THE INCIDENTAL ADRENAL MASS
D. Lynn Loriaux
An unanticipated adrenal mass is found in ˜4% of upper abdominal computed tomographic (CT) scans (see Chap. 88 and Chap. 89). There are 100,000 such scans done annually. Thus, the consultation for an incidentally discovered adrenal mass is an important one for the endocrinologist. The primary questions posed in the consultation are two: What is the possibility that the mass is a primary adrenal cancer, and should the mass be surgically removed? The first question can be answered with some certainty. The one piece of “hard” data concerning this question is the known incidence of adrenocortical cancer, ˜1 in 600,000 per year.1 This number is taken from “pre-incidentaloma” registries and is based on criteria that ensure malignant behavior. If we assume a 3-year “preclinical” life, the prevalence of adrenocortical cancer can be estimated at 1 in 200,000. Let us assume, further, that all of these tumors will be found by the usual upper abdominal CT scan. Thus, if 200,000 people are scanned, 8000 nodules will be found, of which 1 will be a primary adrenal malignancy, a prevalence of 0.01%. In other words, the possibility that an “incidental” adrenal mass is a primary adrenal cancer is very small. Some series, however, report an incidence of adrenal cancer in incidental adrenal masses as high as 7%.2,3 This means that 560 of the 8000 nodules would have the pathologic diagnosis of adrenal cancer, and only 1 would exhibit the clinical behavior of an adrenal cancer. Many of these nodules are removed by surgeons, are misdiagnosed by the pathologist as cancer, and, since they are in fact benign, do not recur—a cancer “pseudocure.” It is this fact that introduces most of the confusion that bedevils the management of these patients.
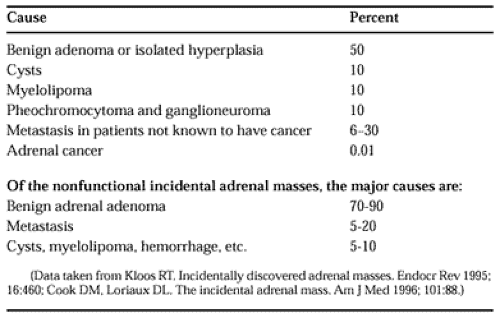
The causes of an incidental adrenal mass are shown in Table 84-1. Three surprises emerge from a study of these data: the high frequency of metastatic lesions to the adrenal gland that “present” as an incidental finding, the high percentage of pheochromocytomas in this group of patients, and, as previously noted, the extreme rarity of adrenocortical cancer.
Thus, the major challenge for the clinician managing these patients is to identify, with certainty, metastases to the adrenal gland and pheochromocytomas, and to develop a plan for following the remaining nodules of adrenal origin, including the identification of infectious causes of adrenal enlargement that need treatment, such as tuberculosis. A decision tree for the management of these patients is shown in Figure 84-1.
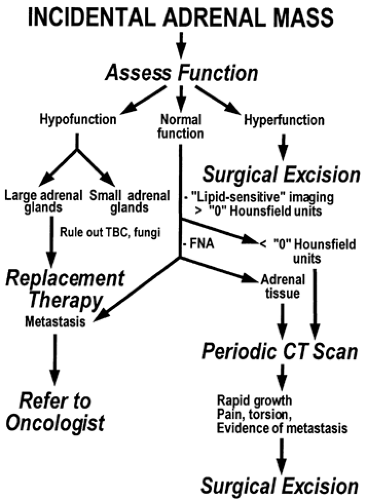 FIGURE 84-1. Decision tree for the management of patients with an incidentally discovered adrenal mass. (TBC, tuberculosis; CT, computed tomographic.) |
The functional capacity of the lesion should be assessed first; it should be assessed clinically and biochemically. Signs and symptoms of glucocorticoid and mineralocorticoid excess or deficiency, and symptoms of androgen excess in women and estrogen excess in men, should be sought out. The author’s choices for supporting laboratory tests are shown in Table 84-2. There are many variations on this theme, and most can be defended. In the opinion of the author, all patients should have a standard cosyntropin stimulation test (250 μg) with measurements
of cortisol, 17-hydroxyprogesterone, and fractionated urinary cate-cholamines. The remaining tests should be used if the clinical picture is strong enough to warrant a corroboration.
of cortisol, 17-hydroxyprogesterone, and fractionated urinary cate-cholamines. The remaining tests should be used if the clinical picture is strong enough to warrant a corroboration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree