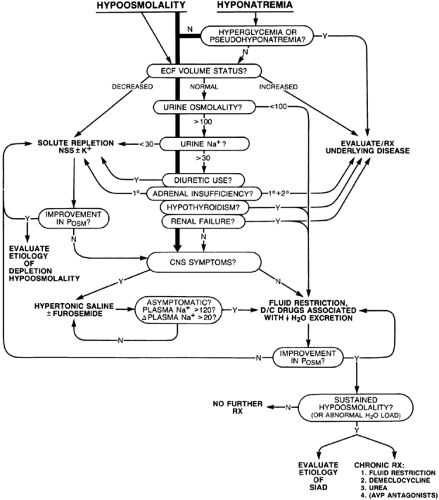
THERAPEUTIC APPROACH TO HYPOOSMOLALITY
Despite continuing controversy concerning the rapid correction of osmolality in hypoosmolar patients, relative consensus exists regarding appropriate treatment of this disorder (Fig. 27-4). Once true hypoosmolality is verified, the ECF volume status of the patient should be assessed by careful clinical examination. If fluid retention is present, the treatment of the underlying disease should take precedence over the correction of plasma osmolality. Often, this involves treatment with diuretics, which, by virtue of the excretion of hypotonic urine, should simultaneously improve serum tonicity. If any degree of hypovolemia is present, the patient must be considered to have depletion-induced hypoosmolality, in which case volume repletion with isotonic saline (0.9% sodium chloride) at a rate appropriate for the estimated volume depletion should be initiated immediately. If diuretic use is known or suspected, the isotonic saline should be supplemented with potassium (30 to 40 mEq/L), even if the serum [K+] is not low, because of the propensity of such patients to develop total body potassium depletion. Most often, the hypoosmolar patient is clinically euvolemic, in which case the evaluation should include the measurement of urine osmolality and [Na+]. Several situations dictate the reconsideration of solute depletion as a potential diagnosis, even in the patient without clinically apparent hypovolemia. These include a decreased urine [Na+], any history of recent diuretic use, and any suggestion of primary adrenal insufficiency. In fact, whenever a reasonable possibility of depletion-induced, rather than dilution-induced, hypoosmolality exists, the patient is most appropriately treated initially with isotonic saline, regardless of whether signs of hypovolemia are present. An improvement in and eventual correction of osmolality support a diagnosis of solute and volume depletion,24 although SIAD may also resolve spontaneously. If the patient has SIAD rather than solute depletion, no harm comes from administration of a limited amount (i.e., 1–2 L) of isotonic saline, because such patients simply excrete excess sodium chloride without a significant change in plasma osmolality.17
The approach to patients with SIAD varies according to the clinical situation. A patient who meets all essential criteria for the syndrome but has a low urine osmolality should be observed on a trial of modest fluid restriction. If the hypoosmolality is attributable to transient SIAD or severe polydipsia, the urine will remain dilute, and the plasma osmolality will be corrected as free water is excreted. If, however, the patient has the reset osmostat form of the disorder, then the urine will become concentrated at some point before the plasma osmolality and serum [Na+] return to normal ranges. If either primary or secondary adrenal insufficiency is suspected, glucocorticoid replacement should be initiated immediately after the completion of a rapid adrenocorticotropic hormone stimulation test. A prompt water diuresis after initiation of glucocorticoid treatment supports a diagnosis of glucocorticoid deficiency. However, the absence of a quick response does not necessarily negate this diagnosis because several days of glucocorticoid replacement are sometimes required for normalization of plasma osmolality. If hypothyroidism is suspected, thyroid function tests should be conducted and a serum thyroid-stimulating
hormone level should be obtained; usually, however, thyroid replacement therapy is withheld pending these results unless the patient is obviously myxedematous (see Chap. 45). The presence of renal failure in a patient with hypoosmolality generally requires a more extensive evaluation of renal function before treatment is initiated.
hormone level should be obtained; usually, however, thyroid replacement therapy is withheld pending these results unless the patient is obviously myxedematous (see Chap. 45). The presence of renal failure in a patient with hypoosmolality generally requires a more extensive evaluation of renal function before treatment is initiated.
ACUTE TREATMENT OF HYPOOSMOLALITY
In any significantly hypoosmolar patient, one is immediately faced with the question of how quickly the plasma osmolality should be corrected. Although hyponatremia is associated with a broad spectrum of neurologic symptoms,4 sometimes leading to death in severe cases,43,44 too rapid correction of severe hyponatremia can produce pontine and extrapontine myelinolysis, a brain demyelinating disease that also can cause substantial neurologic morbidity and mortality.46,47 Furthermore, some studies have suggested that the morbidity and mortality associated with even symptomatic hyponatremia may not be as high as previously thought.48 Reviews of clinical and experimental results have suggested that optimal treatment of hyponatremic patients must, therefore, entail balancing the risks of hyponatremia against the risks of correction for each patient.42,49,50,51 and 52 Although individual variability in response remains great, and consequently which patients will develop neurologic complications from either hyponatremia or its correction cannot always be accurately predicted, consensus guidelines for treating hypoosmolar patients allow a rational approach that minimizes the risks of both these complications. Implicit in these guidelines is the concept that treatment must be tailored to the patient’s clinical presentation: appropriate therapy for one patient may be inappropriate for another patient despite equivalent degrees of hypoosmolality.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree