The red blood cell indices
These will usually be haemoglobin (Hb), haematocrit (Hct) and RBC.
Hb is the oxygen-carrying protein in red blood cells (erythrocytes) and it can be used as a marker for surgical outcome. It can also be compared to other red cell indices, such as anaemia (Hb low). In addition, it can be used as a surrogate marker of renal insufficiency (low), blood loss (low), oxygen deprivation (high) or glucose in excess (HbA1C), and in genotyping for some sickle cell conditions.
The red blood cells transport oxygen, carbon dioxide and some nutrients between organs, and they have a lifespan of around 12 weeks. This is important when thinking about repeating or measuring an intervention. In a patient who is being treated for iron deficiency anaemia, there may therefore be little value in repeating the RBC before 12 weeks. If the patient is being corrected for a surgical intervention, because their Hb is too low or following blood loss, then cells called reticulocytes can be measured. Reticulocytes are ‘baby’ red blood cells and their profile increases to intervention for anaemia within a few days (compared to a few weeks for mature red blood cells).
Production of red blood cells is regulated by a biochemical process called erythropoiesis. This process is linked to tissue hypoxia (lack of oxygen) and driven by the hormone erythropoietin (EPO), which is produced by the kidney ( U&Es and renal anaemia). An elevated Hb and RBC are called polycythaemia. This is often caused by tissue hypoxia due to carbon monoxide or carbon dioxide, cigarette smoking, asthma or chronic obstructive pulmonary disease (COPD) or being at high altitude. Alternatively, high red cells may be seen in damage to the spleen (caused by trauma) or acute dehydration (relative rises). In practice, this normal physiological process is competing with disease pathologies and conditions. These are shown in the figure below, with the orange arrow representing COPD and the green arrow representing renal dysfunction.
U&Es and renal anaemia). An elevated Hb and RBC are called polycythaemia. This is often caused by tissue hypoxia due to carbon monoxide or carbon dioxide, cigarette smoking, asthma or chronic obstructive pulmonary disease (COPD) or being at high altitude. Alternatively, high red cells may be seen in damage to the spleen (caused by trauma) or acute dehydration (relative rises). In practice, this normal physiological process is competing with disease pathologies and conditions. These are shown in the figure below, with the orange arrow representing COPD and the green arrow representing renal dysfunction.
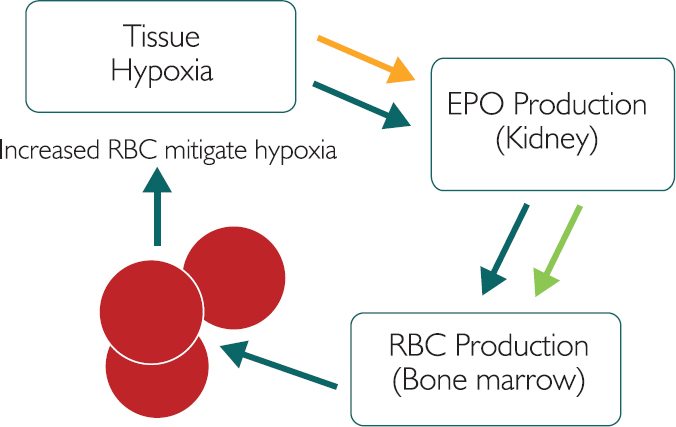
Figure 5.1: The process of erythropoiesis, with COPD and renal dysfunction
Considering the orange arrow, COPD causes narrowing of the airways and a subsequent fall in airflow. Bronchitis or emphysema (often caused by exposure to particulates such as cigarette smoke) is usually irreversible and leads to a lack of oxygen. This will usually cause hypoxia, which will result in increased EPO. EPO induces bone marrow production of red blood cells (erythropoiesis) and thus an increase in RBC. However, given the chronic, ongoing nature of COPD, this rise in RBC will not usually mitigate the hypoxia. COPD patients will often therefore have higher than normal RBC, which may present an increased risk of a cardiovascular event. Oxygen therapy may help to reduce or suppress the red blood cell production.
Considering the green arrow, overall renal function, as measured by estimated glomerular filtration rate (eGFR), generally falls by 10% per decade after the age of 35. Given this natural decline in renal performance, the kidney’s ability to sustain production of EPO is also reduced, leading to the renal anaemia seen in some elderly patients. EPO supplements may help to induce red blood cell production in these cases.
Anaemia
Anaemia means a reduced RBC (and Hb) and could indicate inability to sustain EPO ( U&Es), bone marrow insufficiency (leukaemia –
U&Es), bone marrow insufficiency (leukaemia –  white cell and platelets as described, see Table 3.1 above), blood loss or nutritional anaemia.
white cell and platelets as described, see Table 3.1 above), blood loss or nutritional anaemia.
Low Hb/RBC/lethargy could be anaemia, especially with normal white cell and platelet number, but what type of anaemia? Mean cell volume (MCV) can help identify the type of anaemia. MCV represents the average size of the red blood cells – big, small or normal.
Normal MCV (normocytic) means that the body can make red cells but it cannot keep them. This could suggest blood loss (due to menstruation, surgery or trauma, for example) but it can also be a surrogate marker of stomach ulcers or GI cancers.
Low MCV (microcytic) means that the body does not have the structural components needed to make red cells of the correct size. Storytelling: Imagine not having enough metal tent poles for your tent. The tent will not be the right size and will be small. This is usually due to an iron (Fe) deficiency, so consider tests for serum ferritin and total iron-binding capacity (TIBC). Possible causes of this could be Fe deficiency, sickle cell or thalassaemia.
High MCV (macrocytic) means that the body does not have enough nutritional components to make red cells of the correct size. Consider tests for either folate or B12 deficiency. Folate and B12 in this pathway provide ‘instructions’ for the cells by making accurate DNA. Storytelling: Imagine owning a new inflatable tent, which requires 75 litres of air to make it the right size. If the instructions have a misprint of 95 litres then more air is added and the tent will be bigger than expected. Possible causes of this could be liver disease, pregnancy, some antibiotics, and folate and B12 deficiency.
If folate is low, it could be due to dietary factors or a genetic defect in the enzyme (MTHFR) or some medications such as anti-cancer or epileptic drugs, or alcohol intake ( deranged LFTs). Alcohol can affect the stomach lining and reduce folate absorption. As red blood cells last for around 12 weeks, it would take sustained alcohol intake to change the entire RBC profile.
deranged LFTs). Alcohol can affect the stomach lining and reduce folate absorption. As red blood cells last for around 12 weeks, it would take sustained alcohol intake to change the entire RBC profile.
If B12 is low, it could be dietary or could be due to an autoimmune pernicious anaemia (PA), which can affect the stomach lining and reduce oral B12 absorption. A positive parietal cell and/or intrinsic factor antibody test can confirm PA. Given that oral absorption is restricted in PA, an intra-muscular B12 injection is usually required. Failure to correct B12 deficiency may lead to B12 neuropathy and demyelination because B12 is required to make the myelin sheath. If the myelin sheath is dysfunctional then nerve integrity is lost and neural and vascular retraction from the site (usually feet) will occur.  Patients who are positive for parietal cell or intrinsic factor antibodies may also be positive for anti-thyroid antibodies and have low T4 (thyroxine). A thyroid function test (TFT) may therefore be appropriate.
Patients who are positive for parietal cell or intrinsic factor antibodies may also be positive for anti-thyroid antibodies and have low T4 (thyroxine). A thyroid function test (TFT) may therefore be appropriate.
In summary, using the MCV test from the FBC can help to differentiate between microcytic, normocytic and macrocytic anaemia.
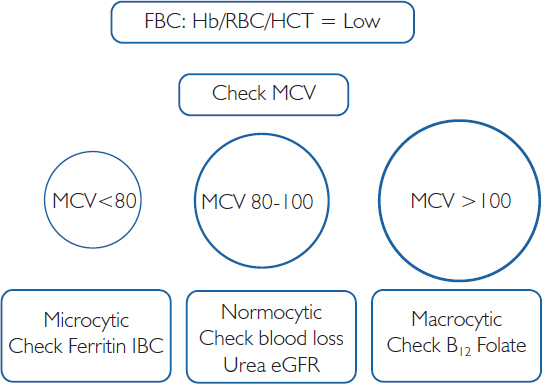
Figure 5.2: Patterns of Anaemia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree