The Male and Female Reproductive System in Hypothyroidism
Gerasimos E. Krassas
Nikolaos E. Pontikides
Hypothyroidism affects the reproductive system in women more than in men. Clinicians have long recognized that thyroid diseases in general and hypothyroidism in particular in premenopausal women are often associated with menstrual abnormalities. In men, whether induced or spontaneous, affects the male reproductive tract in a number of ways, depending in part on the age at onset. A review of the physiology of the male reproductive system from fetal to adult life is given in Chapter 27.
Reproductive Effects of Hypothyroidism in Males
Animal Studies
Hypothyroidism, induced or occurring soon after birth was associated with marked sexual maturation and development delays in animals (1). Rats made hypothyroid transiently by propylthiouracil (PTU) administration (from birth to 24 to 26 days of age) showed a decrease in testicular size, retardation in Sertoli cell differentiation, and prolongation of Sertoli cell proliferation time (2,3). When the rats became older and returned to a euthyroid status, there was an increase in testis size, Sertoli cell number, and sperm production (4). In one interventional study Hardy et al. (5) administered PTU to suckling rat pups from birth through day 24 postpartum as a 0.1% solution in the mothers’ drinking water. When the PTU tested pups became adults there was an increase in testis size and sperm production by about 80% and 140%, respectively, without affecting peripheral testosterone levels (5). In other studies in which experimental hypothyroidism in rats were left untreated for more than one month, there was an arrest of sexual maturity as well as an absence of libido and ejaculate. The longer the hypothyroidism persisted, the greater the damage to the testes (6). Induction of hypothyroidism in mature male rats had little effect on the histopathology of the testes, spermatogenesis, or serum testosterone concentrations (7). In the adult ram, hypothyroidism was associated with decreased testosterone concentrations but normal spermatogenesis (8). It would therefore appear that hypothyroidism affects the immature – but not the mature – testis.
Jiang et al. (9) conducted a study to determine whether hypothyroidism in adult male rats induced infertility by impairing sexual behavior or testicular function, whether infertility could be reversed by thyroxine (T4) treatment, and whether mutant rats could be produced by infertile rats via in vitro fertilization (IVF). The results showed that infertility resulted from both defective sexual behavior and testicular dysfunction; no untreated rats mated; the weights of epididymides were significantly reduced, whereas testes weights were not different from those of normal rats. Moreover, no fertilization was detected in vivo or in vitro. After T4 administration, which produced markedly increased serum T4 levels, the weights of the epididymides and testes increased markedly and there was partial reversion of the impaired sexual behavior. When determined both in vivo and in vitro, sperm fertility characteristics were entirely normalized and homozygous embryos developed to term after transfer without viability loss (9).
Table 41.1 Hormonal Changes in Male and Female Patients with Hypothyroidism | ||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||
Pekary and Sattin (10) treated young adult Sprague–Dawley male rats for one week with daily intraperitoneal saline injections, T4 (5 μg), PTU (3 mg), or castration to investigate the hypothesis that thyrotropin-releasing hormone (TRH) and TRH-derived peptides may contribute to the behavioral and mood changes accompanying hypothyroidism, thyrotoxicosis, and hypogonadism. The results showed that both hypothyroidism and castration reduced TRH levels as well as a majority
of other TRH-like peptides in the entorhinal cortex. Rats made hypothyroid had subnormal growth hormone mRNA (GH-mRNA) in their pituitary glands (11,12). The promoter of the rat GH gene has been documented to contain a thyroid hormone response element (13,14,15). This important finding provides a possible clue to the mechanism by which thyroid hormone interacts with the GH genes to correct GH secretion deficiency that is common in patients with primary hypothyroidism.
of other TRH-like peptides in the entorhinal cortex. Rats made hypothyroid had subnormal growth hormone mRNA (GH-mRNA) in their pituitary glands (11,12). The promoter of the rat GH gene has been documented to contain a thyroid hormone response element (13,14,15). This important finding provides a possible clue to the mechanism by which thyroid hormone interacts with the GH genes to correct GH secretion deficiency that is common in patients with primary hypothyroidism.
Human Studies
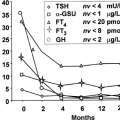
Hormonal Changes
Hypothyroidism is less common in men than in women and has less clear-cut effects on reproductive function (16,17,18,19,20,21,22). Primary hypothyroidism results in a decrease in sex hormone–binding globulin (SHBG) and total testosterone (T) concentrations, and free T concentrations are reduced in approximately 60% of males with hypothyroidism (Table 41.1). In a prospective study of 10 men with primary hypothyroidism, plasma free T levels were low and increased after the onset of levothyroxine (LT4) therapy (23). It has been reported that thyroid hormone administration to hypothyroid men induces a rise in both SHBG and total serum T (24). Boys with congenital hypothyroidism (CH) diagnosed and treated soon after birth have normal sexual development and adult height, indicating that treated CH does not produce long-term detrimental effects on gonadal function (25).
Although prolactin (PRL) elevation is the common link between primary hypothyroidism and gonadal dysfunction in females, males with primary hypothyroidism seldom exhibit elevated serum PRL concentrations, except those with long-standing and severe hypothyroidism. Severe primary hypothyroidism may result in pituitary tumors in men with hyperprolactinemia and hypogonadotropic hypogonadism. Replacement therapy with thyroid hormone reverses these abnormalities (26,27,28). A mechanism for hypogonadism associated with primary hypothyroidism without PRL elevation has been sought after. Most studies indicate that hypothyroid men with hypogonadism have normal luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels, suggesting that the primary defect is not in the Leydig cells and presumably results from a defect at the hypothalamus and/or pituitary level. Blunted gonadotropin (Gn) responses to Gn-releasing hormone (GnRH) support this notion, and it is likely, therefore, that primary hypothyroidism impairs the ability of the pituitary gland to respond to GnRH (29). Another finding that supports the above notion is that human chorionic gonadotropin (hCG) produces an exaggerated response of serum T in these patients, which is in contrast with what is expected if the primary defect was in Leydig cells. The latter may also be explained in part from the impaired clearance of hormones and drugs with which hypothyroidism is associated (30,31). The net consequence of an impaired hypothalamic–pituitary–gonadal axis is that free T levels may be subnormal in men with primary hypothyroidism.
Dehydroepiandrosterone (DHEA), DHEA-sulfate (DHEA-S), estrogenic metabolites of DHEA (androstenediol and its sulfate) and pregnenolone sulfate are decreased in the serum of men with hypothyroidism, compared to normal controls (32) (Table 41.1).
Hypothyroidism is associated with a variety of endocrine disorders depending on the age and severity of primary hypothyroidism (33,34,35). In children, hypothyroidism is associated with growth retardation and alterations in GH secretion and action (34). Hyposecretion of adrenocorticotropin (ACTH) and cortisol have also been reported in primary hypothyroidism, although cortisol levels remain normal (23,33,36,37). The discrepancy between serum cortisol concentrations and its secretion rate has been attributed to diminished cortisol clearance (34). Both provocative tests and sleep-induced GH secretion have been reported to be subnormal in male patients with primary hypothyroidism and are reversible by thyroid hormone replacement (34,38). Primary hypothyroidism produces delayed or precocious puberty in pre-pubertal boys and hypogonadism in post-pubertal individuals (38). As mentioned above, boys with CH do not show impaired adult height or sexual development when they have been treated with LT4 since the neonatal period (26).
Effects of Hypothyroidism in Early Life
CH is not associated with abnormal development of the male reproductive tract (1). This is not surprising because small but adequate amounts of maternal thyroid hormones cross the placenta to satisfy fetal demands (39). Maternal hypothyroidism during pregnancy and cretinism are also not associated with abnormal male reproductive tract development (40).
When adequately treated with LT4, boys with CH progress through puberty normally and at the appropriate time (25,41). Untreated hypothyroidism in early childhood can result in delay in sexual maturation, which can be reversed by thyroid hormone therapy (42). It has been known for many years that severe juvenile hypothyroidism is associated with precocious pseudopuberty (1,43). External genitalia develop early, but without axillary or pubic hair, and there is often macro-orchidism (44). The serum Gns are usually normal, and serum T is in the pre-pubertal range. It is proposed that cross-reactivity of TSH with the FSH receptor may be responsible for this rare phenomenon (45).
When adequately treated with LT4, boys with CH progress through puberty normally and at the appropriate time (25,41). Untreated hypothyroidism in early childhood can result in delay in sexual maturation, which can be reversed by thyroid hormone therapy (42). It has been known for many years that severe juvenile hypothyroidism is associated with precocious pseudopuberty (1,43). External genitalia develop early, but without axillary or pubic hair, and there is often macro-orchidism (44). The serum Gns are usually normal, and serum T is in the pre-pubertal range. It is proposed that cross-reactivity of TSH with the FSH receptor may be responsible for this rare phenomenon (45).
Sexual Dysfunction, Spermatogenesis, Fertility, and Hypothyroidism
Hypothyroidism is associated with decreased libido or impotence (16,46). In the studies by Carani et al. (47) and Krassas et al. (48) sexual behavior was also investigated in males with hypothyroidism, both before and after thyroid hormone treatment. In the Carani study (47), 14 adult hypothyroid males showed an overall 64% prevalence for hypoactive sexual desire (HSD), delayed ejaculation (DE) and erectile dysfunction (ED), and 7% for premature ejaculation (PE). After euthyroidism was restored, half of the patients with DE had no complaints, ED almost disappeared, and patients with HSD found a significant improvement in symptoms while on therapy. In the Krassas study (48), 44 hypothyroid patients and 71 controls were investigated with the Sexual Health Inventory for Males (SHIM) questionnaire. A global score between 25 and 22 was considered normal, between 21 and 11 was indicative of mild to moderately severe ED, and 10 or less was diagnostic of severe ED. Thirty-seven of 44 (84%) hypothyroid patients had an SHIM score of 21 or less, compared with only 24 of 71 controls (33.8%; p < 0.0001). Thirteen patients (35.1%) with ED had SHIM score of 10 or less, indicative of severe ED, compared with only 6 (25%) controls (p < 0.01). Negative correlations were found between the SHIM scores and serum TSH levels (p < 0.001). After treatment of hypothyroidism, a significant increase in SHIM scores was noted. As in thyrotoxicosis in males, the conclusion of this was that ED was also common in hypothyroid males and that treatment restored normal erectile function, indicating again that screening for thyroid dysfunction is recommended in all men presenting with ED.
Little is known of the effects of hypothyroidism on human spermatogenesis and fertility. Griboff (49) investigated five patients with primary hypothyroidism (aged 30 to 64 years) and, whereas all patients demonstrated normal sperm counts, semen exposure to room air revealed a rapid drying of the material and sperm motility loss in two of the five specimens. De la Balze et al. (50) investigated six adult hypothyroid men (aged 17 to 59 years) and reported that all patients demonstrated features of hypogonadotropic hypogonadism, with testicular biopsies revealing histologic abnormalities. Thyroid insufficiency had occurred before puberty in five of the men, whereas it occurred during childhood in the sixth patient. It was concluded that severe and prolonged thyroid insufficiency occurring early in life resulted in moderate failure of pituitary Gns secretion and abnormal testicular biopsies.
Wortsman et al. (51) investigated eight hypothyroid men aged 37 to 77 years. All patients had evidence of hypogonadism; five were hypergonadotropic, and three hypogonadotropic. Seven patients had various degrees of testicular atrophy, but sperm analysis was not performed. Serum T and SHBG concentrations were low in four patients. The authors concluded that abnormalities in gonadal function were common in men with primary hypothyroidism. Corrales Hernández et al. (52) studied spermatogenesis in 10 hypothyroid patients treated with LT4, in whom hypothyroidism was re-induced by discontinuing (or decreasing) the daily LT4 dose over at least one spermatogenic cycle. A decrease in seminal volume, progressive spermatozoa forward motility and cumulative percentage of mobile spermatozoa forms was observed. No abnormality in sperm density or the percentage spermatozoa with normal morphology was observed. Re-induction of hypothyroidism did not lead to seminal changes, when compared with the same patients when euthyroid. Serum concentrations of T and Gns were normal during the hypothyroid phase. It appears, therefore, that short-term post-pubertal hypothyroidism does not cause seminal alterations of sufficient intensity to impair male fertility. Jaya Kumar et al. (53) studied reproductive and endocrine function in eight males with primary hypothyroidism during the hypothyroid phase and again after achieving euthyroidism with LT4. The authors found high mean Gn levels, low serum T, low SHBG and subnormal T responses to hCG. Semen analysis was performed in five patients; results were not reported, but the authors claimed that “some improvement in sperm count and motility was observed”.
The effects of hypothyroidism on male spermatogenesis were investigated in a recent prospective, controlled study. A total of 25 hypothyroid men and 15 normal individuals were investigated, with semen analysis, fructose and acid phosphatase measurements, teratozoospermia index (TZI) and acridine orange test determined both before and 6 to 9 months after treatment with LT4 (54). The conclusion was that hypothyroidism had an adverse effect on human spermatogenesis, with sperm morphology the only parameter that was significantly affected. Screening for thyroid dysfunction in males who present with a defect in spermatogenesis is strongly advised and, when hypothyroidism is diagnosed, response to thyroid hormone should be evaluated before initiating other treatments. Characteristics on the quality of semen in patients with hypothyroidism are presented in Table 41.2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree