Thrombophilic conditions are associated with an increased risk of venous thromboembolic events (VTE) during pregnancy. Thrombophilic disorders are either acquired, as in antiphospholipid syndrome, or inherited, as in factor V Leiden. Both are associated with VTE but acquired disorders can also increase the risk of arterial events. However, there is controversy as to whether they may adversely affect other pregnancy outcomes including pregnancy loss, placental abruption, severe preeclampsia, and stillbirth. This article discusses the effect of thrombophilias on pregnancy.
Thrombophilic conditions are associated with an increased risk of venous thromboembolic events (VTE) during pregnancy. Thrombophilic disorders are either acquired, as in antiphospholipid syndrome, or inherited, as in factor V Leiden. Both are associated with VTE but acquired disorders can also increase the risk of arterial events. However, there is controversy as to whether they may adversely affect other pregnancy outcomes including pregnancy loss, placental abruption, severe preeclampsia, and stillbirth. This article discusses the effect of thrombophilias on pregnancy.
Epidemiology and risks for VTE
The risk of having a thromboembolic event during pregnancy in the general population is approximately 200 per 100,0000 deliveries. The risk is higher during the postpartum period, with an incidence of approximately 500 per 100,000, with a clinical presentation of deep vein thrombosis (DVT) occurring more frequently than pulmonary embolism (PE). The risk seems to increase with age; it is 1.38-fold higher for women who are older than 35 years during their pregnancy. Many factors increase the risk of having a thromboembolic event, including having concomitant diseases such as systemic lupus erythematosus or sickle cell disease, obesity, postpartum complications, or the presence of an underlying thrombophilic disorder. Most thrombotic events are venous, with arterial clots accounting for 20%, which includes stroke and myocardial infarction. Most thrombotic events occur at the time of delivery, with one-third of DVTs and 50% of PEs occurring during the postpartum period. PE remains the leading cause of maternal death in developed countries and accounts for 20% of pregnancy-related deaths.
The reasons for the increased risk for VTE during pregnancy are multifactorial. The increases in hormone levels can decrease venous outflow from the lower extremities, and more venous thrombotic events occur in the left leg than the right because of mechanical issues; this is related to the course of the right iliac artery, which courses over, and can compress, the left iliac vein. There is also increased pressure over the pelvic veins from the gravid uterus. As with patients who are not pregnant, decreased mobility can also put a patient at increased risk of having a clotting event, as can a history of a prior thrombotic event or a history of smoking.
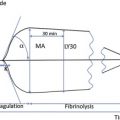
Pregnancy itself can also lead to hypercoagulability. Many hemostatic changes occur during pregnancy that can affect the normal clotting mechanisms.
The levels of many coagulation factors, including factor VII, factor VIII, factor X, von Willebrand factor, and fibrinogen, are increased, whereas free protein S is decreased. Other alterations include increased resistance to activated protein C in the second and third trimesters, and increased levels of fibrinolytic inhibitors including thrombin activatable fibrinolytic inhibitor (TAFI) and plasminogen activator inhibitor-1 and inhibitor-2 (PAI-1 and PAI-2). Although these changes may be essential for maintaining adequate hemostasis and preventing blood loss during delivery, they all potentially contribute to a hypercoagulable state, thereby increasing the risk of having a thromboembolic event during pregnancy that persists into the postpartum period.
There have been many studies of the factors that increase a patient’s risk of having a VTE during pregnancy. Patients who have had a previous VTE have a higher incidence of developing a second event compared with those without a past history of a clotting event. The highest risk during pregnancy occurs in women who have had a spontaneous clotting event in the past, with a recurrence rate of 10.9% during pregnancy. Although constant throughout pregnancy, the risk seems to be highest during the postpartum period. Apart from having a history of thrombosis, thrombophilia is the most important risk factor for developing thrombotic complications during pregnancy. Both acquired and inherited thrombophilias seem to increase the risk of having an event during pregnancy.
Inherited and acquired thrombophilias
Inherited Disorders
The inherited thrombophilias include deficiencies of the natural anticoagulant proteins, protein C, protein S, and antithrombin. Two gain-of-function mutations occur in genes encoding the procoagulant proteins, factor V and prothrombin. Factor V Leiden results from the replacement of arginine (Arg) by glutamine (Gln) at position 506 in the protein, leading to impaired inactivation of factor Va by activated protein C (ie, the phenomenon of activated protein C resistance). Prothrombin G20210A is a mutation in the 3′-nontranslated region of the prothrombin gene, and heterozygotes have approximately 30% higher plasma levels of prothrombin than noncarriers. Factor V Leiden is the most common genetic risk factor in pregnant women, occurring in up to 44% of those with a history of VTE. The prothrombin G20210A mutation is found in 17% of women with venous thrombosis during pregnancy. Heterozygosity for the factor V Leiden or prothrombin G20210A mutations are common in healthy white populations, with prevalence of about 5% and 2%, respectively. Because, in normal pregnancy, there is increased activated protein C resistance, the presence of the factor V Leiden abnormality worsens this phenomenon and likely accounts for the increased thrombotic diathesis.
More controversial than the inherited thrombotic disorders is homozygosity for the thermolabile variant (C677T) of 5,10-methylene tetrahydrofolate reductase (MTHFR). It is associated with higher levels of homocysteine in the general population and often occurs in individuals who have low folate levels. Homocysteine plays an essential role in the metabolism of vitamin B12 and folate. During pregnancy, it has been shown that homocysteine decreases with time. Recent data from many studies have suggested that there is no significant increase in VTE risk in individuals who harbor homozygous mutations in the MTHFR gene. For this reason, it is not usually considered when assessing a patient’s thrombotic risk, especially in light of the folate supplementation that is routine in pregnancy and offers a means of reducing homocysteine levels.
Acquired Disorders
An acquired disorder in pregnant women leading to thrombosis or pregnancy loss is antiphospholipid antibody. For a patient to be diagnosed with antiphospholipid syndrome, several criteria must be met. The clinical criteria include having had at least 1 arterial or venous thrombotic episode or pregnancy-associated morbidity. The latter include unexplained fetal loss after 10 weeks’ gestation; 1 or more premature births of a morphologically normal neonate before gestational age 34 weeks that results from eclampsia, preeclampsia, or placental insufficiency; or having had 3 or more unexplained miscarriages before the tenth week of gestation. There are also laboratory criteria that must be present to assign a diagnosis of antiphospholipid syndrome. These criteria include the presence of a lupus anticoagulant, increased levels of cardiolipin (immunoglobulin G or immunoglobulin M), or β 2 glycoprotein 1 antibodies. In order for the criteria to be met, lupus anticoagulant must be positive, or cardiolipin or β 2 glycoprotein 1 must be of medium or high titer on 2 or more laboratory blood draws at least 12 weeks apart.
Inherited and acquired thrombophilias
Inherited Disorders
The inherited thrombophilias include deficiencies of the natural anticoagulant proteins, protein C, protein S, and antithrombin. Two gain-of-function mutations occur in genes encoding the procoagulant proteins, factor V and prothrombin. Factor V Leiden results from the replacement of arginine (Arg) by glutamine (Gln) at position 506 in the protein, leading to impaired inactivation of factor Va by activated protein C (ie, the phenomenon of activated protein C resistance). Prothrombin G20210A is a mutation in the 3′-nontranslated region of the prothrombin gene, and heterozygotes have approximately 30% higher plasma levels of prothrombin than noncarriers. Factor V Leiden is the most common genetic risk factor in pregnant women, occurring in up to 44% of those with a history of VTE. The prothrombin G20210A mutation is found in 17% of women with venous thrombosis during pregnancy. Heterozygosity for the factor V Leiden or prothrombin G20210A mutations are common in healthy white populations, with prevalence of about 5% and 2%, respectively. Because, in normal pregnancy, there is increased activated protein C resistance, the presence of the factor V Leiden abnormality worsens this phenomenon and likely accounts for the increased thrombotic diathesis.
More controversial than the inherited thrombotic disorders is homozygosity for the thermolabile variant (C677T) of 5,10-methylene tetrahydrofolate reductase (MTHFR). It is associated with higher levels of homocysteine in the general population and often occurs in individuals who have low folate levels. Homocysteine plays an essential role in the metabolism of vitamin B12 and folate. During pregnancy, it has been shown that homocysteine decreases with time. Recent data from many studies have suggested that there is no significant increase in VTE risk in individuals who harbor homozygous mutations in the MTHFR gene. For this reason, it is not usually considered when assessing a patient’s thrombotic risk, especially in light of the folate supplementation that is routine in pregnancy and offers a means of reducing homocysteine levels.
Acquired Disorders
An acquired disorder in pregnant women leading to thrombosis or pregnancy loss is antiphospholipid antibody. For a patient to be diagnosed with antiphospholipid syndrome, several criteria must be met. The clinical criteria include having had at least 1 arterial or venous thrombotic episode or pregnancy-associated morbidity. The latter include unexplained fetal loss after 10 weeks’ gestation; 1 or more premature births of a morphologically normal neonate before gestational age 34 weeks that results from eclampsia, preeclampsia, or placental insufficiency; or having had 3 or more unexplained miscarriages before the tenth week of gestation. There are also laboratory criteria that must be present to assign a diagnosis of antiphospholipid syndrome. These criteria include the presence of a lupus anticoagulant, increased levels of cardiolipin (immunoglobulin G or immunoglobulin M), or β 2 glycoprotein 1 antibodies. In order for the criteria to be met, lupus anticoagulant must be positive, or cardiolipin or β 2 glycoprotein 1 must be of medium or high titer on 2 or more laboratory blood draws at least 12 weeks apart.
Thrombophilia and the risk of VTE during pregnancy
Either an acquired or inherited thrombophilia can be identified in 20% to 50% of white women who have a venous thromboembolic event during pregnancy or the postpartum period. To better understand the importance of thrombophilia in pregnancy, Robertson and colleagues conducted a systemic review of previously published studies evaluating the importance of thrombophilia in pregnancy-associated VTE. The risk seems to be greatest for those with homozygosity for the factor V Leiden mutation, with an odds ratio (OR) of 34.4. Heterozygosity for factor V Leiden confers an OR of 8.32. Mutations in the prothrombin gene are also highly associated with increased risk with homozygosity and heterozygosity being associated, with ORs of 26.3 and 6.8, respectively. The risk of having a venous thromboembolic event has been estimated to be 1:500 for those who are heterozygous for factor V Leiden, 1:200 for those who are heterozygous for prothrombin G20210A, and 4.6:100 for compound heterozygotes who carry the factor V Leiden and prothrombin gene mutations. The risk with protein C deficiency is 1:113 and 1:42 for antithrombin deficiency type 2 and 1:2.8 for antithrombin deficiency type I. Therefore, the women with the greatest risk are those who are homozygous for factor V Leiden, prothrombin, double heterozygous individuals, and those with antithrombin deficiency.
The acquired disorder of antiphospholipid antibody syndrome also has been associated with increased risk of VTE. Although there is still much controversy, it has been estimated that the OR is 15.8. Antiphospholipid antibodies are present in approximately 5% of pregnant women and in 37% of women who are pregnant and have systemic lupus erythematosus. One study found that the persistence of the increased cardiolipin antibodies was associated with the strongest association for an increased risk of pregnancy-related thrombotic events, although it is generally believed that the presence of a persistent lupus anticoagulant is a stronger risk factor.
Because the risk of having a thromboembolic event during pregnancy is still low in women with the most commonly encountered thrombophilic disorders, most women who harbor thrombophilias in the absence of a history of venous thromboembolism or fetal loss do not generally receive anticoagulation as a preventative measure. The women who gain the most benefit from antithrombotic prophylaxis before and after giving birth are those with a history of a prior thrombotic event.
Thrombophilias and pregnancy
There is concern that the thrombophilias can lead to adverse outcomes in pregnancy other than venous thromboembolism or fetal loss. Studies that have evaluated the risk of thrombophilias in adverse pregnancy outcome are difficult to interpret because of heterogeneity in study design, including issues with inclusion criteria, sample size, population selection, and diagnostic criteria. The disorders have been linked to poor obstetric outcomes in association with thrombophilia, including preeclampsia, placental abruption, intrauterine growth delay, and fetal loss.
Preeclampsia
In the general population, the incidence of preeclampsia has been estimated at 26 per 1000 births. There seems to be an even higher risk of preeclampsia and the associated conditions of severe preeclampsia and hypertension, increased liver function tests, low platelets (HELLP) syndrome in those with thrombophilia. One study found that 40% of women who develop preeclampsia harbor a thrombophilic defect. Meta-analyses have been performed to establish whether there is an association between thrombophilia and preeclampsia. However, it is difficult to interpret these results because there was significant statistical heterogeneity in the results of the different studies. Some studies did suggest an association. One large meta-analysis of the role of factor V Leiden in preeclampsia found that it was associated with an OR of 2.5 for severe hypertension during pregnancy. However, other studies were not able to confirm this observation. Studies of a link between the presence of the factor V Leiden mutation and preeclampsia have only found small differences in risk. Other studies have not consistently shown an association between preeclampsia and presence of mutations in prothrombin gene. However, there may be a role for hyperhomocysteinemia as an adverse risk factor for preeclampsia. Meta-analyses have also shown a link between preeclampsia and having either protein S or protein C deficiency, with ORs of 12.7 and 21.5, respectively. In general, it is unclear how to interpret these studies because many small studies were included in these analyses, which weakens the statistical significance of the analysis. In conclusion, it is believed that there is not a strong link between preeclampsia and thrombophilia.
Thrombophilia and Placental Abruption
There may be a link between the presence of thrombophilia and the occurrence of placental abruption. A study by Roque and colleagues established that there was a significant dose-dependent increased risk of abruption in those who carry thrombophilic conditions, with the highest risk established for those who carry a deficiency in antithrombin. The association between the prothrombin gene mutation and placental abruption is controversial, with one study suggesting an association based on meta-analyses but no clear-cut association by prospective cohort study. Hyperhomocysteinemia is believed to be associated with placental abruption based on a large cohort study and support from a meta-analysis study. These findings suggest an association between antithrombin deficiency and hyperhomocysteinemia as risk factors for placental abruption.
Pregnancy Outcome in Women with Thrombophilia
There is controversy as to whether there is an association between recurrent pregnancy loss in early as well as late pregnancy and the inherited thrombophilias. Two major studies provide an overview of the evidence linking pregnancy outcome and hypercoagulability. A meta-analysis by Rey and colleagues of 31 case-control, cohort, and cross-sectional studies found that there were some associations. Protein C and antithrombin deficiencies were not associated with fetal loss, whereas protein S was associated with late fetal loss that was not recurrent. Prothrombin gene mutation was linked to both early recurrent and late nonrecurrent loss. Factor V Leiden was also associated with loss throughout pregnancy in women with recurrent and nonrecurrent fetal loss. Meinardi and colleagues confirmed that women with factor V Leiden mutations have an increased incidence of fetal loss, whereas Tormene and colleagues did not find this. Other prospective studies have evaluated the association of the factor V Leiden and prothrombin gene mutations and with pregnancy. In one study that evaluated more than 5000 women, presence of factor V Leiden significantly increased the risk of stillbirth, with an ORs of 10.9. The same association was not found for early fetal loss and no clear role of the prothrombin gene mutation was identified in early or late fetal loss. Another study of more than 100 patients with pregnancy loss found that, of those who had had stillbirth, there was a significant association with either the factor V Leiden or prothrombin gene mutations. However, this result was not found for recurrent early pregnancy loss.
The only prospective and controlled study of thrombophilia and fetal loss was performed by the European Prospective Cohort on Thrombophilia (EPCOT) study, which showed no significant risk of fetal loss in women with thrombophilia in comparison with the general population. This study evaluated 843 women with thrombophilia , 571 of whom had 1524 pregnancies compared with 541 control women, 395 of whom had 1019 pregnancies. The rate of fetal loss was increased in women with thrombophilia (29 vs 23); however the OR was statistically significant only for stillbirth. Having multiple thrombophilic disorders was associated with a higher risk of stillbirths, with an OR of 14.3. There was a trend toward an increased risk of stillbirth or late fetal loss for all of the thrombophilias. However, for miscarriage, the only clear-cut association that emerged was for antithrombin deficiency.
Overall, carrying a thrombophilic condition increases the risk of having a late fetal loss or a stillbirth, but does not increase the risk of early pregnancy loss. These results were recently confirmed by a cohort study of more than 490 patients with thrombophilia who had suffered late pregnancy loss. In this study, the presence of 1 or more thrombophilic conditions was associated with an increased risk of pregnancy loss in the second and third trimester. This study also revealed that having a thrombophilic tendency protected patients from experiencing losses in the early stages of pregnancy.
There is also controversy as to whether the thrombophilias can lead to intrauterine growth delay and low birth weight infants, which is believed to be caused by altered oxygen distribution with low blood flow through the placental circulation. However, there does not seem to be a strong association between the presence of a thrombophilic disorder and fetal growth restriction. One meta-analysis specifically of the role of the factor V Leiden and prothrombin gene mutations and MTHFR homozygosity in intrauterine growth restriction, which included analyses of both case-control and cohort studies, found no evidence of any association between these disorders and growth restriction. Another study with a small sample size suggested that there may be an association between protein S deficiency and fetal growth delay, with an OR of 10.2, but wide confidence intervals reduced the study’s validity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree