Thoracic Malignancies
NON SMALL CELL LUNG CANCERS
Helena A. Yu
Mark G. Kris
Epidemiology
|
Etiology and Clinical Manifestations
Molecular Biology
EGFR Mt: 23% all pts, 43% never-smokers w/ADCL, L858R in exon 21 (40%) & exon 19 deletions (50%) confer EGFR TKI Sn, initially described in female Asian never-smokers but also present in smokers (J Clin Oncol 2011;29:2066), exon 20 insertions do not confer Sn to EGFR TKI, acquired T790M gatekeeper Mt confers EGFR TKI resistance (NEJM 2005;352:786)
ALK Rearrangements in 6%, various ALK fusion partners, a/w never/light smoking hx w/signet-ring ADCL histology, confers Sn to crizotinib (NEJM 2010;363:1693)
KRAS Mt: 25% of ADCL, a/w smoking (transversions: G12C, G12V) but present in 6% of never-smokers (transitions: G12D), confers EGFR TKI resistance (CCR 2008;14:5731)
Other aberrations in ADCL: BRAF Mt 3%, RET Fusions 1%, HER2 Amp/Mt 1%, PIK3CA Mt 3%, ROS1 Fusions 2%, may confer Sn to crizotinib, MET Amp 2% (JCO 2011;29:abstr 7506; JCO 2012;30:863; JCO 2012;30:4352)
Screening and Prevention
No mortality benefit for CXR & sputum cytology screening
Annual low-dose CT: 20% mortality benefit in Nat’l Lung Screening Trial, NNT = 320 (NEJM 2011;365;395)
Screening recommended: Ages 55-74, ≥30 pack y, quit <15 y ago w/annual low-dose CT
Smoking cessation: Most effective method of prev
High risk of second primary tumors in smokers – most commonly 2nd lung 1°, no evidence for chemoprevention w/retinoids, beta-carotene
Workup and Staging
Bx: Core needle preferred, send for histologic review w/IHC, molecular testing for all pts regardless of smoking status
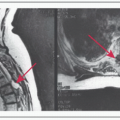
CT chest down to adrenals, bone scan or PET scan to evaluate for distant disease, MR brain for pts w/≥ stage IB disease, PFTs for symptomatic evaluation
Mediastinal evaluation: Recommended for nodes >1 cm on CT or PET+ via mediastinoscopy, EBUS-guided bronchoscopy or endoscopy w/LN bx
Stage I: Tumor ≤5 cm N0, Stage II: Tumor ≥5 cm N0, T1-2N1 (station ≥10; hilar/peribronchial nodes), T3N0, Stage IIIA: T3N1 or N2 (ipsilateral mediastinal nodes), T4N0-1, Stage IIIB: N3 (supraclavicular, scalene, contralateral mediastinal nodes), Stage IV: Contralateral pulmonary nodule (M1a), pleural involvement/effusion (M1a), distant disease (M1b)
Management: Stage I to Nonbulky IIIA (cT3N1) Disease
Surgery: Lobectomy preferred operation, preoperative FVC of >1.5 L required for lobectomy & >2 L for pneumonectomy
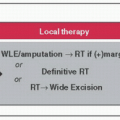
RT: For nonsurgical candidates, >60 Gy, can use standard RT, SBRT, radiofrequency ablation, good outcomes in early-stage disease
Adjuvant Chemo: ↑ OS for pathologic stage II-IIIA, CIS doublet for 4 cycles (LACE JCO 2008;26:3552), studies used CIS/vinorelbine, other doublets likely w/similar efficacy & ↑ tolerability, adjuvant TKIs: Erlotinib (EGFR-Mt) & crizotinib (ALK-fusion+) studies ongoing
PORT: Controversial, N2 nodes, +margins w/likely benefit
Management: Bulky Stage IIIA (cN2) to IIIB Disease
Induction: If resectable, chemo to best response followed by resection ± RT
Chemoradiation: Concurrent > sequential Rx (JCO 1999;17:2692) in unresectable stage III, regimens: CIS/etoposide, carboplatin/paclitaxel, CIS/vinorelbine
Pancoast tumor: ChemoRT → Sx (T3-4, N0-1), improves resectability, ↑ OS
Management: Metastatic Disease
Median OS: 6-mo BSC, 10-mo plat doublet, 12-mo plat doublet + Bev (NEJM 2006;355:2542), ↑ OS w/early palliative care (NEJM 2010;363:733), survival benefit w/doublet chemo in ECOG PS2 (JCO 2006;26:863)
1st-line Tx: RR ˜30%, standard is 4-6 cycles of plat doublet ± Bev (if eligible: No hemoptysis, non-SQCLC), doublet choice: CIS/peme (non-SQCLC) vs. CIS/GEM (SQCLC) (JCO 2008;26:3543), carboplatin/paclitaxel (any histology)
Continuation maintenance (d/c plat): Continue peme ↑ OS (PARAMOUNT Lancet Oncol 2012;13:247), peme + Bev ↑ PFS (AVAPERL), GEM ↑ PFS (JCO 2012;30:3516)
Switch maintenance (d/c plat doublet, switch to different agent): Peme (Lancet 2009;374:1432), erlotinib (SATURN), docetaxel (JCO 2009;27:591)
2nd-line Tx: RR ˜10%, doublet not better than single agent, docetaxel (JCO 2000;18:2095), GEM, 3rd-/4th-line options include vinorelbine, mitomycin/vinblastine
Targeted Therapy
EGFR TKIs (erlotinib): Rx of choice in EGFR-Mt, ↑ PFS, improved RR/PFS compared to plat doublet in 1st-line setting (IPASS NEJM 2010;362:2380), 2nd gen. TKIs (afatinib) in clinical trials, s/e: Rash (30-50% pts, Tx: Moisturizers, abx, topical steroids), diarrhea
Acquired resistance to EGFR TKIs (mechanisms: T790M Mt, MET Amp, SCLC transformation): Pts who d/c TKI may experience disease flare (CCR 2011;17:6298), many continue TKI, if chemo-naïve give plat doublet, clinical trial whenever possible, consider local tx if POD in single site
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree