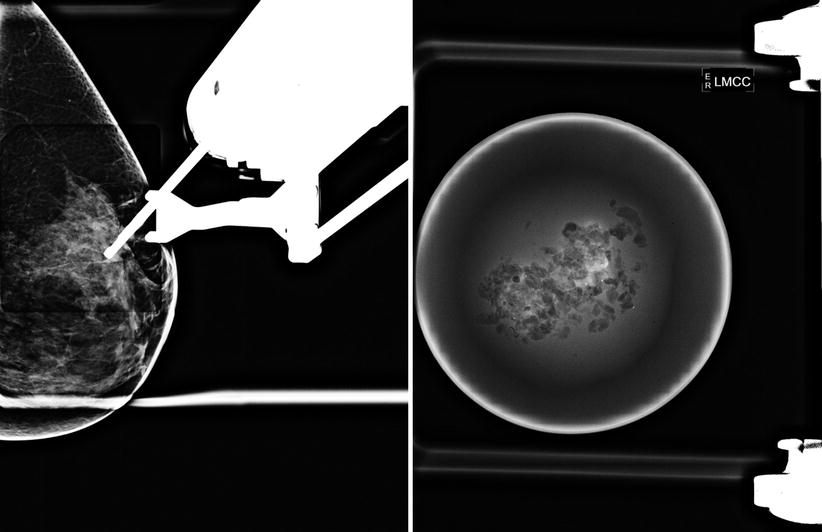
Fig. 6.22
(a, b) 3D T-VAB Rml (a) and Rml after intervention (b)
US
No internal US.
Histology
DCIS, degree of differentiation G3.
Further Imaging/Further Diagnostic
MRI recommended, look for expansion.
6.1.5 Case 5
General Information/Clinical Issues
Patient was a 66-year-old female, asymptomatic.
Mammographic Analysis 2D (Synthetic) and 3D
Breast density ACR I. Nonspecific density on Lcc 2D (synthetic) lateral without calcification; BI-RADS 1 (Fig. 6.24a, b). On 3D there was a dense 8 mm lesion causing architectural distortion (Fig. 6.25a, b); BI-RADS 4.

Fig. 6.24
(a, b) 2D synthetic Lobl (a) and Lcc (b) in 2013

Fig. 6.25
(a, b) 3D Lobl (a) and Lcc (b) in 2013
Differential Diagnosis on 2D (Synthetic) and 3D
Radial scar, DCIS, or invasive breast cancer.
Conclusion/Diagnosis with 3D: 3D
Advantage compared with 2D (synthetic) in this case; on 3D the lesion is suggestive of malignancy (BI-RADS 4); 10 % of DCIS is manifested as a mass without calcifications (non-mass-like lesion).
Recommendation
US or S-VAB or T-VAB biopsy (Fig. 6.26a, b).
Fig. 6.26
(a, b) 3D Lml localization for T-VAB and magnification
US
No internal US.
Histology
DCIS, low differentiated, G3.
Further Imaging/Further Diagnostic
No MRI recommended (ACR I).
6.1.6 Case 6
General Information/Clinical Issues
Patient was a 54-year-old female. Screening.
Mammographic Analysis 2D (Synthetic) and 3D
Breast density ACR IV. Compared with priors in 2010 (Figs. 6.27a, b and 6.28a, b), with scattered calcifications on both sides, progressive clustered crushed-stone-like microcalcifications central near chest wall on the left side. 2D (synthetic) and 3D, no associated mass (Figs. 6.29a, b, 6.30a, b and 6.31 [3D magnification, same figure as 6.30b]); BI-RADS 4.
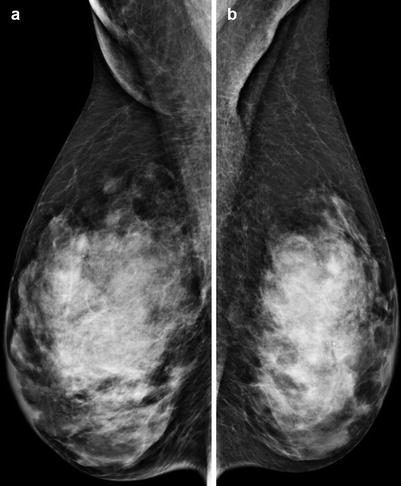
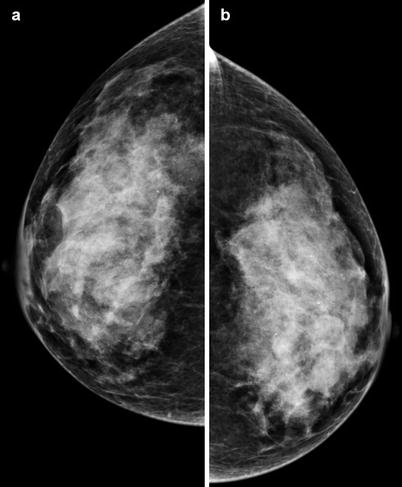
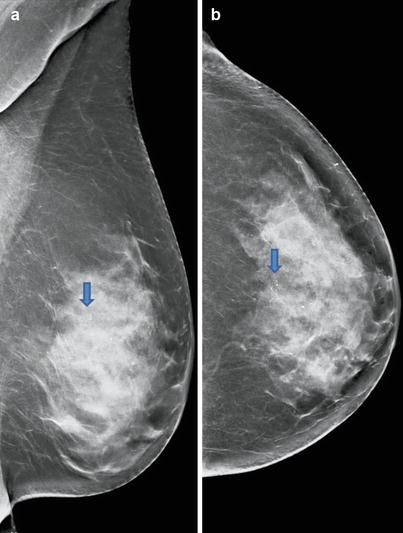
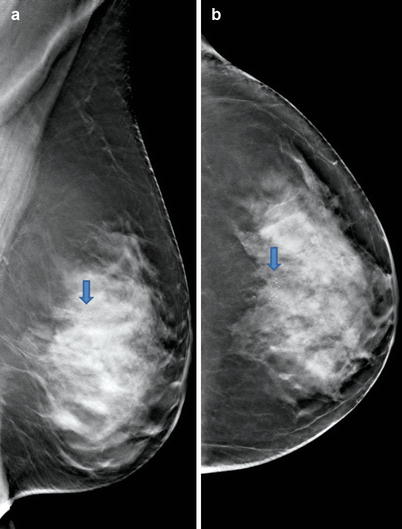
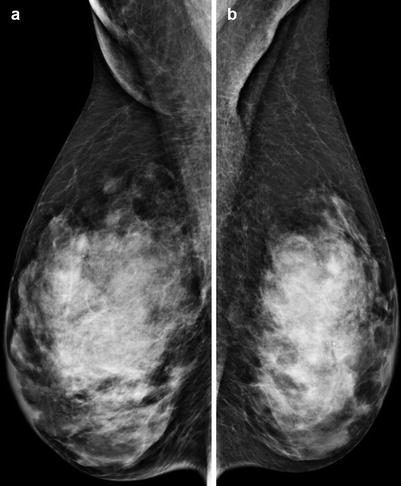
Fig. 6.27
(a, b) 2D Robl (a) and Lobl (b) in 2010
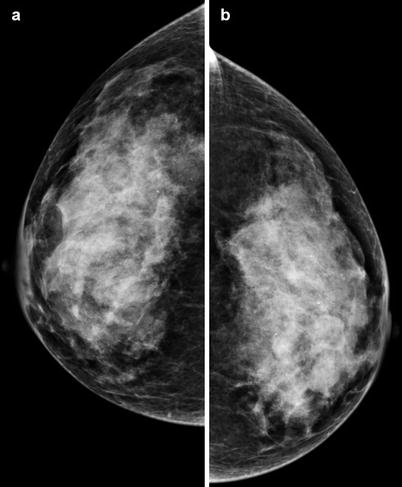
Fig. 6.28
(a, b) 2D Rcc (a) and Lcc (b) in 2010
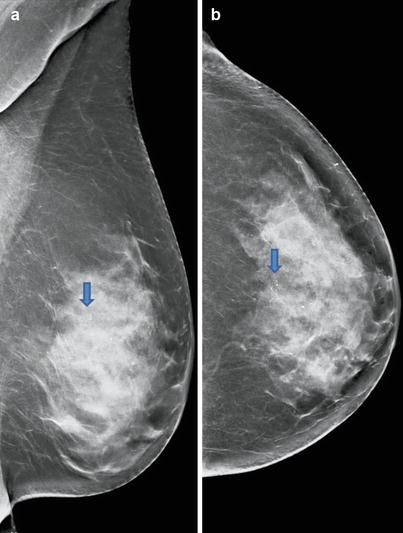
Fig. 6.29
(a, b) 2D synthetic Robl (a) and Rcc (b) in 2014
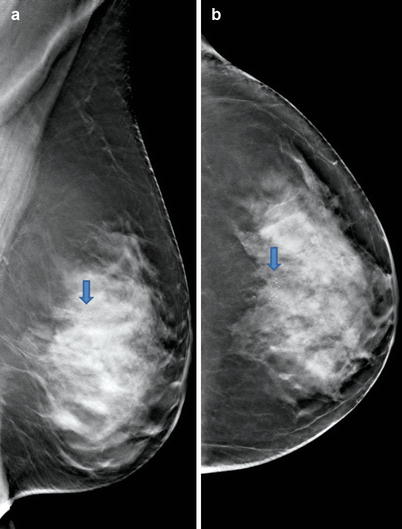
Fig. 6.30
(a, b) 3D Robl (a) and Rcc (b) in 2014
Fig. 6.31
3D magnification Lcc
Differential Diagnosis on 2D (synthetic)
Cyst, fibrocystic changes, ADH, ALH, LCIS, fibroadenoma, papilloma, lymph node, mucinous or papillary carcinoma, DCIS, IDC.
Conclusion/Diagnosis with 3D
No advantage compared with 2D (synthetic) in this case, suggestive of malignancy (BI-RADS 4).
Recommendation
US
No internal US.
Histology After S-VAB
DCIS, G3.
Further Imaging/Further Diagnostic
MRI recommended (ACR IV).
MRI
Performed with diffuse background enhancement on both sides, difficult to distinguish from DCIS (Fig. 6.33).
Fig. 6.33
MRI
6.1.7 Case 7
General Information/Clinical Issues
Patient was a 63-year-old female; painful area caudolateral right.
Mammographic Analysis 2D and 3D
Breast density ACR III; extensive casting-type calcifications, linearly arranged; grouped pleomorphic microcalcifications laterocentral right side 2D (Figs. 6.34a, b and 6.35a, b) and 3D (Fig. 6.36a, b), no associated mass; BI-RADS 5.

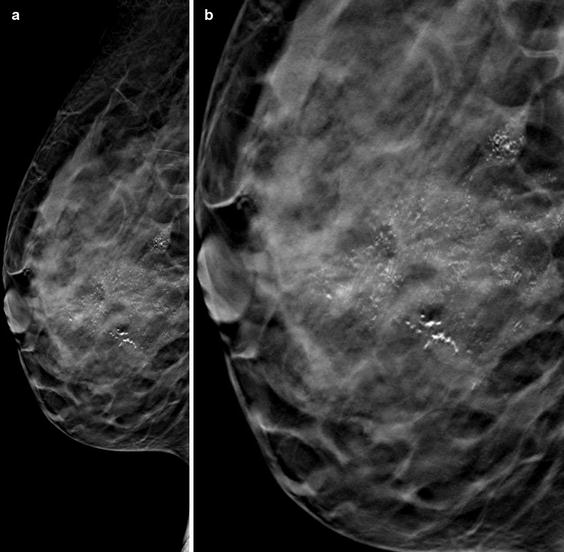

Fig. 6.34
(a, b) 2D Robl (a) and Lobl (b) in 2009
Fig. 6.35
(a, b) 2D Robl (a) and Lobl (b) in 2009
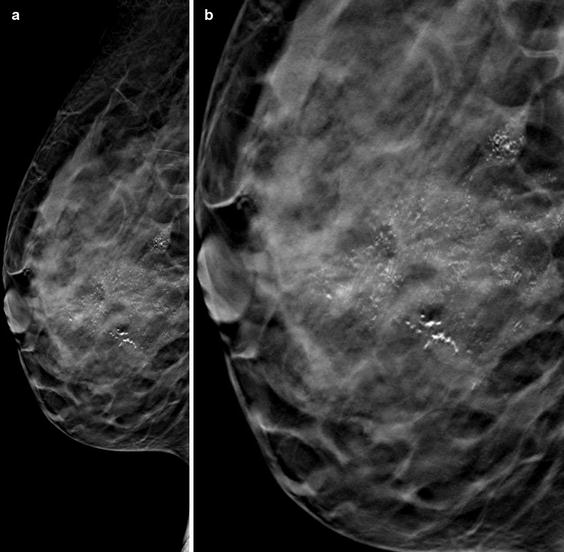
Fig. 6.36
(a, b) 3D Rcc (a) and 3D magnification Rcc (b)
Differential Diagnosis on 2D
DCIS, invasive cancer.
Conclusion/Diagnosis with 3D
No advantage compared with 2D in this case, 2D and 3D highly suggestive of malignancy (BI-RADS 5).
Recommendation
US-guided biopsy.
US
Hypoechoic irregular inhomogeneous area with multiple hyperechoic foci representing DCIS (Fig. 6.37).


Fig. 6.37
US
Histology
DCIS, multicentric low differentiated, G3.
Further Imaging/Further Diagnostic
MRI recommended (ACR III); look for expansion.
MRI
Performed with typical non-mass enhancement (5.5 cm), multicentric in upper outer and lower outer quadrants (Fig. 6.38).
Fig. 6.38
MRI
6.1.8 Case 8
General Information/Clinical Issues
Patient was a 70-year-old female; hormone replacement therapy (HRT), T0N0.
Mammographic Analysis 2D and 2D (Synthetic) and 3D
Breast density ACR III. Compared with priors in 2010 (Fig. 6.39a, b), with progressive casting-type calcification, linearly arranged; grouped pleomorphic microcalcifications (morphologically similar to plasmacell mastitis) lateral and medial on the left side. 2D (Fig. 6.40a, b) and 3D (Fig. 6.41a, b), no associated mass. On 2D (synthetic) microcalcifications are strengthened and thus are more visible than on 2D and 3D (Fig. 6.42a, b); BI-RADS 4.
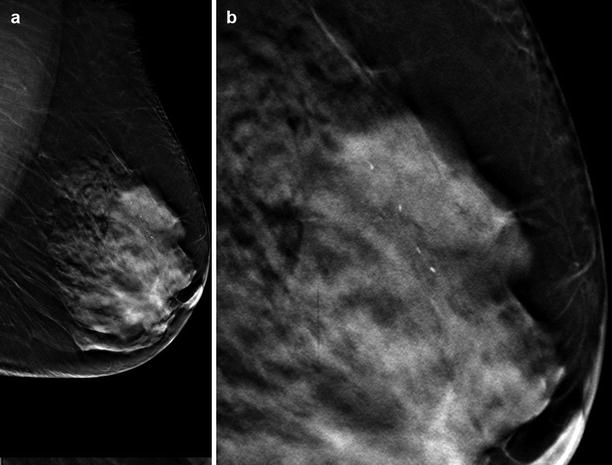
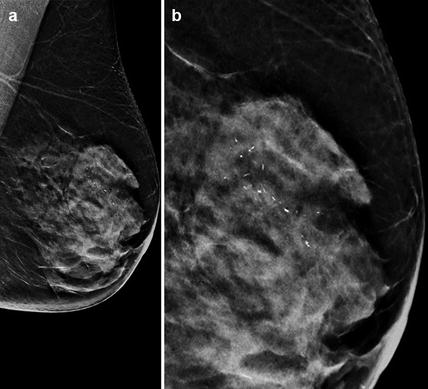
Fig. 6.39
(a, b) 2D Lcc (a) and Lobl (b) in 2010
Fig. 6.40
(a, b) 2D Lcc (a) and Lobl (b) in 2012
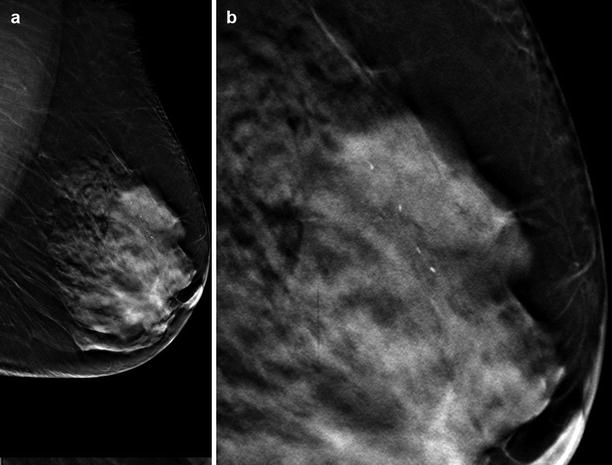
Fig. 6.41
(a, b) 3D Robl (a) in 2012 and 3D magnification (b)
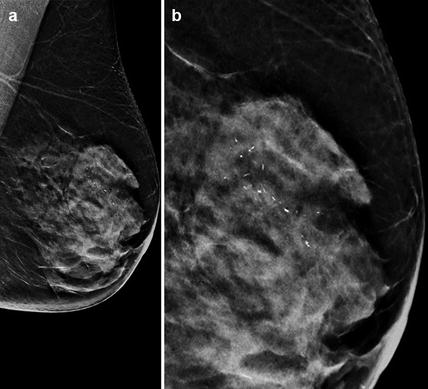
Fig. 6.42
(a, b) 2D synthetic Robl (a) in 2012 and 2D Robl synthetic magnification (b)
Fig. 6.43
US
Differential Diagnosis on 2D and 2D (Synthetic)
Plasmacell mastitis, papilloma, DCIS.
Conclusion/Diagnosis with 3D
No advantage compared with 2D in this case, suggestive of malignancy (BI-RADS 4).
Histology
DCIS left side, invasive breast cancer right side was detected on MRI at 12 o’clock position (2D images).
Further Imaging/Further Diagnostic
MRI recommended (ACR III); look for expansion.
MRI
Performed with detection of an additional contralateral breast cancer on the right side at 12 o’clock position, no 3D on right side.
6.1.9 Case 9
General Information/Clinical Issues
Patient was a 54-year-old female, asymptomatic.
Mammographic Analysis 2D (Synthetic) and 3D
Breast density ACR I; segmentally distributed crushed stone -like calcifications, pleomorphic microcalcifications laterocranial left side. 2D (synthetic) (Fig. 6.45a, b) and 3D (Figs. 6.46a, b and 6.47 [3D magnification, same figure as 6.46a]), no associated mass; BI-RADS 5.
Fig. 6.45
(a, b) 2D synthetic Robl (a) and Rcc (b) in 2013
Fig. 6.46
(a, b) 3D Robl (a) and Rcc (b) in 2013
Fig. 6.47
3D Lobl magnification
Differential Diagnosis on 2D (Synthetic)
DCIS, invasive cancer.
Conclusion/Diagnosis with 3D
No advantage compared with2D (synthetic) in this case; 2D (synthetic) and 3D highly suggestive of malignancy (BI-RADS 5).
Recommendation
S-VAB or T-VAB biopsy.
US
No internal US.
Histology
DCIS, moderately differentiated, G2.
Further Imaging/Further Diagnostic
No MRI recommended (ACR I).
6.1.10 Case 10
General Information/Clinical Issues
Patient was a 52-year-old female; breast cancer left side in 2000 and DCIS right side in 2003; with breast-conserving therapy, annual control, follow-up with 2D (synthetic).
2D (Synthetic) and 3D Mammographic Analysis
Breast density ACR III; progressive linear segmentally oriented calcifications centrocaudal right side close to the chest wall on 2D (synthetic) (Figs. 6.48a, b and 6.49a, b) and 3D (Figs. 6.50a, b, 6.51 and 6.52 [3D magnification, same figure as 6.50a, b]), no associated mass; BI-RADS 4.

Fig. 6.48
(a, b) 2D synthetic Robl (a) and Lobl (b) in 2013
Fig. 6.49
(a, b) 2D synthetic Rcc (a) and Lcc (b) in 2013
Fig. 6.50
(a, b) 3D Rcc (a) and Robl (b) in 2013
Fig. 6.51
3D magnification Rcc

Fig. 6.52
3D magnification Robl
Differential Diagnosis on 2D (synthetic)
Cyst, fibrocystic changes, ADH, ALH, LCIS, fibroadenoma, papilloma, lymph node, mucinous or papillary carcinoma, DCIS, IDC.
Conclusion/Diagnosis
With 3D no advantage compared with 2D (synthetic) in this case; 2D (synthetic) and 3D suggestive of malignancy (BI-RADS 4).
Recommendation
US
No internal US.
Histology
DCIS, G3.
Further Imaging/Further Diagnostic
MRI recommended (ACR III); not performed.
Comment
The basis for the analysis of microcalcifications is the detection of the same. This, in turn, depends on the mammography equipment used (c-view) and on the density of the glandular tissue. The next step is the analysis of the distribution and the shape of the microcalcifications. Secondary is the size, the density, and the number of microcalcifications. Grouped microcalcifications are not a domain of US, in our opinion. Microcalcifications are easier to detect on 2D than subtle lesions causing radial distortions; 3D is very helpful in detecting these lesions; many of these lesions represent small invasive cancers, and finding a small invasive cancer has a much higher benefit than finding a DCIS.
Image Interpretation Pearls
Fine linear branching casting-type calcifications and segmental distribution along the milk ducts → high grade in situ G3/G2, pleomorphic heterogeneous, crushed stone-like calcifications → characteristic of G2 in situ carcinoma, amorphous indistinct calcifications → G1 in situ carcinoma located in the terminal ductal lobular units. These intralobular calcifications lead to significant differential diagnostic difficulties with low specificity, due to their morphology being similar to that of the calcifications of benign changes (differential diagnosis – see above).
6.2 Malignant Changes: Invasive Ductal Carcinoma (IDC)
6.2.1 Case 1
General Information/Clinical Issues
Patient was a 55-year-old female; FNA or FNAC 2004 right side, asymptomatic, no familial history.
Mammographic Analysis on 2D (Synthetic) and 3D
Breast density ACR III; 9 mm stellate mass with single fine monomorphic calcification located in the edge region at the 12 o’clock position right side, equal on 2D (synthetic) and 3D (Figs. 6.54a, b, 6.55a, b, 6.56, and 6.57 [3D magnification, same figure as 6.55a, b]), radial lesions are highlighted in the reconstructed 2D (synthetic) images comparing them with 2D images; BI-RADS 5.
Fig. 6.54
(a, b) 2D synthetic Robl (a) and Rcc (b)
Fig. 6.55
(a, b) 3D Robl (a) and Rcc (b)
Fig. 6.56
3D magnification Robl
Fig. 6.57
3D magnification Rcc
Differential Diagnosis on 2D
Abscess, granuloma, fat necrosis, radial scar, complex sclerosing lesion, LCIS, invasive breast cancer.
Conclusion/Diagnosis with 3D
Highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy.
US
Typical ill-defined hypoechoic shadowing lesion with interrupted Cooper ligaments, vertically orientated lesion, hypervascular (Fig. 6.58); BI-RADS 5.
Fig. 6.58
US
Histology
IDC, pT1c pN0 R0 Mx G1.
Further Imaging/Further Diagnostic
In breast density ACR III and IV, preoperative MRI is recommended (disease extent, associated DCIS/extensive intraductal component [EIC]), multifocality in 15 %, bilaterality in 5 %).
MRI
T1 fat sat (FS) contrastenhancing (C)+ irregular mass with rim enhancement, rapidly enhanced, plateau or washout, > 95% sensitivity.
6.2.2 Case 2
General Information/Clinical Issues
Patient was a 81-year-old female; status after reduction mammoplasty, symptomatic with palpable lump on the left side, no familial history.
Mammographic Analysis on Prior 2D and 2D (Synthetic) and 3D
Breast density ACR III; comparing current 2D (synthetic) with previous 2D (Fig. 6.59a, b), there was a focus of a slight increase in density (9 mm) mediocaudal close to the chest wall, more obvious in Lcc projection (Fig. 6.60a, b). US is recommended; BI-RADS 0/4. 3D shows a dense slightly spiculated growing mass without calcification (Figs. 6.61a, b, 6.62 and 6.63 [3D magnification, same figure as 6.61a, b]) compared with prior 3D (Fig. 6.64), BI-RADS 4.
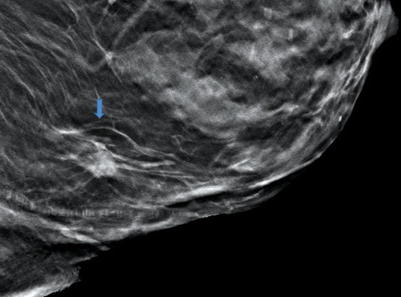
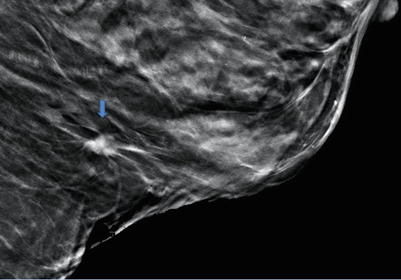
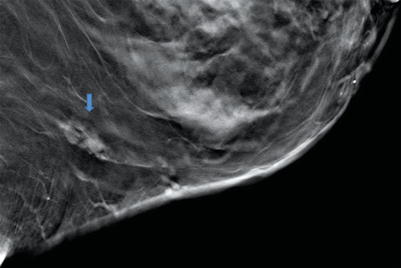
Fig. 6.59
(a, b) 2D Lcc (a) and Lobl (b) in 2012
Fig. 6.60
(a, b) 2D synthetic Lcc (a) and Lobl (b) in 2012
Fig. 6.61
(a, b) 3D Lcc (a) and Lobl (b) in 2012
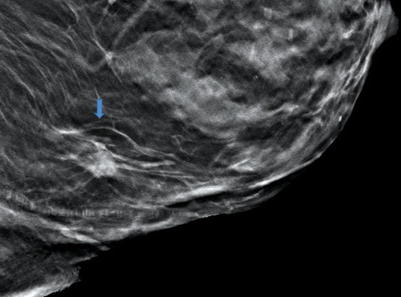
Fig. 6.62
3D magnification Lcc in 2012
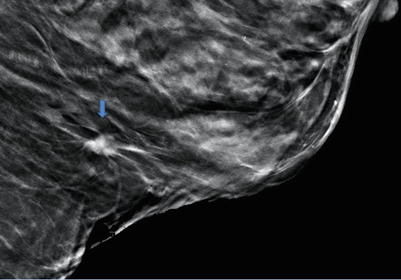
Fig. 6.63
3D magnification Lobl in 2012
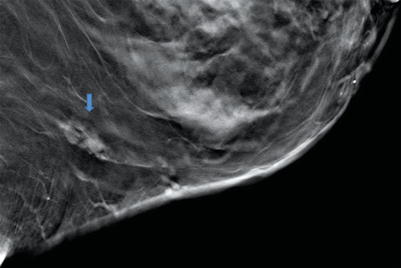
Fig. 6.64
3D magnification Lobl in 2010
Differential Diagnosis on 2D
Granuloma, fat necrosis, radial scar, complex sclerosing lesion, LCIS, IDC, and all other types of breast cancer.
Conclusion/Diagnosis with 3D
Higher diagnostic accuracy with 3D. On 2D, only an increase in density was seen; on 3D spiculated mass suggestive of malignancy (BI-RADS 4).
Recommendation
US biopsy.
US
Ill-defined hypoechoic shadowing lesion with interrupted Cooper ligaments, hypervascular, (Fig. 6.65); BI-RADS 5.
Fig. 6.65
US
Histology
IDC.
Further Imaging/Further Diagnostic
In breast density ACR III and IV, preoperative MRI is recommended (disease extent, in 15 % multifocal, in 5 % bilateral). T1 FS C+ irregular mass with rim enhancement, rapidly enhanced, plateau or washout, > 95% sensitivity
6.2.3 Case 3
General Information/Clinical Issues
Patient was a 65-year-old female; asymptomatic, familial history (grandmother), HRT, screening examination.
Mammographic Analysis on 2D and 3D
Breast density ACR III. On 2D only in Lcc, subtle architectural distortion lateral with indicative thick band pulling to the chest wall (Figs. 6.66a, b and 6.67a, b), additional spot recommended; BI-RADS 0. 3D Lcc and Lml demonstrate an isodense 6 mm stellate mass (Figs. 6.68a, b, 6.69, and 6.70 [3D magnification, same figure as 6.68a, b]); BI-RADS 4
Fig. 6.66
(a, b) 2D Robl (a) and Lobl (b) in 2009
Fig. 6.67
(a, b) 2D Rcc (a) and Lcc (b) in 2009
Fig. 6.68
(a, b) 3D Lml (a) and Lcc (b) in 2009
Fig. 6.69
3D magnification Lml
Fig. 6.70
3D magnification Lcc
Differential Diagnosis on 2D
Summation artifact due to superimposed glandular breast tissue, radial scar, DCIS, LCIS, all other types of breast cancer.
Conclusion/Diagnosis with 3D
BI-RADS upgrade on 3D, spiculated mass suggestive of malignancy (BI-RADS 4).
Recommendation
US biopsy.
US
Lesion not visible on US; MRI confirmed lesion, subsequently S-VAB was done (no images).
Histology After S-VAB
Sclerotic necrotic fibroadenoma, papilloma, apocrine metaplasia; the following breast surgery confirmed IDC.
Further Imaging/Further Diagnostic
In breast density ACR III and IV, preoperative MRI is recommended (disease extent, associated DCIS/IC, multifocality in 15 %, bilaterality in 5 %); on performed MRI, there was unifocal disease (Fig. 6.71).
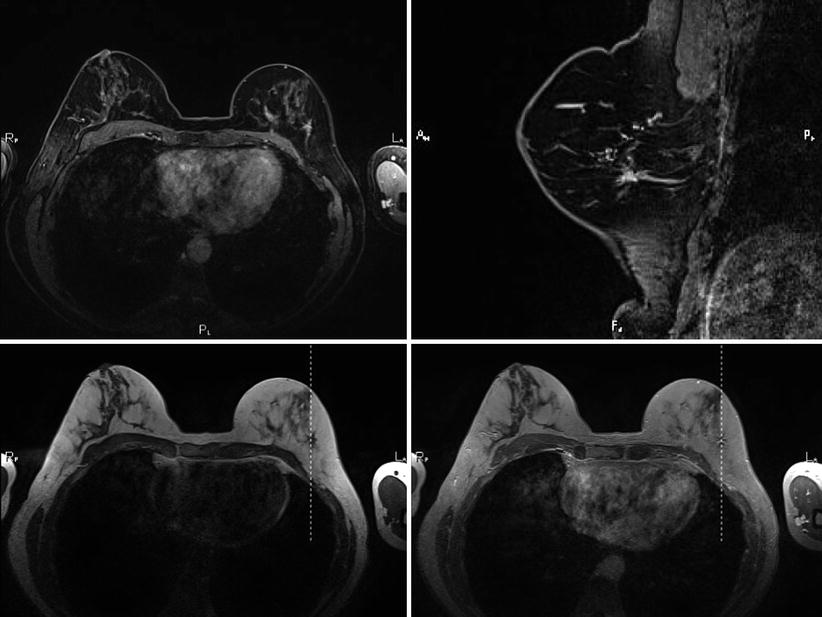
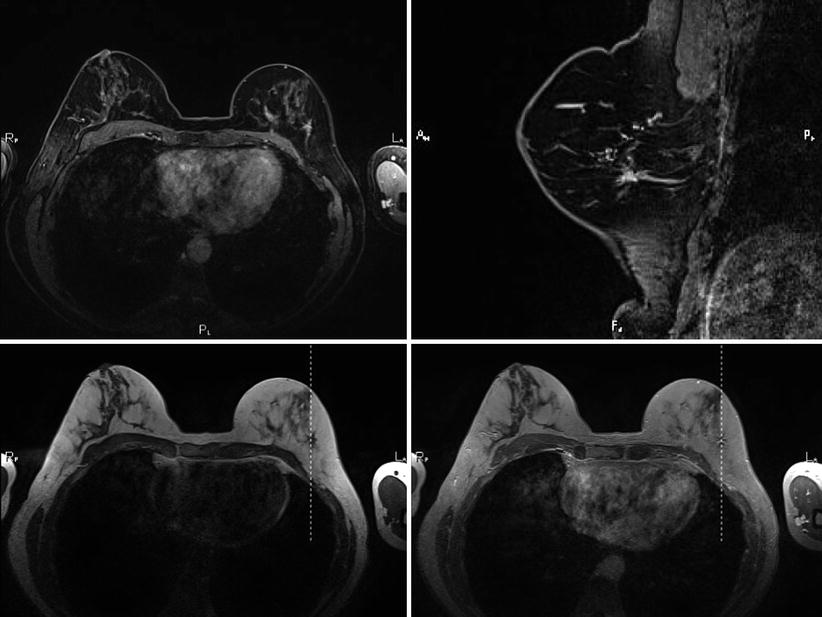
Fig. 6.71
MRI
MRI
T1 FS C+ irregular mass with rim enhancement, rapidly enhanced, plateau or washout, > 95% sensitivity.
6.2.4 Case 4
General Information/Clinical Issues
Patient was a 66-year-old female; asymptomatic, no familial history, mastodynia, controlled under HRT.
Mammographic Analysis on 2D and 3D
Further Diagnostics
Spot and US required; BI-RADS 4. 3D demonstrated a dense 16 mm stellate mass (Fig. 6.74a, b); BI-RADS 5.


Fig. 6.72
(a, b) 2D Robl (a) and Lobl (b) in 2009
Fig. 6.73
(a, b) 2D Rcc (a) and Lcc (b) in 2009
Fig. 6.74
(a, b) 3D Lobl (a) and Lcc (b) in 2009
Differential Diagnosis on 2D
Summation artifact due to superimposed glandular breast tissue, complex sclerosing lesion, DCIS, all other types of breast cancer.
Conclusion/Diagnosis with 3D
BI-RADS upgrade on 3D, no additional X-ray of the spiculated mass needed, highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy.
US
Typical ill-defined hypoechoic shadowing lesion with echogenic halo (Fig. 6.75); BI-RADS 4.
Fig. 6.75
US
Histology
IDC, moderately differentiated G2.
Further Imaging/Further Diagnostic
No preoperative MRI recommended.
See Sect. 6.16, Case 3: Malignant changes; ACR IV.
See Sect. 6.5, Case 1: Malignant medullary changes.
See Sect. 6.15, Case 4: Malignant changes: one-view-only findings.
Comment
Typical findings in IDC are a dense spiculated or microlobulated mass, grouped associated microcalcifications in 30 %. It is the most common form (70 %) of invasive breast cancer; most women detect a lump themselves unless routinely screened; IDC occurs in all age groups (peak age 55–60 s), age < 40 years rare (consider familial cancer); hard and stiff lump; palpation often overestimate the size of the lesion; prognosis depends on lymph node status > tumor size > tumor grading—well, moderately, or poorly differentiated (G1 better than G2, G2 better than G3).
Image Interpretation Pearls:
Morphologically, IDC is a very variable tumor (asymmetric density, distortion, circumscribed round or oval mass); compare with prior mammogram if possible and look for new or increased density, associated grouped microcalcifications (may be the only hint in breast density ACR III and IV), skin or nipple retraction (rare) due to often strong fibrotic component of the tumor. Caution – in dense breasts 50 % of IDCs are occult on mammography.
6.3 Malignant Changes: LCIS
6.3.1 Case 1
General Information/Clinical Issues
Patient was a 75-year-old female; referred for image-guided biopsy due to grouped microcalcifications with suspected associated distortion lateral on the right side.
Mammographic Analysis 2D, 2D (Synthetic) and 3D
On 2D Rcc in 2012 (Fig. 6.76a, b) possible architectural distortion lateral on right side, spot or 3D recommended (BI-RADS 0). On 2D (synthetic) there was a combination of clearly visible clustered microcalcifications (Fig. 6.77a, b) and the more obvious architectural distortion could represent a malignancy; BI-RADS 4. On 3D (Fig. 6.78a, b) the suspected lesion caused a clear architectural distortion in both views (cc and obl), with associated microcalcifications. Furthermore, an additional spiculated mass was detected close to the architectural distortion; BI-RADS 5.
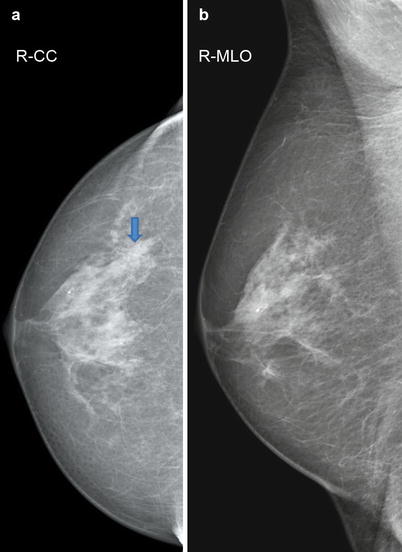
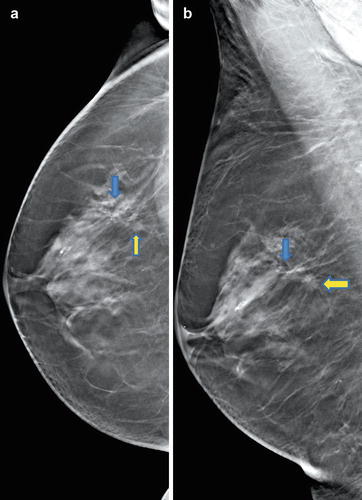
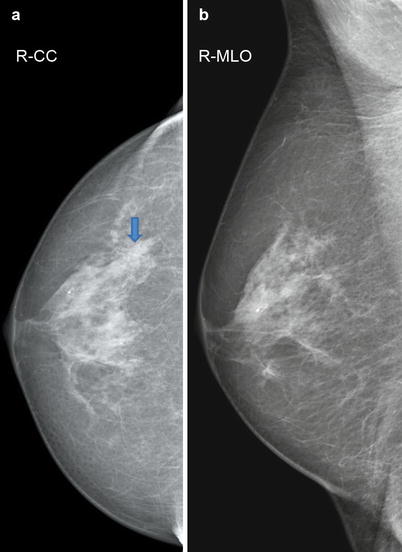
Fig. 6.76
2D Rcc (a) and Robl (b)
Fig. 6.77
2D synthetic Rcc (a) and Robl (b)
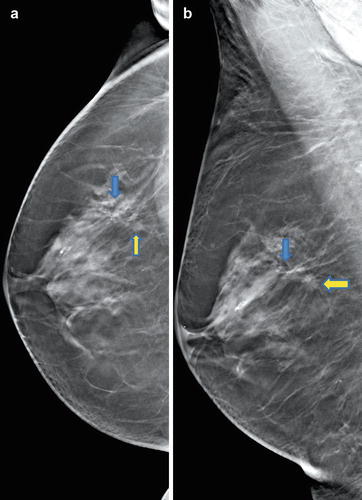
Fig. 6.78
3D Rcc (a) and Robl (b)
Differential Diagnosis on 2D
Fibrocystic changes, ADH and ALH, LCIS, DCIS, IDC (BI-RADS 4).
Conclusion/Diagnosis with 3D
On 3D the morphology of the architectural distortion is clearer and pathbreaking, leading to a BI-RADS upgrade with the second lesion detected (BI-RADS 5).
Recommendation
Rule out malignancy with US-guided biopsy or T-VAB (BI-RADS 4).
US
Histology
I. Biopsy (lesion I) – lobular invasive cancer, II. biopsy (lesion II) – LCIS.
Further Imaging/Further Diagnostic
MRI discussed for further evaluation (non-mass enhancement or non-mass ductal enhancement) because of tendency to multifocality/multicentricity and bilaterality.
6.3.2 Case 2
General Information/Clinical Issues
Patient was a 51-year-old female; referral for punch biopsy due to a mammographically and sonographically (external) unclear lesion left side at 1 o’clock.
Mammographic Analysis 2D and 3D
On 2D there was a nonspecific 6 mm density localized close to the chest wall on the left side in one of the forbidden areas, and this could represent a malignancy (Fig. 6.80); BI-RADS 0/4 with recommended US and biopsy standby. On 3D the lesion caused an architectural distortion (Fig. 6.81 without clip); BI-RADS 4.
Fig. 6.80
2D Lobl in 2014
Fig. 6.81
3D Lobl in 2014
Differential Diagnosis
On 2D ectopic breast tissue, fibrocystic changes, fibroadenoma, lymph node, ADH and ALH, LCIS, DCIS, IDC. The histological result of a fibroadenoma after biopsy 1; therefore, diagnosis on 2D may be acceptable.
Conclusion/Diagnosis with 3D
Biopsy 1.—fibroadenoma, histological result and 3D morphology of the lesion are not conclusive (Fig. 6.82 after biopsy—correct location of the clip inside the lesion); referrral for T-VAB (Fig. 6.83a, b). Biopsy 2. revealed LCIS.
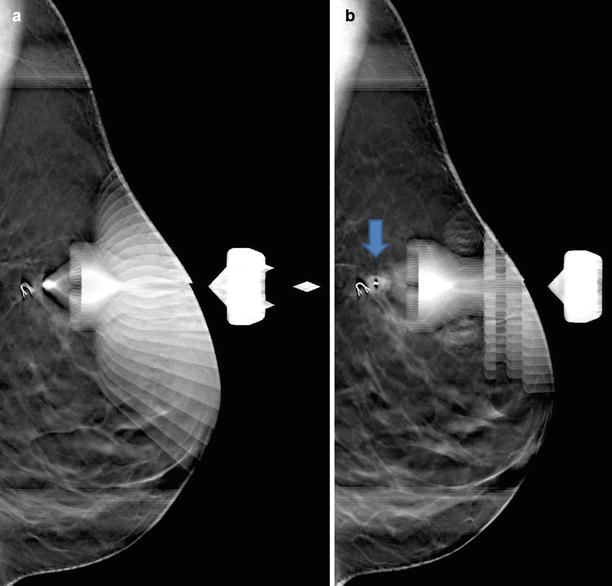
Fig. 6.82
3D Lobl with inserted clip in 2014
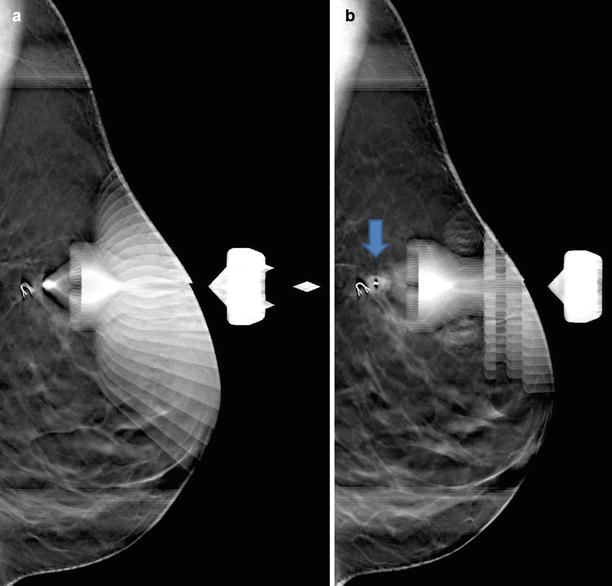
Fig. 6.83
(a, b) T-VAB in decubitus position (a) with inserted clip (b)
Recommendation
Rule out malignancy with US-guided biopsy (BI-RADS 4).
US
Histology
1. Biopsy—fibroadenoma after US-guided biopsy; 2. Biopsy—LCIS after T-VAB.
Further Imaging/Further Diagnostic
MRI discussed for further evaluation (non-mass enhancement or non-mass ductal enhancement) because of tendency to multifocality/multicentricity and bilaterality.
Comment
Surgical excision recommended (biopsy → surgery: histologic upgrade in 15–25 %); in premenopausal women the risk of developing breast cancer is (8–12 × higher or 1 % per year); consider screening of high-risk patients.
Image Interpretation Pearls
Often there is an incidental finding and search for other lesions in histologically proven LCIS. Often there is an incidential finding. On mammographic analysis there are amorphous calcifications, and, rarely, a mass with or without calcifications.
6.4 Malignant Changes: Lobular
6.4.1 Case 1
General Information/Clinical Issues
Patient was a 71-year-old female. 2D in 2007 with formerly palpable lump left side lateral without suspicious finding; on US 3 years later hypoechoic lesion right side, suspicious for breast cancer.
Mammographic Analysis 2D and 3D
Breast density ACR III. On 2D inhomogeneous breast tissue with areas of pre-existing higher density on the right side laterocranial and at 12 o’clock position on the left side (Figs. 6.86a, b and 6.87a, b); no circumscribed distortion or mass on follow-up 2D (Fig. 6.88a, b); BI- RADS 0. 3D shows, in Robl view, a 22 mm microlobulated slightly spiculated mass with very fine grouped monomorphous microcalcifications (Fig. 6.89a, b); BI-RADS 4.
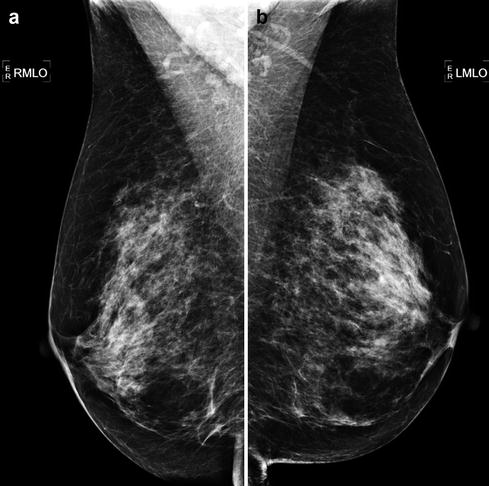
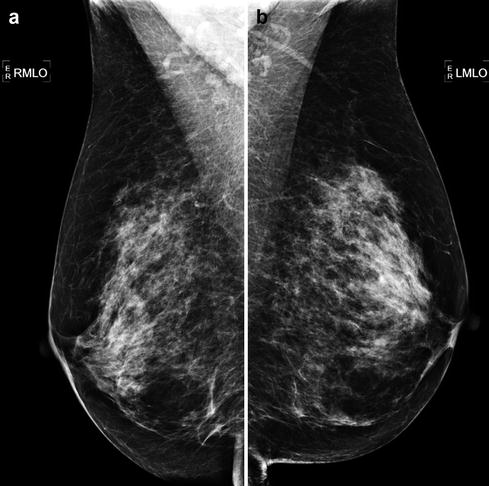
Fig. 6.86
(a, b) 2D Robl (a) and Lobl (b) in 2007
Fig. 6.87
(a, b) 2D Rcc (a) and Lcc (b) in 2007
Fig. 6.88
(a, b) 2D Rcc (a) and Robl (b) in 2010
Fig. 6.89
(a, b) 3D Rcc slices in 2010
Differential Diagnosis on 2D
Mammographically missed cancer: on 2D , US recommended (BI-RADS 0).
Conclusion/Diagnosis with 3D
One of the fundamental challenges for the assessment of 2D is dense breast tissue, due to the low sensitivity and low positive predictive value of 2D. Superimposition of overlying structures obscures true lesions, as shown in this case on 2D. Creation of 1 mm thin slices on 3D reveals the inner architecture of the breast with reduced tissue overlapping, especially in dense breasts, and makes the tumor visible (BI-RADS 4).
Recommendation
US biopsy
US
No internal US.
Histology
Lobular invasive carcinoma, pT2N1(3/16)R0G2.
Further Imaging/Further Diagnostic
MRI recommended for assessing the extent of disease, spiculated lesions, isolated architectural distortions, sometimes multiple foci with interconnecting septal enhancement, rare isolated septal enhancement; can be false negative; look for axillary lymphadenopathy.
MRI
On the performed MRI (Fig. 6.90) there was a solitary lobular invasive cancer (40 mm), size was underestimated on 3D.
Fig. 6.90
MRI
6.4.2 Case 2
General Information/Clinical Issues
Patient was a 83-year-old female; T1N0 left side.
Mammographic Analysis on 2D (Synthetic) and 3D
Breast density ACR I. Slight asymmetrical density with emphasis only on supporting tissue (septa, interstitium); architectural distortion in adipose tissue on the left side central cranial on 2D (synthetic) (Figs. 6.91a, b and 6.92a,b), more obvious on 3D (Figs. 6.93a, b and 6.94 [3D magnification, same figure as 6.93a]), US recommended in biopsy standby (Fig. 6.95); BI-RADS 0/4.


Fig. 6.91
(a, b) 2D synthetic Robl (a) and Lobl (b) in 2012
Fig. 6.92
(a, b) 2D synthetic Rcc (a) and Lcc (b) in 2012
Fig. 6.93
(a, b) 3D Lcc (a) and Lobl (b) in 2012
Fig. 6.94
3D magnification Lcc
Fig. 6.95
US
Differential Diagnosis on 2D (Synthetic)
Fat necrosis, complex sclerosing lesion, rare type of invasive lobular carcinoma.
Conclusion/Diagnosis with 3D
In combination with a palpable lump, exclude this rare type of invasive lobular carcinoma by US-guided biopsy (BI-RADS 4).
Recommendation
US biopsy.
US
Diffuse hypoechoic structure and sound alteration, with appearance similar to a fat necrosis (Fig. 6.95); BI-RADS 4.
Histology
Invasive lobular carcinoma.
Further Imaging/Further Diagnostic
MRI recommended for assessing the extent of disease, spiculated lesions, isolated architectural distortions, sometimes multiple foci with interconnecting septal enhancement, rare isolated septal enhancement; can be false negative; look for axillary lymphadenopathy.
6.4.3 Case 3
General Information/Clinical Issues
Patient was a 89-year-old female. No-risk patient, symptomatic with palpable lump detected1 year previously, US-guided biopsy on first presentation (fibrolipoma), follow-up in 2010, no prior 2D.
Mammographic Analysis 2D and 3D
Breast density ACR II; nonspecific slightly diffuse radial density without a center, centrally located close to the chest wall (Figs. 6.98a, b and 6.99a, b); US recommended; BI-RADS 0. On 3D spiculated hyperdense fatty-tissue-containing lesion, 30 mm in size, located in the centrolateral posterior part of the left breast near the chest wall (Fig. 6.100a, b), not representing a fibrolipoma; BI-RADS 5.
Fig. 6.98
(a, b) 2D Robl (a) and Lobl (b) in 2010
Fig. 6.99
(a, b) 2D Rcc (a) and Lcc (b) in 2010
Fig. 6.100
(a, b) 3D slices Lcc
Differential Diagnosis on 2D (Synthetic)
Asymmetric involution (glandular breast tissue), complex sclerosing lesion, diffuse interstitial edema, lymphangitis carcinomatosis, invasive cancer (BI-RADS 0).
Conclusion/Diagnosis with 3D
Suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy.
Histology
Invasive lobular carcinoma, pT2N0(0/13),R0,G2.
Further Imaging/Further Diagnostic
MRI recommended; not performed.
6.4.4 Case 4
General Information/Clinical Issues
Patient was a 71-year-old female; screening under HRT, T0N0.
Mammographic Analysis 2D and 3D
Breast density ACR II; asymmetric involution with a little more breast tissue on the left side, similar to prior 2D (Figs. 6.106a, b and 6.107a, b). On the 2-year follow-up 2D (Fig. 6.108a, b) BI-RADS 1. On 3D there were two spiculated interconnected (septal) isodense lesions, 9 and 10 mm in size, located lateral in the right breast (Fig. 6.109a, b); BI-RADS 5.
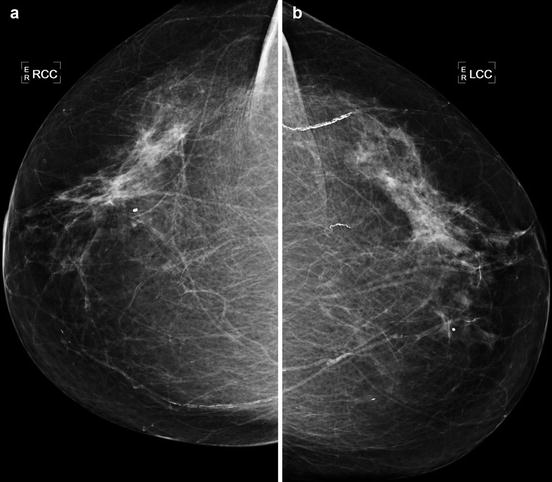
Fig. 6.106
(a, b) 2D Robl (a) and Lobl (b) in 2011
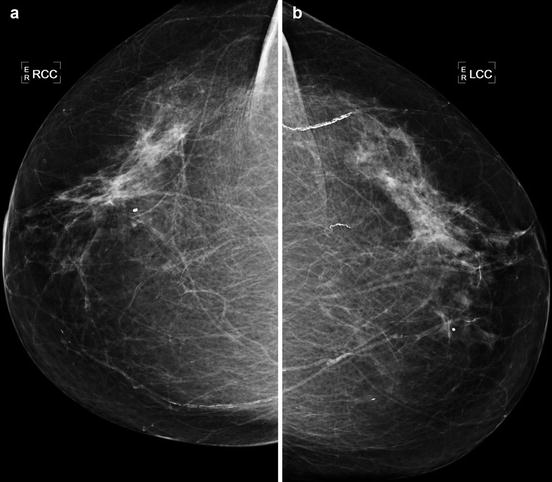
Fig. 6.107
(a, b) 2D Rcc (a) and Lcc (b) in 2011
Fig. 6.108
(a, b) 2D Rcc (a) and Robl (b) in 2013
Fig. 6.109
(a, b) 3D Rcc (a) and Robl (b) in 2013
Differential Diagnosis on 2D
Normal variant of asymmetric involution (BI-RADS 1).
Conclusion/Diagnosis with 3D
3D was highly suggestive of malignancy, showed breast cancer missed on 2D; upgrade of BI-RADS (BI-RADS 5).
Recommendation
US biopsy.
US
No internal US.
Histology
Invasive lobular carcinoma.
Further Imaging/Further Diagnostic
Preoperative MRI recommended.
MRI
Performed MRI (Fig. 6.110) confirmed a bifocal invasive breast cancer at 9 o’clock and a non-mass enhancement at 3 o’clock. MRI-guided biopsy confirmed DCIS G2 at 3 o’clock, with detection of multicentricity.
Fig. 6.110
MRI
6.4.5 Case 5
General Information/Clinical Issues
Patient was a 65-year-old female; family risk (sister), palpable lump 9 o’clock right side T1N0.
Mammographic Analysis Prior 2D and 2D (Synthetic) and 3D
Breast density ACR II; prior 2D (Fig. 6.111a, b) in 2010 identical to current 2D (synthetic) and 3D in 2012 (Figs. 6.112a, b and 6.113a, b), no obvious mass or distortion, palpable lump marked at 9 o’clock; BI-RADS 1.
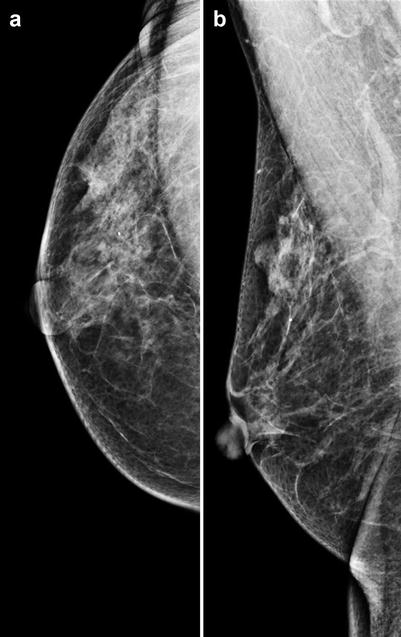
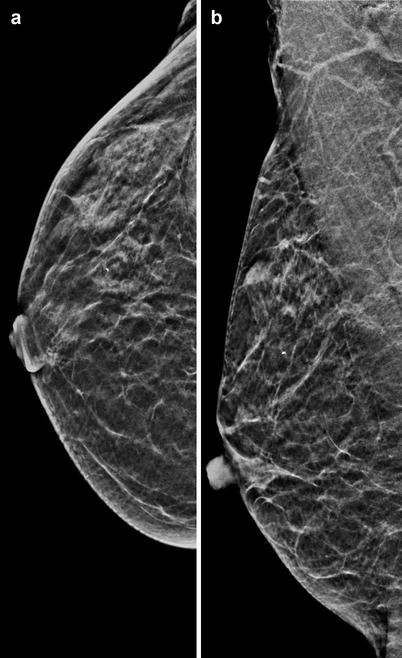
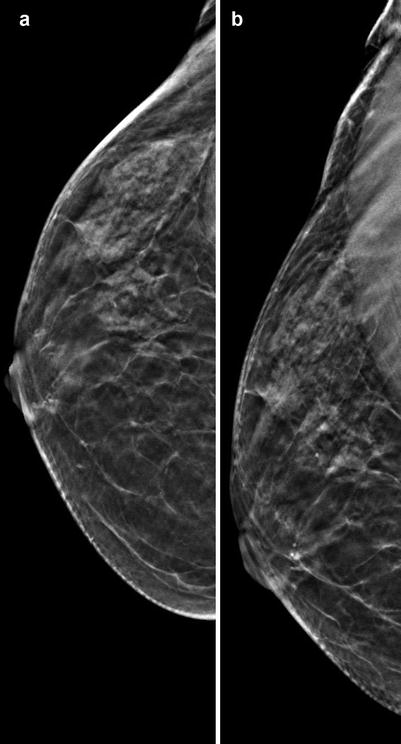
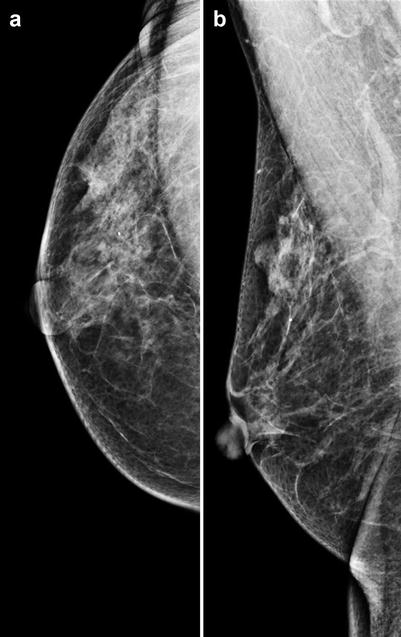
Fig. 6.111
(a, b) 2D Rcc (a) and Robl (b) in 2010
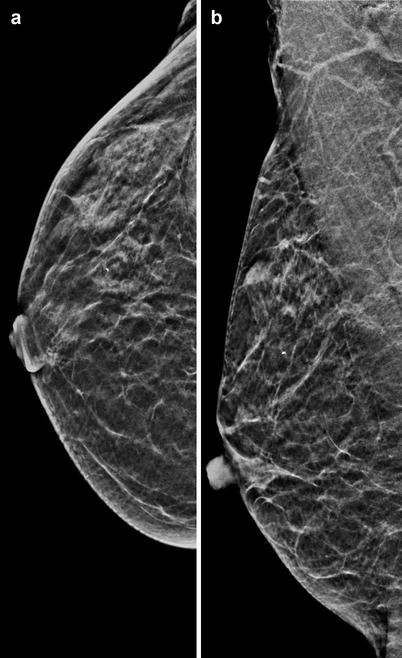
Fig. 6.112
(a, b) 2D synthetic Rcc (a) and Robl (b) in 2012
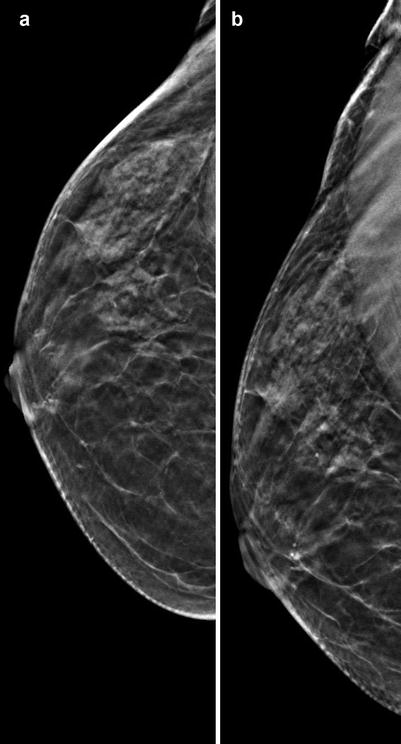
Fig. 6.113
(a, b) 3D Rcc (a) and Robl (b) in 2012
Differential Diagnosis on 2D (Synthetic)
Occult, missed cancer in ACR II.
Conclusion/Diagnosis with 3D
With 2D (synthetic) and 3D no suspicious lesion could be detected (formal BI-RADS 1), but the newly emerged palpation required a complementary US (BI-RADS 0).
Recommendation
US
Histology
Lobular invasive carcinoma, pT1cpN0,R0G2.
Further Imaging/Further Diagnostic
Preoperative MRI recommended.
MRI
Performed MRI showed no contrast enhancement of the lesion (Fig. 6.115), but the slightly hyperintense lesion on coronal T2 images is suspicious in DWI (diffusion weighted images) and ADC (apparent diffusion coefficient).
Fig. 6.115
MRI
(see Sect. 6.15 case 1. Malignant changes one-view-only findings)
Further Imaging/Further Diagnostic
MRI recommended for assessing the extent of disease, spiculated lesions, isolated architectural distortions, sometimes multiple foci with interconnecting septal enhancement, rare isolated septal enhancement; can be false negative; look for axillary lymphadenopathy.
Comment
Invasive lobular carcinoma has the lowest detection rate of breast carcinomas; therefore, it is often diagnosed late; sensitivity on mammography is ~50–60 %; sensitivity on US is better, ~85–90 %. The entity accounts for 10–15 % of all breast cancers (often LCIS- or ALH-associated precursors); occurs at all ages, peak between 40 and 60 years; palpable thickening or palpable mass; tendency to multicentricity, multifocality, and bilaterality; prognosis equal to IDC.
Image Interpretation Pearls
Chameleons—from spiculated mass, isolated architectural distortion, focal asymmetry to only septal thickening (worst prognosis), calcifications only in 10 %, tendency to multifocality, increased rate of bilateral cancer, extend of the disease often.
6.5 Malignant Changes: Medullary
6.5.1 Case 1
General Information/Clinical Issues
Patient was a 50-year-old female; biopsy-proven breast cancer on the right side.
Mammographic Analysis on 2D (Synthetic) and 3D
Breast density ACR II. On 2D (synthetic) suspect microlobulated circumscribed round-oval mass (17 mm) mediocaudal right side without calcifications (Fig. 6.116a, b), US required with biopsy; BI-RADS 4. 3D demonstrated only the partially indistinct margins of the mass clearly (Fig. 6.117a, b); BI-RADS 4.
Fig. 6.116
(a, b) 2D synthetic Rcc (a) and Robl (b) in 2013
Differential Diagnosis on 2D
Fibroadenoma, abscess, granuloma, fat necrosis, radial scar, complex sclerosing lesion, LCIS, all other types of breast cancer.
Conclusion/Diagnosis with 3D
Suggestive of malignancy (BI-RADS 4).
Recommendation
US biopsy.
US
No internal US.
Histology
Multifocal (22 mm and 5 mm) invasive ductal carcinoma, moderately differentiated G2, triple negative (estrogen receptor [ER]-, progesterone receptor [PR]-, Her-2 negative), pT2(m:2)pN0(0/1)(sn)L1R0.
Further Imaging/Further Diagnostic
No preoperative MRI in this case; in breast density ACR III or IV, MRI is recommended; look for common satellite lesions and axillary lymphadenopathy.
Comment
Special type of IDC (controversial discussion), 5 % of all breast cancers (younger patients and those with BRCA gene), rapidly growing palpable soft mass, calcifications uncommon, tendency to multicentricity and bilaterality, triple negative, early recurrences but prognosis better than IDC (5 year survival 90 %.).
Image Interpretation Pearls
may be, in its typical form, difficult to distinguish from fibroadenoma; satellite lesions common; look for axillary lymph nodes.
Comment US
oval – round or lobular circumscribed hypoechoic lesion; look for indistinct or microlobulated margins due to lymphocytic-infiltrative changes, hyperechogenic halo, posterior enhancement.
6.6 Malignant Changes: Papillary
6.6.1 Case 1
Image data courtesy of Dr. A. Belfer and Dr. V. Schivartche – CDB Premium, Sao Paulo, Brazil.
General Information/Clinical Issues
In 2013 the patient refused biopsy, in 2014 the lesion had become bigger and the patient accepted biopsy.
2D (Synthetic) and 3D Mammographic Analysis
Breast density ACR II. On 2D and 2D (synthetic) in 2013 most likely benign lesion on the left side (Figs. 6.118a, b and 6.119a, b), US recommended; BI-RADS 0. On 3D circumscribed margins of a 5 mm mass shown on the left side (Fig. 6.120a, b); BI-RADS 0. On 2D, 2D (synthetic), and 3D in 2014 the circumscribed mass had become bigger (Figs. 6.121a, b, 6.122a, b and 6.123a, b); BI-RADS 4.
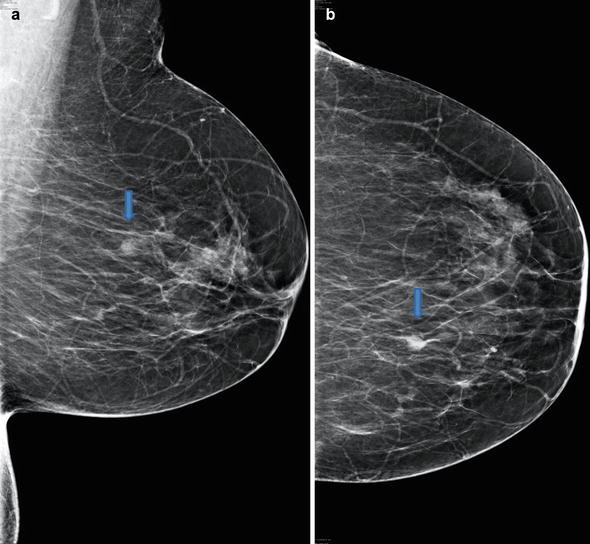
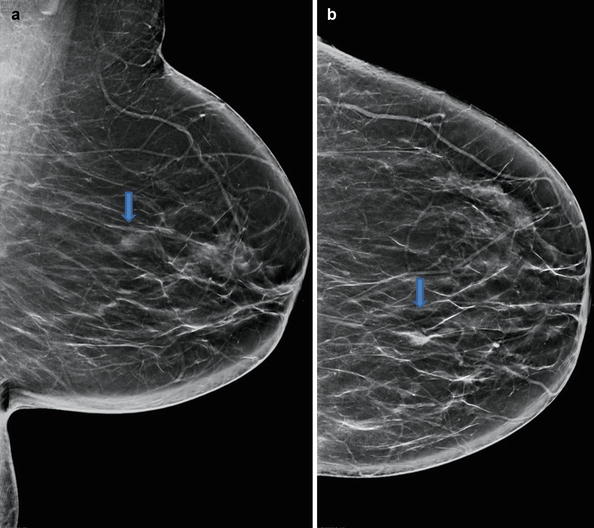
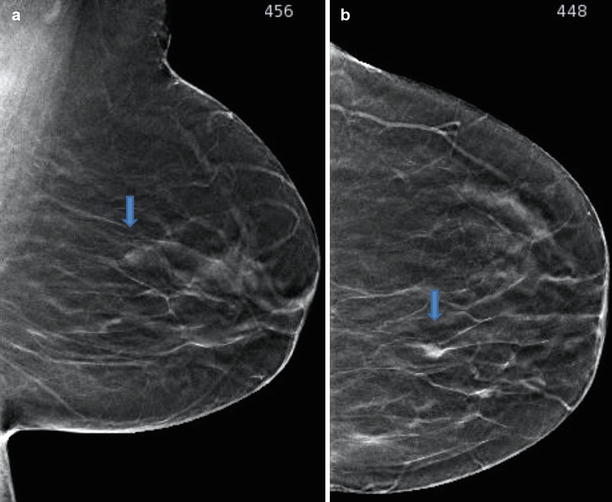
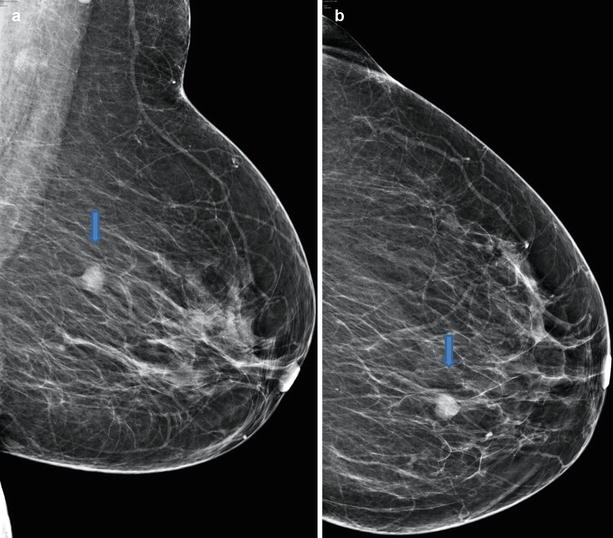
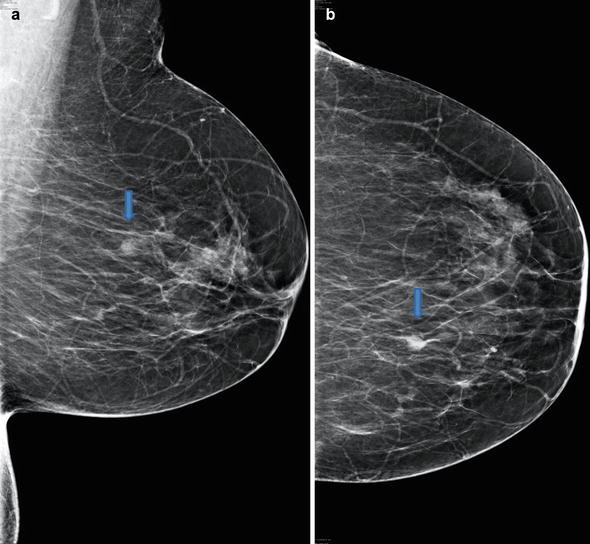
Fig. 6.118
(a, b) 2D Lobl (a) and Lcc (b) in 2013
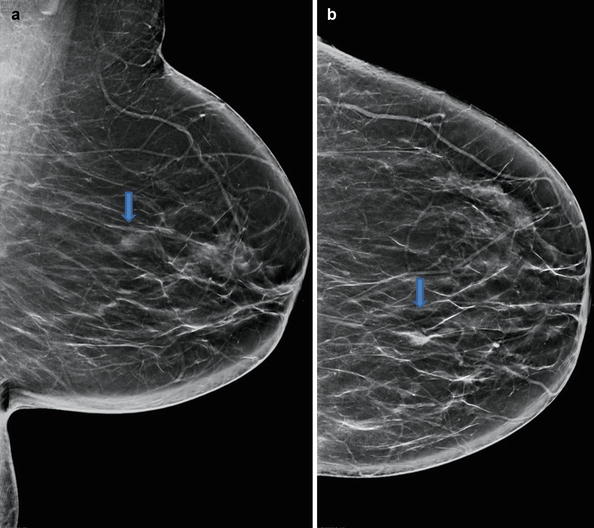
Fig. 6.119
(a, b) 2D (synthetic) Lobl (a) and Lcc (b) in 2013
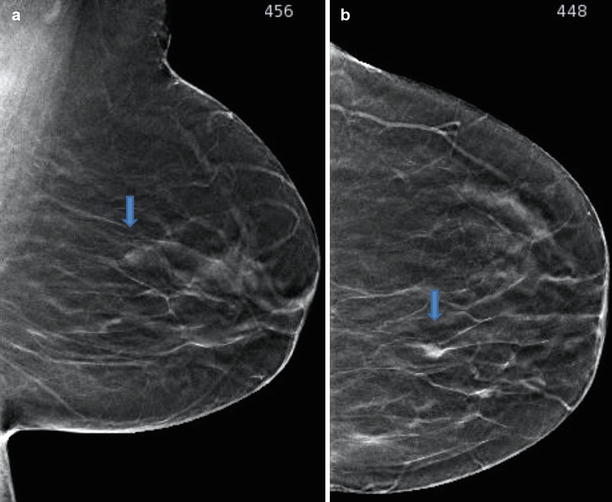
Fig. 6.120
(a, b) 3D Lobl (a) and Lcc (b) in 2013
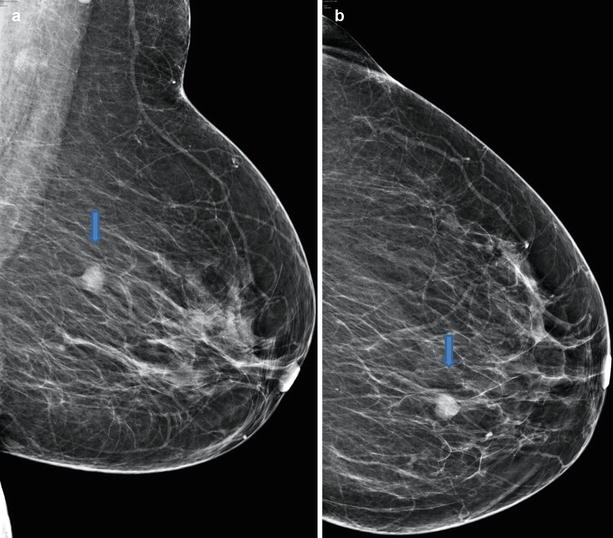
Fig. 6.121
(a, b) 2D Lobl (a) and Lcc (b) in 2014
Fig. 6.122
(a, b) 2D synthetic Lobl (a) and Lcc (b) in 2014
Fig. 6.123
(a, b) 3D Lobl (a) and Lcc (b) in 2014
Differential Diagnosis on 2D and 2D (Synthetic) in 2013
Cyst, lymph node, fibroadenoma, vessel loop (BI-RADS 0).
Conclusion/Diagnosis with 3D in 2014
Due to the increase in size, the biological behavior (dignity) of the lesion is unclear; malignancy cannot be excluded (BI-RADS 4).
Recommendation
US biopsy.
US
Histology
Papillary cancer G 2.
Further Imaging/Further Diagnostic
No MRI recommended.
Comment
Rare 1–2 %, age peak 50–60 years, often lobulated subareolar lesion, rarely associated fine granular microcalcifications, circumscribed margins – caution: circumscribed margins on 2D and 3D are not always benign; in the intracystic growth of papillary carcinoma the circumscribed margins of the lesion are unharmed. The margins get indistinct when the cyst wall is infiltrated.
Image Interpretation Pearls
Nodule is less visible on 2D and 2D (synthetic). False spiculae due to superposition of blood vessel and fiber. 3D is very good for the evaluation of margins. Good example of why you need 3D even if you see it on 2D and 2D (synthetic); look for asymmetric density in retromammillary region.
6.7 Malignant Changes: Tubular
6.7.1 Case 1
General Information/Clinical Issues
Patient was a 73-year-old female; suspect lesion on screening mammogram left side, no-risk patient, asymptomatic.
Mammographic Analysis 2D (Synthetic) and 3D
Breast density ACR II. Spiculated isodense lesion, 9 mm in size, located in the outer upper quadrant of the left breast, near the chest wall (Figs. 6.126a, b, 6.127a, b, and 6.128 [3D magnification, same figure as 6.126a]); spiculated isodense lesion on 3D Lobl better delineated than on 2D (synthetic); Lcc not diagnostically different from Lobl; BI-RADS 5.
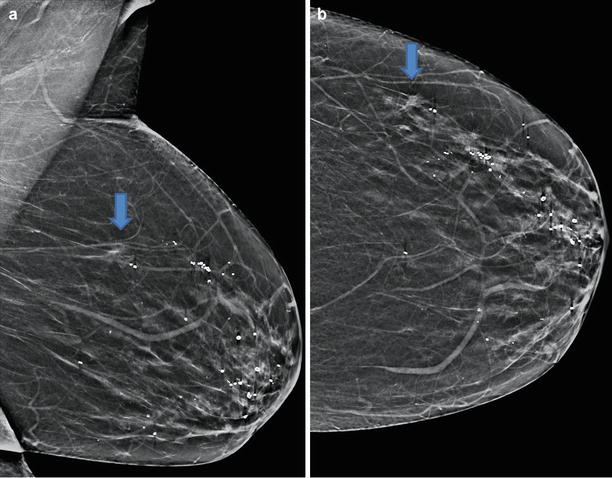
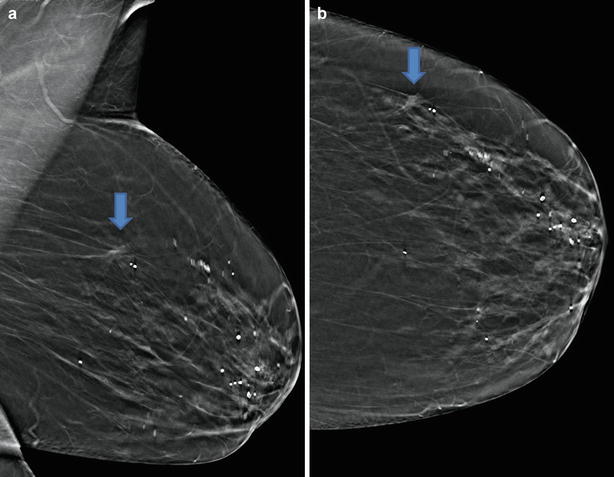
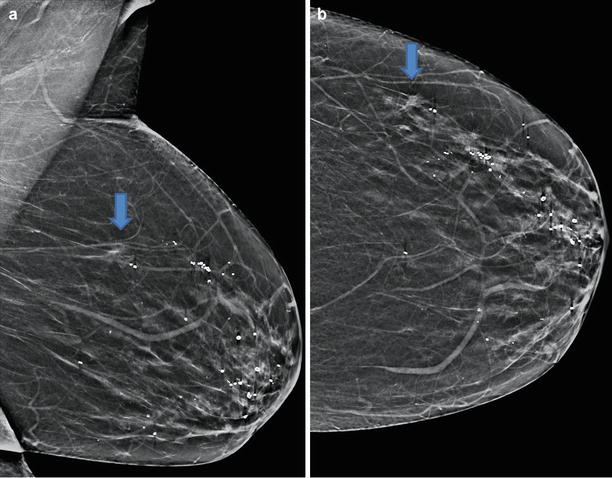
Fig. 6.126
(a, b) 2D synthetic Lobl (a) and Lcc (b) in 2014
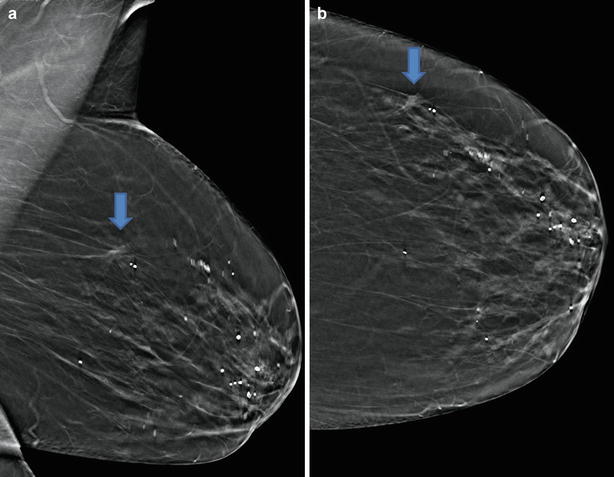
Fig. 6.127
(a, b) 3D synthetic Lobl (a) and Lcc (b) in 2014
Fig. 6.128
magnification 3D Lobl
Differential Diagnosis on 2D (Synthetic)
Radial scar, invasive cancer.
Conclusion/Diagnosis with 3D
With 2D (synthetic) and 3D highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy.
Histology
Tubular carcinoma, G1, pT1a,pN0,L0,R0 with associated DCIS (solid and cribriform), G1 and G3.
Further Imaging/Further Diagnostic
No preoperative MRI (can be false negative).
Comment
Can arise from radial scars, can be stable for years or slowly growing, rare (2 %), all ages (mean 50 years), better prognosis than IDC, 95 % 5 year survival.
Image Interpretation Pearls
ill-defined, subtle distortion or stellate mass with prominent spiculae, sometimes one-view-only finding, associated with grouped microcalcifications in 50 % and associated with DCIS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree