As we have highlighted in the other cases, the clinical management of catecholamine-secreting pheochromocytomas or paragangliomas (PPGLs) can be very challenging—both diagnostically and therapeutically. However, when PPGL is diagnosed in the setting of pregnancy, the complexity rises 10-fold. Herein we share a case of a patient in whom the pheochromocytoma was diagnosed peripartum. In addition, a positive family history of pheochromocytoma but negative genetic testing led to an unexpected discovery.
Case Report
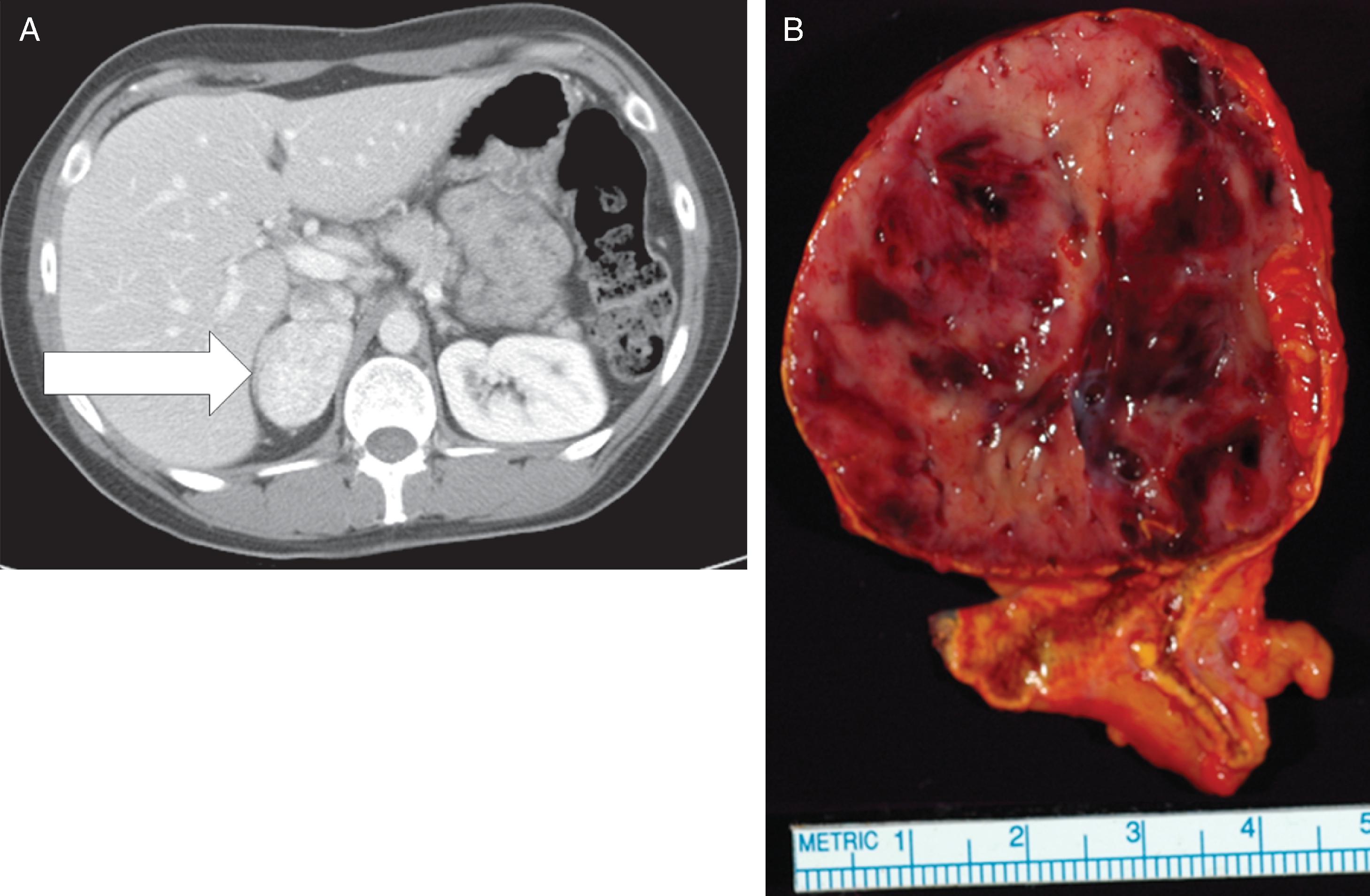
This 32-year-old woman had no history of hypertension or diabetes before her recent first pregnancy. She was noted to have hyperglycemia in the first trimester and abnormal liver function tests in the third trimester. The finding of abnormal liver function tests led to a decision to induce labor. During induction, her blood pressure rose to 180/90–100 mmHg. Labor lasted 24 hours, and her blood pressure was elevated throughout and treated with magnesium sulfate. Her baby boy’s delivery was complicated by pneumothorax and hypoglycemia, and he was kept in the neonatal intensive care unit for 5 days. Treatment of the mother’s hypertension with magnesium sulfate was continued for 24 hours after delivery. However, she developed fast and forceful palpitations, headache, and nausea, and the poorly controlled hypertension persisted. Because of nausea and emesis she was treated with metoclopramide. Shortly after receiving metoclopramide, she had a sense of impending doom and was diffusely diaphoretic. An electrocardiogram showed findings consistent with acute myocardial infarction. She was transferred from the obstetric floor to the coronary care unit, where an echocardiogram showed an ejection fraction of 45% and hypokinesis of the cardiac apex. Troponin I was elevated at 10 ng/mL (normal, <0.04 ng/mL). Coronary angiogram showed normal coronary arteries. Treatment with carvedilol was initiated. While in the coronary care unit, she mentioned that some family members had been diagnosed with pheochromocytoma in the past; this triggered a 24-hour urine collection for fractionated metanephrines and catecholamines, which showed: norepinephrine 1555 mcg (normal, <80 mcg) and normetanephrine 13,000 mcg (normal, <900 mcg). Treatment with phenoxybenzamine was initiated, and computed tomography of the abdomen detected a 4.5-cm right adrenal mass ( Fig. 96.1 ), and she was referred to Mayo Clinic at 5 weeks postpartum. With the addition of phenoxybenzamine (10 mg twice daily), her blood pressure averaged 100/60 mmHg.
Her family history was remarkable. Her paternal grandfather died at age 47 after returning from World War II with hypertension and a known pheochromocytoma. Her paternal aunt had a pheochromocytoma removed at 38 years of age. A cousin (offspring of her paternal aunt) had a pheochromocytoma removed at 18 years of age. In addition, three children of her paternal grandfather’s brother had pheochromocytoma. There was no family history of medullary thyroid carcinoma, hyperparathyroidism, cerebellar tumors, spinal cord tumors, retinal angiomas, pancreatic tumors, kidney tumors, neurofibromas, or any other familial neoplasms. Her father had a history of hypertension and coronary artery disease but had not been screened for pheochromocytoma. Our patient had two brothers and one sister and none had been screened for pheochromocytoma.
Her medications included phenoxybenzamine, 10 mg twice daily, and carvedilol, 6.25 mg twice daily. On physical examination her body mass index was 24.1 kg/m 2 , blood pressure 102/67 mmHg, and heart rate 100 beats per minute. The retinal examination was normal, and no Lisch nodules were evident on examination of the iris bilaterally. The thyroid gland was normal to palpation. Examination of the skin was normal, with absence of café au lait spots, axillary or inguinal freckling, and subcutaneous neurofibromas.
INVESTIGATIONS
Laboratory studies at Mayo Clinic reconfirmed a noradrenergic catecholamine-secreting tumor ( Table 96.1 ). The echocardiogram was normal with no regional wall motion abnormalities, and the ejection fraction was normal at 61%. The exercise sestamibi study was normal with no evidence of provokable ischemia.
| Biochemical Test | Result | Reference Range |
| Sodium, mmol/L Potassium, mmol/L Creatinine, mg/dL Plasma metanephrine, nmol/L Plasma normetanephrine, nmol/L 24-Hour urine: Metanephrine, mcg Normetanephrine, mcg Norepinephrine, mcg Epinephrine, mcg Dopamine, mcg | 140 4.3 0.9 <0.2 28.6 117 8760 781 2.4 197 | 135–145 3.6–5.2 0.7–1.2 <0.5 <0.9 <400 <900 <80 <20 <400 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree