deficiencies in iron, B12 and glucose); metabolic production ( production of cholesterol, CRP, fibrinogen (PT, INR, aPTT) and albumin); and detoxification of endogenous and exogenous toxins. Liver function tests (LFTs) will usually report enzymes, albumin and bilirubin levels. If the test name ends in ‘ase’ or has the units (IU/L) then it is an enzyme. An enzyme takes a substrate (usually not soluble and toxic) and converts it into a product (usually more soluble and less toxic).
production of cholesterol, CRP, fibrinogen (PT, INR, aPTT) and albumin); and detoxification of endogenous and exogenous toxins. Liver function tests (LFTs) will usually report enzymes, albumin and bilirubin levels. If the test name ends in ‘ase’ or has the units (IU/L) then it is an enzyme. An enzyme takes a substrate (usually not soluble and toxic) and converts it into a product (usually more soluble and less toxic).
Almost all enzymes are intracellular. The presence of high concentrations of enzymes in the blood means that cells have been destroyed, allowing the enzymes to ‘leak out’. Possible causes of cellular destruction could be trauma, alcoholic cirrhosis, viral damage from hepatitis, or cellular necrosis (cell death) resulting from drug toxicity. The particular enzymes raised will usually indicate which type of damage has occurred.
A standard LFT may contain:
•Bilirubin: Plumbing of the liver – pre-, actual, post- and red blood cell turnover
•Alanine aminotransferase (ALT): Viral hepatitis and drug toxicity – refer to British National Formulary (see Further Reading, page 103) and the pharmacy department in your local healthcare setting
•Aspartate aminotransferase (AST): Alcoholic hepatitis, acute liver failure
•Alkaline phosphatase (ALP or Alk Phos): The biliary tree, gall stones, pancreas
•Gamma-glutamyltransferase (GGT): Alcohol, analgesics and opiates
•Amylase: Pancreatitis
•Albumin: Decreased on liver failure
•International normalised ratio (INR): Now being used as a surrogate liver marker. In liver failure, fibrinogen production is compromised, and clotting time (INR) is therefore significantly extended.
As the liver is a dynamic and interconnected organ, the blood results from the LFT may be difficult to interpret when presented as a list on a results screen or printout. Instead, it may be helpful to imagine them superimposed onto a general anatomy and physiology diagram, and interconnected to other organs.
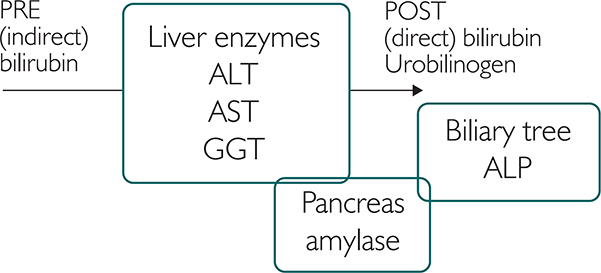
Figure 16.1: Liver enzymes
Bilirubin
Bilirubin is a breakdown product of red blood cells. Elevated bilirubin is called jaundice, and bilirubin is a marker of ‘plumbing’ in the liver. Pre-hepatic bilirubin is called indirect or unconjugated. In the liver an enzyme called UGT1A1 (which is dysfunctional in Gilbert’s syndrome) converts indirect bilirubin into direct, or conjugated bilirubin. The conjugated bilirubin is then partly used to produce urobilinogen and partly excreted in the faeces. The LFT result of ‘Total bilirubin’ is direct + indirect, both of which can also be measured to further investigate liver dysfunction. As indirect bilirubin rises, this is usually a pre- or actual hepatic condition; a rise in the direct form usually indicates a post-hepatic blockage.
Jaundice can occur when high levels of bilirubin are produced in polycythaemia ( full blood count and red blood cell count). High levels of bilirubin from the red cells overload the liver and may predispose the patient to jaundice. Jaundice can also be seen in actual liver damage, with high liver enzyme concentrations of aspartate aminotransferase (AST), alanine aminotransferase (ALT) and gamma-glutamyltransferase (GGT). Often bilirubin rises before the liver enzymes do. This may occur in patients undergoing chemotherapy, or those with hepatitis (both viral and alcoholic), or being treated with antibiotics or with some genetic conditions. In a post-hepatic blockage (with high Alk phos/amylase and raised liver enzymes) bilirubin will increase and this can be linked to the absence of urobilinogen.
full blood count and red blood cell count). High levels of bilirubin from the red cells overload the liver and may predispose the patient to jaundice. Jaundice can also be seen in actual liver damage, with high liver enzyme concentrations of aspartate aminotransferase (AST), alanine aminotransferase (ALT) and gamma-glutamyltransferase (GGT). Often bilirubin rises before the liver enzymes do. This may occur in patients undergoing chemotherapy, or those with hepatitis (both viral and alcoholic), or being treated with antibiotics or with some genetic conditions. In a post-hepatic blockage (with high Alk phos/amylase and raised liver enzymes) bilirubin will increase and this can be linked to the absence of urobilinogen.
Aminotransferases
Alanine aminotransferase (ALT) is found inside liver cells (see the earlier chapter on ways in which blood can change). Therefore, as the liver cells are damaged, the ALT will leak out and we can now measure it in the blood. ALT is a liver enzyme that closely reflects chronic and acute liver damage. It is often raised in viral hepatitis, drug toxicity or overdose.
Aspartate aminotransferase (AST) is a liver enzyme that indicates acute liver damage. It is often raised in alcoholic patients, due to severe liver damage. It can be used in conjunction with ALT to assess the extent of liver dysfunction.
In a raised ALT, you should ask the following:
•Is the value more than 1.5 x above the upper range?
•Is the patient symptomatic?
•Are bilirubin, INR and albumin also abnormal?
If the answer to any of these questions is ‘yes’, further investigations should be considered. If the answer is ‘no’, then consider repeating the test.
In the following examples, the upper reference range for AST is 40 IU/L and for ALT 40 IU/L. The figures used demonstrate which enzyme is raised, and should not be used as a diagnostic cut-off in practice. Some surgeries use a clinical decision limit protocol of 1.5x to 2x as the upper limit for defining group A. Assuming the patient is asymptomatic, hasn’t started a new medication, and the other liver markers are within a normal range, an ALT of less than 80 IU/L could perhaps be filed as a false positive.
Patient 1 has AST 100 IU/L and ALT 22 IU/L, and all other LFTs are normal. AST is also found in cardiac tissue so investigation of chest pain may reveal a cardiac event.
Patient 2 has ALT 100 IU/L and AST 48 IU/L, which could indicate viral hepatitis, toxicity to methotrexate, or over-use of analgesics.
Patient 3 is an alcoholic patient with severe liver damage. AST is 200 IU/L and ALT is 100 IU/L. If the AST was to increase to 500 IU/L the prognosis would become increasingly poor.
Patient 4 has obstetric cholestasis, presenting with pruritus (itch) and raised ALT. Bile salts are ordered. Bile salts are made by the liver and stored in the gall bladder; they are then secreted into the duodenum to dissolve fats (enterohepatic circulation). In hepatobiliary conditions, the enterohepatic circulation is dysfunctional and bile salts can be secreted into the systemic circulation. Given the lipid-dissolving, surfactant properties of bile salts, their presence in a pregnant patient’s systemic circulation could lead to foetal distress or damage.
Gamma-glutamyltransferase (GGT)
The enzyme gamma-glutamyltransferase (GGT) is often used as a marker for alcohol intake. GGT can be elevated for up to five days following alcohol intake. However,  full blood count (FBC) and the mean cell volume (MCV) because a raised GGT could be due to transient alcohol intake. A high GGT and a folate-deficient macrocytic anaemia, caused by alcohol intake, are more indicative of alcohol abuse. As this will take at least 6–12 weeks to develop, consider the red blood cell lifespan.
full blood count (FBC) and the mean cell volume (MCV) because a raised GGT could be due to transient alcohol intake. A high GGT and a folate-deficient macrocytic anaemia, caused by alcohol intake, are more indicative of alcohol abuse. As this will take at least 6–12 weeks to develop, consider the red blood cell lifespan.
Alkaline phosphatase
The enzyme alkaline phosphatase (Alk phos or ALP) is also present in other organs (bones, kidney and placenta) so  these tests, symptoms and history. Liver-specific Alk phos is an enzyme mainly found in the cells that line the bile ducts and biliary tree. Therefore ALP is usually elevated with bile duct blockage – caused by gall stones, pancreatitis, post-hepatic tumour or cholestasis.
these tests, symptoms and history. Liver-specific Alk phos is an enzyme mainly found in the cells that line the bile ducts and biliary tree. Therefore ALP is usually elevated with bile duct blockage – caused by gall stones, pancreatitis, post-hepatic tumour or cholestasis.
If ALP is raised and GGT is not, then consider a non-hepatic condition. If GGT is raised, and/or ALP is twice the upper range, and/or both ALP and GGT have been raised for more than three months, and/or the patient has symptoms, consider a liver ultrasound.
Amylase
The enzyme amylase is found in the pancreas and saliva. It is therefore often elevated in pancreatitis.
Patient 5 had a rise in amylase (pancreas), bilirubin (post-hepatic blockage) and Alk phos (biliary tree), followed by GGT, ALT and then AST (secondary liver damage), which represented the progression of a pancreatic tumour.
Albumin
Albumin is a protein made by the liver and has three main roles: as a chaperone (transporter) for molecules like calcium ( bone profile); to provide pressure and osmotic stability in the blood, and is thus linked to oedema and renal function (
bone profile); to provide pressure and osmotic stability in the blood, and is thus linked to oedema and renal function ( U&Es); and as a precursor for antibody production (globulins). Albumin can also be decreased in malnutrition, but other LFTs are likely to be normal. Since albumin is made by the liver, any dysfunction will probably reduce albumin concentrations (hypoalbuminaemia). However, you should check the U&Es as some renal dysfunction will not retain albumin, and proteins and cells are likely to be present in the urine.
U&Es); and as a precursor for antibody production (globulins). Albumin can also be decreased in malnutrition, but other LFTs are likely to be normal. Since albumin is made by the liver, any dysfunction will probably reduce albumin concentrations (hypoalbuminaemia). However, you should check the U&Es as some renal dysfunction will not retain albumin, and proteins and cells are likely to be present in the urine.
Alcohol and drug abuse, and viral infection
Patient 6 has raised aminotransferases (>300 IU/L), due to a viral infection and paracetamol overdose, in addition to an alcoholic liver disease.
As the viral infection becomes acute, this value may rise higher still. An AST >400 IU/L and a peak ALT of 1000 IU/L is associated with severe liver damage due to paracetamol overdose. For the hepatitis viral infection in practice, this can also be seen in the diagnosis of viral hepatitis. Hepatitis B surface antigen (HepBsAg) may indicate a current infection. Alternatively, a new, rapid technique is to measure the DNA or RNA of the HepB virus directly in the cell.
Patients who use cocaine, marijuana or heroin alone will usually have out-of-range LFTs, including AST and GGT. If injecting, a raised ALT may often indicate a viral hepatitis. If the patient is alcoholic (raised MCV and raised GGT), additional drug use will also affect these measures.
Storytelling: ALT: Imagine a car engine (the liver). The engine contains oil (ALT). If you notice some oil on the driveway under the car (ALT in the blood), then it’s likely that the oil has leaked out of the engine. The more oil has leaked out, the more damaged the engine is. Likewise, the more ALT there is in the blood, the more ALT must have leaked out of the liver cells. This is an example of cellular content. ALP: This enzyme is also found in the cells after they have been in the liver – any damage in the liver will make the ALP leak out into the blood. The ALP level can therefore give us information about a post-hepatic or obstructive jaundice. This is another example of cellular content. Bilirubin: When a red blood cell reaches the end of its lifespan, it is recycled and a single bilirubin molecule is released into the blood. These single bilirubin molecules are known as ‘unconjugated’ bilirubin. The liver has a 24 hour ‘dating agency’ which pairs up single bilirubin molecules. These paired bilirubin molecules are ‘conjugated’ and they are more easily excreted. We can find out if the patient has a pre- or post-hepatic jaundice by looking at the type of bilirubin. If this information isn’t available, we can look at associated tests. A pre-hepatic jaundice will usually also have raised red blood cells. An actual liver damage jaundice may have raised ALT and a post-hepatic jaundice may also have raised ALP.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree