Three-Dimensional Physics and Treatment Planning
Technological and computer developments have propelled radiation oncology into the three-dimensional conformal radiation therapy (3-D CRT) era.
Computed tomography (CT) and magnetic resonance imaging (MRI) provide a 3-D model of the patient’s anatomy and tumor, which allows radiation oncologists to more accurately prescribe irradiation to the target volume while sparing neighboring critical normal organs.
THREE-DIMENSIONAL TREATMENT PLANNING SYSTEMS
Conformational treatment methods were pioneered by Takahashi (34) in Japan; Proimos, Wright, and Trump in the United States (25, 35, 36); and Green, Jennings, and Christie in Great Britain (15, 16).
Computer-controlled radiation therapy was initiated by the work of Kijewski et al. (19) at the Harvard Medical School and Davy et al. (9, 10) at the Royal Free Hospital in London.
Sterling et al. (33) demonstrated the first 3-D approach to radiation treatment planning (RTP), using a computer-generated film loop technique that gave the illusion of a 3-D view of anatomic features and isodose distribution (two-dimensional [2-D] color washes) throughout a treatment volume.
McShan et al. (22, 30) implemented a clinically usable 3-D RTP system based on beam’s eye view (BEV), which provided the treatment planner with a viewing point from the perspective of the source of radiation, looking out along the axis of the radiation beam, similar to that obtained when viewing simulation radiographs.
Goitein and Abrams (13, 14) reported on a system that took advantage of CT scanning and interactive scan displays, increased minicomputer capabilities, produced high-quality color BEV displays, and computed and displayed radiographs from the digital CT data, called digitally reconstructed radiographs (DRRs).
CONFORMAL RADIATION THERAPY
The goal of 3-D CRT is to conform the prescription dose to the configuration of the target volumes while delivering lower doses to surrounding normal tissues.
Preplanning and Localization
After the proposed treatment position of the patient is determined, immobilization devices are fabricated in a CT simulator suite.
Radiopaque marks are placed on the patient’s skin, and the immobilization device is used for the volumetric 3-D planning CT study in the treatment position.
CT topograms are reviewed and patient alignment adjusted.
Computed Tomography Imaging for Three-Dimensional Planning
A volumetric planning CT scan is performed on the CT simulator with the patient in the treatment position, typically with 50 to 100 slices that are 2 to 8 mm thick (27).
CT images are transferred to a 3-D RTP or virtual simulation computer workstation via a computer network.
Critical Structure, Tumor, and Target Volume Delineation
The task of critical structure, tumor, and target volume delineation is performed by treatment planning staff and the radiation oncologist.
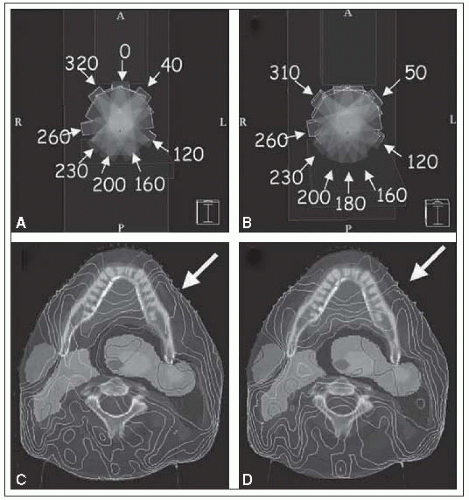
Most structures are contoured manually using a mouse or digitizer, although some structures with distinct boundaries (e.g., skin) can be contoured automatically (Fig. 3-1).
Many critical structures require the expertise of the radiation oncologist.
Consultation with a diagnostic radiologist is often helpful.
Designing Beams and Field Shaping
3-D RTP systems have the ability to simulate all treatment machine motions, including gantry angle, collimator width, length and angle, multileaf collimator (MLC) leaf settings, couch latitude, longitude, height, and angle, thus providing the capability to generate plans that involve nonaxial beams.
BEV display is used to select optimal beam directions and design beam apertures. This task is complemented by a room-view display, which is used to graphically set isocenter position and to better appreciate multiple-beam treatment techniques (27).
Dose Calculation
After the beam geometries are designed, the dose distribution is calculated throughout a defined 3-D volume with appropriate algorithms (28).
Plan Optimization and Evaluation
3-D CRT plans are typically optimized by iteratively changing beam directions and apertures and recalculating the dose distribution until an optimal plan is obtained.
Plans are evaluated qualitatively using dose-display tools, such as dose-volume histograms (DVHs); 2-D axial, sagittal, and coronal isodose sections; and 3-D room-view isodose surface displays.
If warranted, changes are made and the dose distribution recalculated and reevaluated; this process is repeated until the radiation oncologist approves the plan as meeting both target volume goals and normal tissue dose constraints (27).
Treatment Documentation
Once the treatment plan has been designed, evaluated, and approved, documentation for plan implementation is generated.
Documentation includes beam parameter settings, hard-copy block templates for block fabri-cation room or MLC parameters communicated over a network to the computer system that controls the MLC subsystem of the treatment machine (27), DRR generation and printing, and transfer of these documents to the medical record database.
Plan and Treatment Verification
Independent check of the treatment plan and monitor unit calculation by a physicist, radiographic verification simulation, first-day treatment portal films or electronic portal imaging devices, diode, TLD, or MOSFET in vivo dosimetry, and record-and-verify systems are used to confirm the validity and accuracy of the 3-D-based plan (27).
The elements of 3-D CRT are summarized in Figure 3-2.
VOLUME AND DOSE SPECIFICATION FOR THREE-DIMENSIONAL CONFORMAL RADIATION THERAPY
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree