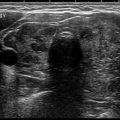
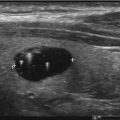
Fig. 11.1
Incidentally discovered thyroid nodule of the right thyroid gland during carotid Doppler ultrasonography
Older studies report that neck US detects incidentalomas with a prevalence of 10–30% [23–25]. However, with more recent-generation US machines, with improved spatial resolution, the prevalence can be as high as 67%, comparable to that found at autopsy [20]. The malignancy rate of thyroid incidentalomas detected by US varies from 1.3 to 12% in various studies [26, 27].
CT and MRI Scans
Thyroid incidentalomas are seen in up to 25% of contrast enhanced chest CT scans [28] and 15% of neck CT scans (Fig. 11.2) [29, 30]. CT examinations are not highly reliable in distinguishing benign from malignant thyroid lesions due to the lack of adequate spatial resolution to reveal some findings commonly used in ultrasonography such as cystic changes, microcalcifications, and irregular margins [31, 32]. In a study of Shetty et al., CT findings matched the sonographic characterization in only 53% of patients, correctly identified the dominant nodule but missed multinodularity in 30%, and underestimated the number of nodules in 10% [32]. However, most recent recommendations from the Incidental Thyroid Findings Committee seem to be taking into consideration certain CT and MRI imaging characteristics (e.g., abnormal lymph nodes and/or invasion of local tissues by the thyroid nodule) to differentiate patients with thyroid incidentalomas into a high- and low-risk category for thyroid cancer [15].
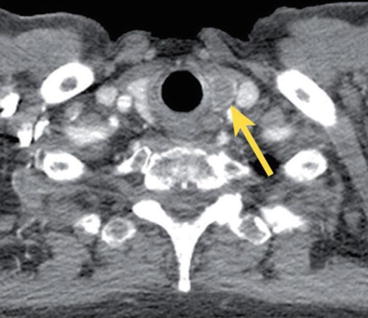
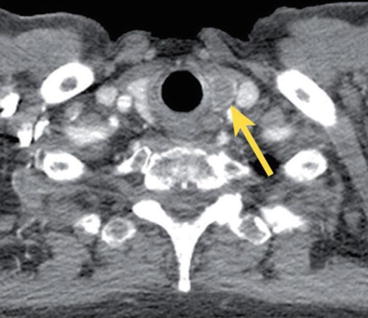
Fig. 11.2
Right thyroid nodule identified on chest CT
On MRI, both malignant and benign thyroid nodules can have isointense T1 and hyperintense T2 signals (Fig. 11.3) [33]. The malignancy rate of thyroid incidentalomas detected on CT and MRI ranges from 0 to 11% [30, 34].
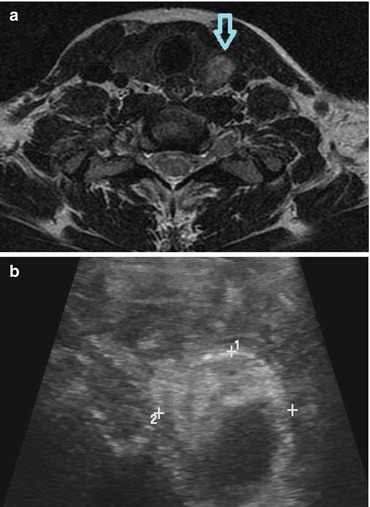
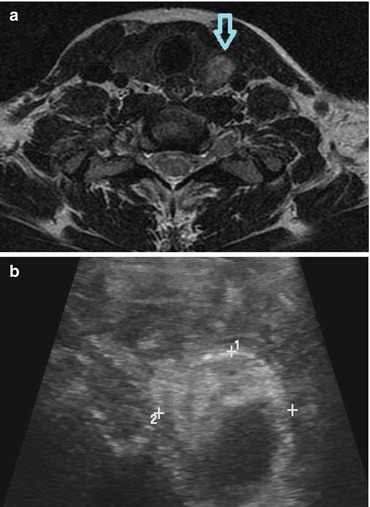
Fig. 11.3
(a) MRI of cervical spine identifies an incidental nodule in left lobe of thyroid. (b) Corresponding US image of the thyroid nodule incidentally identified on cervical MRI
18FDG-PET
18FDG-PET is increasingly performed during the evaluation of patients with both malignant and nonmalignant illness. The normal thyroid gland ) shows very low-grade FDG uptake and is usually not visualized on the whole-body 18FDG-PET scan [35–39]. Incidental 18FDG-PET uptake in the thyroid gland can be either focal or diffuse (Fig. 11.4). Focal 18FDG-PET uptake in the thyroid is incidentally detected in 1–2% of patients, while an additional 2% of patients demonstrates diffuse thyroid uptake [40, 41]. The overall reported incidence of 18FDG-PET thyroid incidentalomas varies in different studies from 1 to 4% [36, 38, 42], whereas the prevalence of thyroid cancer in these studies is remarkably high, ranging from 14 to 56% [21, 37–39, 42–45].
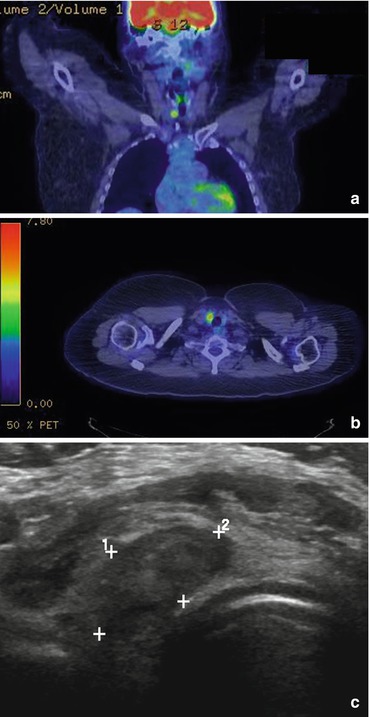
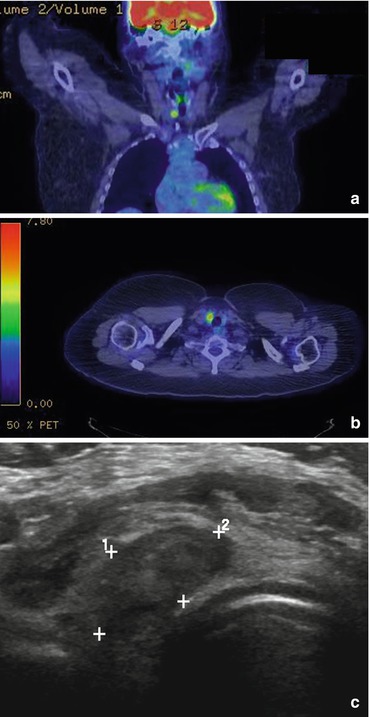
Fig. 11.4
(a, b) Focal 18FDG-PET uptake of the left thyroid gland . (c) Corresponding ultrasonography image of the left thyroid nodule identified on 18FDG-PET
Diffuse thyroid uptake most often represents benign disease corresponding to inflammatory uptake in the setting of Hashimoto’s thyroiditis or other diffuse thyroidal illness. However, if diffuse 18FDG-PET thyroid uptake is detected, it should still prompt sonographic examination to ensure there is no evidence of clinically relevant underlying nodularity.
Chest X-ray
Large-in-size thyroid nodules may as well be incidentally identified on chest X-ray, when structural deviation of adjacent organs occurs, as illustrated in Fig. 11.5. This finding should prompt further evaluation with neck ultrasound to better define nodule size, number, and sonographic characteristics and determine need for additional investigation based on these findings.
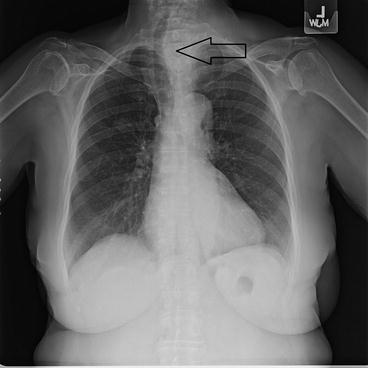
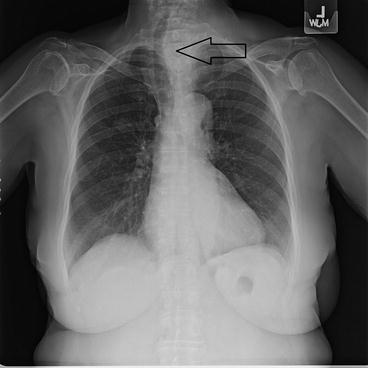
Fig. 11.5
Antero-posterior chest X-ray of a large left side thyroid nodule resulting in tracheal deviation to the right
Diagnostic and Treatment Approach
The major aim when faced with patients with thyroid incidentalomas is to exclude thyroid cancer and to identify those few patients who will benefit from additional investigations and proper management, without incurring in unnecessary tests or causing needless anxiety [48]. Despite the sharp rise in thyroid cancer detection, the mortality of thyroid cancer has not changed. This is not unexpected, considering that we are detecting more cases of thyroid cancer which are most likely clinically indolent and/or low-risk disease [13]. The appropriate management of thyroid incidentalomas remains a public health dilemma.
Given that the risk of thyroid cancer in incidentally discovered thyroid nodules is not insignificant, a thorough sonographic evaluation of the thyroid gland should be performed in the majority of patients with a thyroid incidentaloma. Once the nodule is confirmed on US, then management should be identical to a clinically apparent thyroid nodule, since the risk of malignancy is the same [9]. However, particular attention is warranted in the incidentally discovered thyroid nodule with increased 18FDG-PET uptake given that the risk of malignancy in these nodules is higher [39, 42]. The American Thyroid Association (ATA) as well as the Incidental Thyroid Findings Committee are providing guidelines for appropriate management of these patients [9, 15].
History and Physical Examination
All patients with a thyroid incidentaloma should have a complete history and targeted physical exam of the thyroid gland and cervical lymph nodes. Pertinent information in the history that should increase suspicion of malignancy include young age <35 years or older individuals >60 years [34], male sex, a prior history of childhood head and neck radiation therapy, total body radiation for bone marrow transplantation [49], exposure to ionizing radiation from nuclear fallout in childhood or adolescence [50], or a family history of thyroid cancer or other syndromes associated with thyroid cancer (Table 11.1) in a first degree relative.
Table 11.1
Syndromes associated with thyroid cancer
PTEN hamartoma tumor syndrome (Cowden’s disease) |
Familial adenomatous polyposis (FAP) |
Carney complex |
Werner syndrome/progeria |
Multiple endocrine neoplasia (MEN) 2 |
As already mentioned, patient’s age is an important clinical factor to consider. In the study of Shetty et al., patients younger than 35 years of age, with a thyroid incidentaloma, had a significantly higher incidence of malignancy (50% versus 5%) compared to patients older than 45 years of age [32]. Similar data are supported by other studies as well [51]. Two factors that could account for the above difference could be that young patients undergo imaging studies less frequently and that the prevalence of benign thyroid nodules increases with age making the ratio of malignant to benign thyroid nodules higher in young patients [32].
In addition, several studies [51, 52] have shown that there is a slightly higher risk of tumor growth in young patients (age <40 years) with subclinical, low-risk, papillary thyroid cancers compared to older individuals.
Both observations underline the importance of taking patient’s age into consideration during the diagnostic evaluation of thyroid incidentalomas.
Other important elements of the history that should raise concern for malignancy include evidence of rapid growth of a nodule, the presence of hoarseness, dysphagia, dyspnea, and neck pain. Hoarseness can occur due to tumor invasion or compression of the recurrent laryngeal nerve. Dyspnea, cough, and choking spells may occur from tracheal compression and dysphagia from esophageal compression from large thyroid nodules [48].
Physical examination is important to determine if the nodule is palpable and to evaluate the size, location, consistency, and mobility of the nodule. A solitary nodule is more likely to represent carcinoma than a single nodule within a multinodular gland, with an incidence of malignancy from 2.7 to 30% and 1.4 to 10%, respectively [53]. Yet, the overall risk of malignancy within a gland with a solitary nodule is approximately equal to that of a multinodular gland due to the additive risk of each nodule [54].
Physical findings suggestive of possible malignancy include vocal cord immobility, a very firm nodule on palpation, the presence of cervical lymphadenopathy, large size >4 cm [55], and fixation of the nodule to adjacent tissues [7]. Vocal fold immobility is not always adequately assessed by patient’s voice, and flexible laryngoscopy may be advised in cases of high suspicion of vocal fold tumor invasion [56]. Neck tenderness appreciated on examination should also raise the concern for acute or subacute thyroiditis.
Physical exam, on the other hand, may be limited by the patient’s body habitus and the experience of the clinician on neck palpation, such that obtaining thyroid US becomes an important step in the diagnostic evaluation of these patients [57].
Laboratory Investigation
All patients with a thyroid nodule should have a serum TSH level measured. A serum calcitonin level should be obtained in patients with a family history of medullary thyroid cancer or multiple endocrine neoplasia (MEN) types 2a or 2b, pheochromocytoma, or hyperparathyroidism [58, 59]. An antimicrosomal antibody titer (anti-TPO) should be obtained in patients with an elevated serum TSH level to make a diagnosis of Hashimoto’s thyroiditis. In addition, in cases of malignant thyroid nodules, studies have shown that increased levels of TSH are associated with increased likelihood of thyroid cancer and may also be seen in more advanced stages of differentiated thyroid cancer [60, 61].
Patients with suppressed serum TSH levels should have free T4 and total T3 levels measured and an iodine I-123 thyroid scan performed to investigate whether the nodule is hyperfunctioning [62]. Because the risk of malignancy in hyperfunctioning nodules is very low (<1%), cytologic evaluation is unnecessary [48].
Thyroid Ultrasound
Ultrasonography is the imaging study of choice for the assessment of thyroid nodules. It is very helpful to evaluate the thyroid parenchyma (homogeneous or heterogeneous) and gland size, as well as the size, location, and sonographic characteristics of any nodule(s), to evaluate the presence or absence of cervical lymphadenopathy, and to provide accurate measurements of nodule size and volume for interval monitoring [48].
Ultrasonographic characteristics that are associated with an increased risk of malignancy include solid appearance, marked hypoechogenicity, the presence of internal microcalcifications, irregular margins (Fig. 11.6b, c), size >3 cm, increased internal vascularity , an absence of halo, and a shape that is taller than wide measured on a transverse view [27, 63]. Features with the highest specificity for thyroid cancer are microcalcifications, irregular margins, and tall shape [64]. The specificities of the aforementioned features for detecting thyroid cancer vary greatly, from 41 to 95%, but their sensitivities are consistently very low [27, 64, 65]. However, the probability of malignancy increases significantly when two or more suspicious criteria coexist [66].
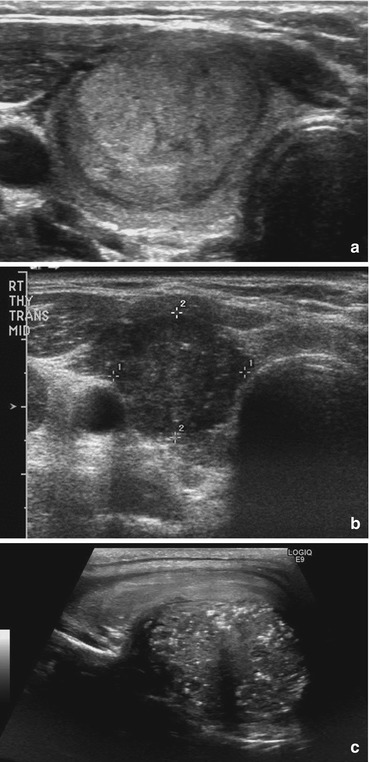
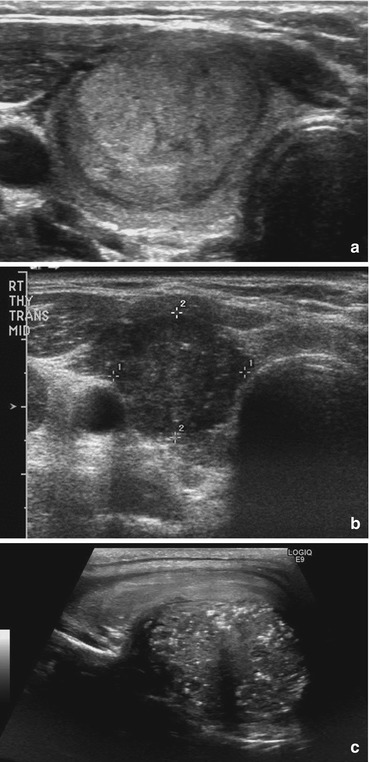
Fig. 11.6
(a) Classic sonographic image of a benign thyroid nodule. Note smooth and well-demarcated boarders and isoechogenicity. (b) Classic sonographic features of papillary thyroid cancer. Note hypoechogenicity, irregular margins. (c) Classic sonographic features of papillary thyroid cancer. Note hypoechogenicity, irregular margins, microcalcifications
Although the ATA recommends that a thyroid US be performed in all patients with a thyroid incidentaloma identified on CT, MRI, or FDG-PET [9], the Incidental Thyroid Findings Committee attempts to allow for some exemptions to the rule [15]. Patients with a thyroid incidentaloma and no suspicious CT or MRI findings (defined as normal lymph nodes and/or no invasion of local tissues by the thyroid nodule) that have (1) limited life expectancy due to comorbidities, (2) have a <1 cm nodule and are ≤35 years of age, and (3) have a <1.5 cm nodule and are ≥35 years of age may not necessarily require a diagnostic US, and a patient-centered approach and discussion are instead recommended by this organization. In several studies validating the application of the above criteria, a 35% decrease of the US-guided FNA procedures [47] with only a 1.2% missed incidental malignancies was noted [67].
Fine-Needle Aspiration (FNA) Biopsy
FNA is the most important study in the evaluation of an incidentally discovered thyroid nodule with suspicious sonographic features. Studies have reported lower rates of both nondiagnostic and false-negative cytology from FNA procedures performed using US guidance compared to palpation [68, 69]. Therefore, for nodules with a cystic component, or nonpalpable posteriorly located nodules that are at high risk for nondiagnostic or sampling error, respectively, a US-guided FNA biopsy should be performed [70]. Thyroid US has been widely used to stratify the risk of malignancy in thyroid nodules and to assist in decision-making about whether FNA is indicated. As a result, the pattern of sonographic features associated with a nodule confers a risk of malignancy and, combined with nodule size, guides FNA decision-making.
Most recent ATA guidelines recommend that only nodules ≥1 cm with a sonographic pattern of high or intermediate suspicion should be evaluated with FNA, since they have a greater potential to be clinically significant cancers [9]. Occasionally, however, there may be nodules smaller than 1 cm that require further evaluation because of the presence of worrisome clinical symptoms or associated cervical lymphadenopathy.
Although FNA for thyroid incidentalomas is a low-risk procedure, for some nonmalignant nodules, confirmation of a benign diagnosis may be difficult, e.g., inability of cytology to differentiate between follicular carcinoma and follicular adenoma [59]. This results in a substantial number of patients undergoing diagnostic surgical excision of benign nodules. In a retrospective study, 25–41% of patients who underwent FNA for thyroid incidentalomas proceeded to surgery, and in 36–75% of them, the nodules were benign [46, 63]. Of those who do not undergo surgery, a vast majority are referred for follow-up thyroid ultrasound.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree